Purpose
To measure the tear meniscus dynamics in aqueous tear deficiency dry eye patients using optical coherence tomography.
Design
Clinical research study of a laboratory technique.
Methods
Twenty-five aqueous tear deficiency dry eye patients and 30 healthy subjects were recruited. Upper and lower tear menisci of 1 randomly selected eye of each participant were imaged during normal and delayed blinking using optical coherence tomography. Measured parameters included upper tear meniscus height and volume, lower tear meniscus height and volume, the blink outcome defined as the meniscus volume change during blink action, and open eye outcome defined as the meniscus volume change during the open eye period.
Results
During normal blinking, both tear meniscus height and volume before blink in dry eye patients were significantly smaller than those in healthy subjects, except for the upper tear meniscus volume. During normal blinking, the blink outcome and open eye outcome of lower tear meniscus were significantly smaller in dry eye patients compared with healthy subjects. During delayed blinking, the upper and lower tear menisci heights and volumes significantly increased in both groups. However, dry eye patients had smaller increases than healthy subjects. During delayed blinking, the open eye outcomes of upper and lower tear menisci were smaller in dry eye patients than healthy subjects.
Conclusions
Dry eye patients seem to have reduced tear meniscus dynamics during normal blinking and smaller increases of meniscus volume during delayed blinking. Analysis of tear meniscus dynamics may provide more insight in the altered tear system in dry eye patients.
The tear system is dynamic, and blinking plays the important role of distributing the tears on the ocular surface so that physiologic equilibrium is maintained. Blinking redistributes the tears to the ocular surface from the tear menisci around both upper and lower eyelids, and it facilitates tear drainage. Blinking also may influence tear evaporation. Dynamic changes of the tear menisci are the result of the interaction between blinking and tears, which has been studied in normal subjects. In dry eye patients, lack of the tears may result in abnormal tear distribution on the ocular surface and irregular interaction during blinking. Distortion of the tear dynamics and the tear distribution on the ocular surface with each blink may contribute to ocular discomfort and dryness, which are the prevalent symptoms reported by dry eye patients with aqueous tear deficiency. The tear system has been evaluated in many studies by measuring tear breakup time, wetting of Schirmer strips, and determining lower tear meniscus dimensions in aqueous tear deficiency dry eye patients. However, tear meniscus dynamics during the blink cycle in dry eye patients remains untested, mainly because of the difficulty of real-time imaging in capturing the alterations of the tear system. Knowledge of these dynamics in dry eye patients may lead to a better understanding of the cause of the tear deficiency and its resulting damage to the ocular surface. In this study, we used real-time optical coherence tomography (OCT) to measure tear meniscus dynamics in aqueous tear deficiency dry eye patients.
Methods
Twenty-five clinically diagnosed aqueous tear deficiency dry eye patients (15 women and 10 men; mean age ± standard deviation, 49.6 ± 17.4 years) and 30 healthy subjects (17 women and 13 men; mean age ± standard deviation, 31.0 ± 8.4 years) were enrolled. Dry eye patients who reported ocular discomfort were evaluated and diagnosed at the Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, and the Department of Ophthalmology, University of Rochester. They had no ocular diseases except for dry eye, and no history of ophthalmic surgery and trauma. The patients were recruited into the aqueous tear deficiency dry eye group if they had a Schirmer I test score of less than 5 mm in 5 minutes, a tear breakup time of less than 10 seconds, no Meibomian glands or eyelid diseases as observed through a slit-lamp examination, and 1 or more of the dry eye symptoms in the questionnaire occurring at least often. The healthy subjects, serving as the control group, were recruited if they had no history of ocular discomfort, ocular diseases, or contact lens wear and had a Schirmer I test score of more than 10 mm.
The specification of the custom-built OCT instrument and the experimental procedure were described in previous studies. The repeatability of tear meniscus measurement with the OCT has been proved. In present study, central air conditioning and 2 humidifiers maintained the temperature at 15 to 25 C and the relative humidity at 30% to 50%. Ambient room light was used while imaging each subject. The subjects were evaluated by OCT after 10 am and were required not to use eye drops 24 hours before the visit. One randomly selected eye of each subject was tested. The custom-built OCT instrument with real-time scanning at 8 frames per second made 12-mm scans at the vertical meridian across the corneal apex. The subjects were asked to look at an external target while blinking normally (normal blinking). The upper and lower tear menisci were monitored simultaneously using OCT. Then, 2 consecutive normal blink actions with 1 blink interval (open eye period) were recorded. After that, the subjects were asked to delay each blink as long as possible (delayed blinking), and video recording, including 2 consecutive delayed blink actions with 1 blink interval, was obtained.
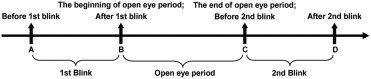
The frames acquired immediately before and after each blink action were processed with custom software as detailed in our previous studies. In brief, both upper and lower tear meniscus variables were obtained, including upper and lower tear meniscus heights and cross-sectional areas. Tear meniscus volumes in upper and lower tear menisci were calculated as described in previous studies. The volume was calculated as the product of the meniscus cross-sectional area, the constant eyelid length of 25 mm, and a factor of 0.75. Because we recorded 2 consecutive blink actions, the meniscus variables obtained before the 2 blink actions were averaged ( Figure 1 ). The meniscus variables obtained after the 2 blink actions were averaged as the same way. Because the 2 consecutive blink actions formed 1 open eye period, the meniscus variables at the beginning of open eye period were obtained after the first blink action. Similarly, the meniscus variables at the end of open eye period were obtained before the second blink action. The blink outcome was defined as the difference in meniscus volume before and after blink action. The open eye outcome was calculated as the difference in meniscus volume at the beginning and the end of the open eye period.
All the data were analyzed electronically. The paired t test was used to identify the differences in tear meniscus variables between normal blinking and delayed blinking. An independent t test was performed to compare the meniscus variables between the dry eye group and the control group.
Results
With normal blinking in dry eye patients, the upper tear meniscus height measured before and after blinking and at the beginning of an open eye period was significantly smaller than those in controls ( P < .05; Table 1 ; Figure 2 ; Figure 3 ). However, there were no significant differences in upper tear meniscus volume ( P > .05). During normal blinking, lower tear meniscus height and volume measured before blinking and at the end of open eye period were smaller in dry eye patients compared with controls ( P < .05; Table 1 ; Figure 3 ). The dry eye patients also had smaller blink outcome and open eye outcome in lower tear meniscus volume ( P < .05; Table 2 ; Figure 4 ).
| UTMH (μm) | UTMV (μL) | LTMH (μm) | LTMV (μL) | |||||
|---|---|---|---|---|---|---|---|---|
| Dry Eye | Controls | Dry Eye | Controls | Dry Eye | Controls | Dry Eye | Controls | |
| Normal blinking | ||||||||
| Blink action | ||||||||
| Before blink | ||||||||
| Mean | 207 a | 241 | 0.28 | 0.34 | 233 a | 287 | 0.36 a | 0.50 |
| ± SD | 74 | 66 | 0.20 | 0.16 | 90 | 100 | 0.25 | 0.33 |
| After blink | ||||||||
| Mean | 190 a | 230 | 0.25 | 0.31 | 227 | 268 | 0.36 | 0.44 |
| ± SD | 87 | 57 | 0.20 | 0.14 | 93 | 97 | 0.28 | 0.32 |
| Open eye period | ||||||||
| The beginning of open eye period | ||||||||
| Mean | 187 a | 230 | 0.25 | 0.30 | 237 | 265 | 0.38 | 0.43 |
| ± SD | 89 | 66 | 0.20 | 0.14 | 100 | 97 | 0.33 | 0.35 |
| The end of open eye period | ||||||||
| Mean | 205 | 242 | 0.29 | 0.34 | 232 a | 283 | 0.35 a | 0.49 |
| ± SD | 88 | 79 | 0.21 | 0.19 | 92 | 103 | 0.23 | 0.35 |
| Delayed blinking | ||||||||
| Blink action | ||||||||
| Before blink | ||||||||
| Mean | 241 | 269 | 0.38 | 0.44 | 317 a | 538 | 0.69 a | 2.19 |
| ± SD | 73 | 73 | 0.27 | 0.20 | 169 | 464 | 0.90 | 3.73 |
| After blink | ||||||||
| Mean | 244 | 278 | 0.39 | 0.44 | 278 a | 479 | 0.54 a | 1.76 |
| ± SD | 87 | 81 | 0.32 | 0.23 | 122 | 390 | 0.48 | 3.42 |
| Open eye period | ||||||||
| The beginning of open eye period | ||||||||
| Mean | 246 | 257 | 0.40 | 0.37 | 283 a | 445 | 0.56 a | 1.37 |
| ± SD | 93 | 79 | 0.34 | 0.20 | 118 | 338 | 0.49 | 2.32 |
| The end of open eye period | ||||||||
| Mean | 237 | 275 | 0.39 | 0.43 | 318 a | 577 | 0.69 a | 2.66 |
| ± SD | 80 | 76 | 0.32 | 0.20 | 150 | 558 | 0.78 | 4.73 |
a Tear meniscus variables in dry eye patients were significantly smaller than those in controls ( P < .05).
| UTMV (μL) | LTMV (μL) | |||
|---|---|---|---|---|
| Dry Eye | Controls | Dry Eye | Controls | |
| Normal blinking | ||||
| Blink outcome | ||||
| Mean | −0.03 | −0.03 | 0.004 a | −0.06 |
| ± SD | 0.07 | 0.11 | 0.06 | 0.15 |
| Open eye outcome | ||||
| Mean | 0.04 | 0.04 | −0.03 a | 0.05 |
| ± SD | 0.13 | 0.13 | 0.13 | 0.12 |
| Delayed blinking | ||||
| Blink outcome | ||||
| Mean | 0.02 | −0.01 | −0.16 | −0.43 |
| ± SD | 0.11 | 0.14 | 0.46 | 1.97 |
| Open eye outcome | ||||
| Mean | −0.01 a | 0.07 | 0.13 a | 1.29 |
| ± SD | 0.14 | 0.17 | 0.36 | 3.08 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


