Purpose
To evaluate acupuncture as treatment for glaucoma.
Design
Prospective double-masked randomized crossover study.
Methods
setting : Clinical practice. population : One eye per patient with primary open-angle glaucoma and stable intraocular pressure (IOP). intervention : Patients were randomized to receive 1 acupuncture series (12 sessions with either eye-related [eye-points] or non-eye-related [non-eye-points] acupoints) and then crossed over to receive the other series. outcome measures : IOP, blood pressure (BP), heart rate (HR), best-corrected visual acuity (BCVA), visual field (VF), optic disc and peripapillary retinal nerve fiber layer (RNFL) measurements, compliance, and adverse reactions. Probability to detect 3 mm Hg IOP difference between series was 90%.
Results
Twenty-two patients volunteered and 11 (50.0%) completed the study; 8 (36.4%) did not complete treatment owing to changes of health, moving away, lack of transportation, or family crisis; and 3(13.6%) were withdrawn owing to needle sensitivity or IOP elevation (8 mm Hg) in the contralateral eye. After an acupuncture session, mean IOP increased slightly with both eye-points (from 12.9 ± 1.8 mm Hg to 13.6 ± 2.0 mm Hg, P = .019) and non-eye-points (from 13.0 ± 1.5 mm Hg to 13.5 ± 1.7 mm Hg, P = .073) series. HR, diurnal IOP, and BCVA showed no statistically significant changes after 12 sessions of either series. Systolic and diastolic BP were reduced after 12 sessions of non-eye-points series ( P = .040, P = .002, respectively). Optic disc, RNFL, and VF showed no statistically significant changes.
Conclusions
Acupuncture has no overall effect on diurnal IOP or BCVA but may temporally increase the IOP immediately after a treatment session. BP is lowered by acupuncture with non-eye-points, but not with eye-points. Compliance and adverse event rates were low.
Glaucoma management in Western medicine is well established and its efficacy has been demonstrated by a number of randomized clinical trials. However, despite medical and surgical therapies, a significant proportion of glaucoma patients continue to go blind. Alternative therapies to reduce the progression rate of glaucoma have been actively sought, but as yet without much success. Acupuncture, a branch of Chinese traditional medicine used for over 2000 years in the treatment of various illnesses, is one alternative therapy that has garnered the attention of many glaucoma patients.
Ocular effects associated with acupuncture have been studied in animal models and in small samples of human subjects. Some studies report beneficial effects such as intraocular pressure (IOP) reduction, improvement of central visual acuity, and alterations of the visual field. However, most of the clinical results are inconclusive because of inadequate research design or incompletely described methodologies. In addition, variable locations of acupoints and different acupuncture intensities, durations, and frequencies of stimulation were studied. This clinical heterogeneity makes scientific analyses or useful comparisons of these acupuncture study results difficult, if not impossible.
The purpose of this investigation was to prospectively evaluate the effects of acupuncture as glaucoma treatment. In particular, IOP, central visual acuity, visual field status, and optic nerve and retinal nerve fiber structure were studied in patients with primary open-angle glaucoma.
Methods
This was a prospective, double-masked, randomized crossover comparative study approved by the Institutional Review Board of the University of California Los Angeles. The study was conducted according to the tenets of the Declaration of Helsinki and all applicable HIPAA rules. Informed consent was obtained from subjects prior to screening and study enrollment. Flyers explaining the nature of the study were available to patients who visited the Glaucoma Division of the Stein Eye Institute. Patients who expressed interest in the study underwent a screening visit for eligibility. Eligibility criteria were primary open-angle glaucoma, age 18 years or older, stable intraocular pressures (less than 2 mm Hg variation in the last 2 follow-up visits over a period of at least 3 months and without alteration of glaucoma therapy for 6 months), no use of any alternative therapy including cannabis, no history of surgical or laser intervention for glaucoma or failed interventions within the prior 3 years, no cardiovascular or neurologic diseases or bleeding disorders, and no retinal abnormalities or nonglaucomatous optic neuropathy. One eye per patient was enrolled; if both eyes qualified for enrollment, only the right eye was enrolled. Diagnosis of primary open-angle glaucoma was made when glaucomatous visual field defects and glaucomatous optic neuropathy were diagnosed by the treating physician (a glaucoma specialist) in the setting of an open angle. Secondary glaucomas were excluded, including pigmentary dispersion, pseudoexfoliation, uveitic, steroid-induced, or traumatic glaucomas.
A separate baseline examination was scheduled after screening to obtain baseline measurements, which included blood pressure (BP) and heart rate (HR), a complete ophthalmic examination, visual field testing, optic disc and peripapillary retinal nerve fiber layer (RNFL) evaluation, and diurnal IOP measurements (measured with Goldmann tonometry every 2 hours from 8 AM to 4 PM). A complete ophthalmic examination consisted of (1) Snellen visual acuity measurement, (2) pupillary reaction evaluation, (3) central corneal thickness measurement, (4) ocular motility evaluation, (5) external and periorbital evaluation, (6) anterior segment examination with slit-lamp biomicroscopy, (7) gonioscopic evaluation of anterior chamber drainage angle, (8) optic disc evaluation, and (9) dilated retinal examination. The visual field was tested with achromatic automated perimetry (Humphrey Field Analyzer [HFA] II; Carl Zeiss Meditec, Dublin, California, USA) with the 24-2 Standard Swedish Interactive Threshold Algorithm (SITA-standard). Optic disc and RNFL measurements were obtained with confocal scanning laser ophthalmoscopy (Heidelberg Retinal Tomography [HRT]; Heidelberg Engineering, Carlsbad, California, USA) and spectral-domain OCT (Cirrus SD OCT; Carl Zeiss Meditec), respectively.
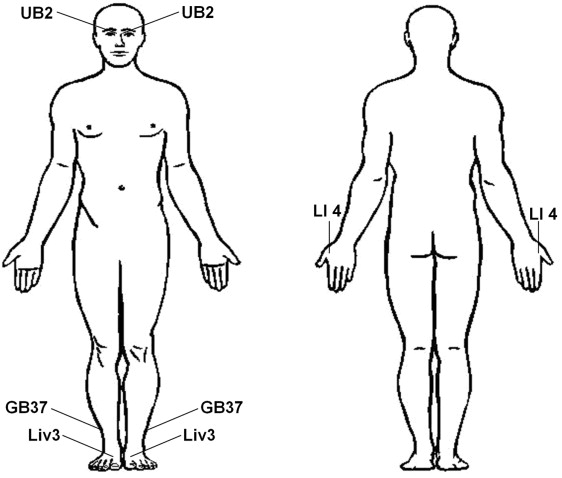
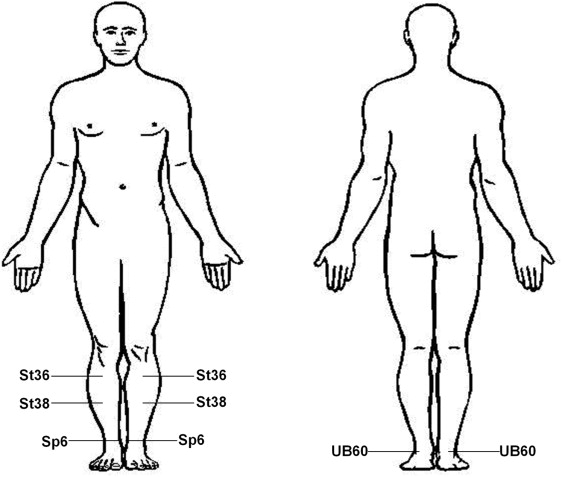
After the baseline examination, patients were scheduled to undergo acupuncture treatment. Acupuncture was performed by an experienced, licensed acupuncturist (S.L.). Two groups of acupuncture points were evaluated. One group of points was related to the eye or used to treat eye diseases according to traditional Chinese acupuncture theory (eye-points). The 4 eye-points were UB2, GB37, Liv3, and LI4 ( Figure 1 ). The second group of acupuncture points was not eye related and is traditionally used to treat nonocular disease (non-eye-points). The 4 non-eye-points were St36, St38, Sp6, and UB60. These non-eye-points are typically used for pain control, stress management, fatigue, and treatment of insomnia and digestive illnesses ( Figure 2 ). There is no consensus among acupuncturists on a set of acupuncture points for treating any particular ocular disease. Literature on acupuncture and Chinese medicine suggests that one cause of ocular disease is an imbalance of body energy flow along the gallbladder (GB) and liver (Liv) meridians. Two eye-points chosen in this study (GB37 and Liv3) belong to these meridians. Eye-points GB37, Liv3, and LI4 were studied in a prospective case series of acupuncture treatment in patients with glaucoma or ocular hypertension. Eye-point UB2, located on the medial end of the eyebrow, belongs to a group of acupuncture points surrounding the orbit that is believed to have a stronger therapeutic effect in treating ocular diseases than distal acupuncture points. Acupuncture needles were placed on points on both sides of the body. Sterile stainless steel disposable acupuncture needles (1 inch 36 gauge needles and 1/2 inch 38 gauge needles) were used. A sensation of numbness and mild aching at the acupoint (traditionally termed “De Qi”) was elicited as an indication of proper needle placement. Each acupuncture treatment session was conducted in an assigned examination room with light dimmed and acupuncture needles left in place for 20 minutes while the patient rested on a 45-degree-reclined examination chair, without electric or laser stimulation of the needle or moxibustion. (Moxibustion is the application of heat resulting from the burning of herbs, or moxa, to acupoints to facilitate the acupuncture effect.) The examination door was closed to avoid noise or disturbance; no music was played.
Patients were randomly assigned (by flipping a coin) to receive 1 acupuncture series, either the eye-points or non-eye-points, for 12 sessions over 6–12 weeks (1–2 sessions per week) and then were crossed over to receive the other acupuncture series (12 sessions over 6–12 weeks) with a washout period of 4 weeks in between. Glaucoma medical therapy was not altered at any time during the study.
Patients and research personnel, except the licensed acupuncturist, were masked to the acupuncture points used, the therapeutic effects of the acupuncture points, and the order of the acupuncture series (whether a patient was receiving the eye-points therapy or the non-eye-points therapy).
BP, HR, and IOP were measured 15 minutes before and after each treatment session. Diurnal IOP measurement and automated visual field measurements were obtained at the baseline visit, within 1 week of completion of the first series of 12 sessions, and within 1 week before and after the second series of 12 sessions. Optic disc (HRT) and RNFL measurements (SD OCT) were obtained at the baseline visit and within 1 week of completing the second acupuncture series. Adverse reactions were recorded throughout the study period.
In this pilot study, a sample size calculation was based on IOP, which is the most important risk factor for glaucoma and the primary parameter monitored in glaucoma therapy. A treatment difference of 3 mm Hg was used based on the results of previous studies. Ten subjects were needed for a 90% probability to detect a treatment difference of 3 mm Hg with a 2-sided .05 significance level, assuming a within-subject standard deviation of 1.5 mm Hg in a 2-treatment crossover study. Standard deviation of 1.5 mm Hg was chosen based on the IOP definition of stability in the inclusion criteria.
Primary outcome measurements included diurnal IOP, best-corrected visual acuity (BCVA), visual field results, and optic nerve and RNFL measurements. Secondary outcome measurements included blood pressure, heart rate, and rates of adverse reactions. BP, HR, and IOP were compared before and after each individual acupuncture treatment session. Diurnal IOP, BCVA, and visual field indices (mean deviation and pattern standard deviation) were compared before and after each series of 12 sessions. Snellen chart visual acuity was converted to the logMAR scale for analysis. Optic nerve and RNFL measurements (linear cup-to-disc area ratio, cup shape measure, rim area, rim volume, RNFL height variation contour, and mean RNFL thickness were measured with HRT; average RNFL thickness and RNFL thickness at superior, nasal, inferior, and temporal quadrants were measured with SD OCT) were compared between the baseline visit and after both 12-session series were completed. Paired Student t tests were used to compare variables before and after interventions. Mean values are reported with their standard deviations (±SD). Adverse reactions were reported using descriptive statistics. Microsoft Office Excel 2010 Analysis ToolPak (Microsoft, Redmond, Washington, USA) was used for statistical analysis.
Results
Twenty-two glaucoma patients volunteered to participate in the study and 11 patients (50.0%) completed the study. Eight patients (36.4%) did not complete the study; 2 of the 8 patients had changes in their health unrelated to glaucoma or acupuncture, 2 of the 8 moved away, 3 had problems with transportation during the study, and 1 had a family crisis. An additional 3 patients (13.6%) were withdrawn from the study by one of the investigators owing to needle sensitivity (2 patients) and to clinically significant elevated IOP (8 mm Hg) in the contralateral eye that required a change in glaucoma treatment for the patient. Table 1 summarizes the demographic characteristics of patients who completed and did not complete the study.
| Patients who Completed the Study | Patients who Did Not Complete the Study | |
|---|---|---|
| Number of patients | 11 | 11 |
| Mean age, y (range) | 63.7 ± 14.3 (35.6–87.6) | 64.5 ± 10.0 (45.0–76.7) |
| Sex: female/male | 8/3 | 8/3 |
| Race: white/black/Hispanic/Asian | 5/1/2/3 | 10/0/0/1 |
| On systemic beta-blockers | None | None |
| Mean central corneal thickness (μm) | 528.8 ± 39.1 | 533.1 ± 43.4 |
| Lens status: phakic/pseudophakic | 10/1 | 7/4 |
| Previous laser trabeculoplasty | 0 | 0 |
| Previous trabeculectomy | 2 | 1 |
| Previous cataract surgery | 1 | 4 |
Intraocular Pressure
After each acupuncture session, with either eye-points or non-eye-points, mean IOP of the treatment groups exhibited a slight increase. After treatment of the eye-points, mean IOP increased from 12.9 ± 1.8 mm Hg immediately before to 13.6 ± 2.1 mm Hg immediately after the treatment session ( P = .019, Table 2 ). A borderline statistically significant increase of mean IOP was noted with the non-eye-point sessions too (from 13.0 ± 1.5 mm Hg to 13.5 ± 1.7 mm Hg, P = .073). This IOP effect appears to be temporary, as no significant change of diurnal IOP was detected after 12 sessions of eye-related or non-eye-related acupuncture treatments ( Table 3 ). Mean diurnal IOPs were 12.9 ± 2.0 mm Hg before and 12.7 ± 2.0 mm Hg after 12 sessions of eye-related acupuncture treatment, and 13.1 ± 1.8 mm Hg before and 12.8 ± 1.8 mm Hg after 12 sessions of non-eye-related acupuncture treatment ( P = .711 and P = .381, respectively).
| Before Individual Treatment Session | After Individual Treatment Session | P Value (Paired Student t Test) | |
|---|---|---|---|
| Eye-Related Acupuncture Treatment | |||
| Mean systolic blood pressure (mm Hg) | 118.6 ± 17.3 | 121.6 ± 18.0 | .040 |
| Mean diastolic blood pressure (mm Hg) | 72.0 ± 6.1 | 72.0 ± 7.2 | .976 |
| Mean heart rate (beats per minute) | 66.8 ± 13.1 | 64.1 ± 9.8 | .082 |
| Mean intraocular pressure (mm Hg) | 12.9 ± 1.8 | 13.6 ± 2.1 | .019 |
| Non-Eye-Related Acupuncture Treatment | |||
| Mean systolic blood pressure (mm Hg) | 120.5 ± 13.2 | 118.1 ± 13.8 | .015 |
| Mean diastolic blood pressure (mm Hg) | 71.1 ± 7.4 | 71.2 ± 9.7 | .901 |
| Mean heart rate (beats per minute) | 67.6 ± 10.5 | 64.3 ± 8.5 | .006 |
| Mean intraocular pressure (mm Hg) | 13.0 ± 1.5 | 13.5 ± 1.7 | .073 |
| Before 12 Treatments | After 12 Treatments | P Value (Paired Student t Test) | |
|---|---|---|---|
| Eye-Related Acupuncture Treatment | |||
| Mean systolic blood pressure (mm Hg) | 122.5 ± 17.7 | 119.0 ± 15.3 | .291 |
| Mean diastolic blood pressure (mm Hg) | 72.5 ± 8.5 | 71.8 ± 8.6 | .771 |
| Mean heart rate (beats per minute) | 60.0 ± 11.6 | 64.4 ± 11.7 | .067 |
| Mean best-corrected visual acuity (logMAR) | 0.084 ± 0.138 | 0.084 ± 0.138 | >.999 |
| Mean diurnal intraocular pressure (mm Hg) | 12.9 ± 2.0 | 12.7 ± 2.0 | .711 |
| Non-Eye-Related Acupuncture Treatment | |||
| Mean systolic blood pressure (mm Hg) | 126.5 ± 19.7 | 116.2 ± 16.8 | .040 |
| Mean diastolic blood pressure (mm Hg) | 78.4 ± 7.4 | 69.5 ± 9.7 | .002 |
| Mean heart rate (beats per minute) | 61.1 ± 9.2 | 62.4 ± 10.4 | .565 |
| Mean best-corrected visual acuity (logMAR) | 0.102 ± 0.125 | 0.097 ± 0.140 | .895 |
| Mean diurnal intraocular pressure (mm Hg) | 13.1 ± 1.8 | 12.8 ± 1.8 | .381 |
Vital Signs (Blood Pressure and Heart Rate)
BP and HR responses were different after single eye-point and non-eye-point treatment sessions. The mean systolic BP and HR of the entire group showed a significant reduction after a single non-eye-point session ( Table 2 ). Mean systolic BP decreased from 120.5 ± 13.2 mm Hg immediately before to 118.1 ± 13.8 mm Hg immediately after a treatment session ( P = .015), while mean HR decreased from 67.6 ± 10.5 beats per minute (bpm) immediately before to 64.3 ± 8.5 bpm immediately after treatment ( P = .006). In contrast, after an eye-point session, mean systolic BP increased from 118.5 ± 17.3 mm Hg before to 121.6 ± 18.0 mm Hg after the session ( P = .040). HR went from 66.8 ± 13.1 bpm before to 64.1 ± 9.8 bpm after an eye-point treatment ( P = .082). Mean diastolic BP did not change with either treatment.
The BP response observed after individual non-eye-point treatment sessions appeared to be sustained. After completion of the series of 12 sessions of non-eye-point acupuncture, mean systolic BP decreased from 126.5 ± 19.7 mm Hg to 116.2 ± 16.8 mm Hg and mean diastolic BP was lowered from 78.4 ± 7.4 mm Hg to 69.5 ± 9.7 mm Hg ( P = .040 and P = .002, respectively). Changes in HR were not statistically significant (from 61.1 ± 9.2 bpm to 62.4 ± 10.4 bpm, P = .565). For eye-point acupuncture, no statistically significant changes were noted in the systolic BP, diastolic BP, or HR after 12 treatment sessions ( Table 3 ).
Vision Acuity
BCVA (logMAR scale) did not change after 12 sessions of either eye-point or non-eye-point acupuncture treatments. BCVA was 0.084 ± 0.138 before eye-point acupuncture treatment (equivalent to Snellen 20/24) and 0.102 ± 0.125 before the non-eye-point series (equivalent to Snellen 20/25). It remained essentially unchanged after 12 sessions of either treatment (0.084 ± 0.138, 0.097 ± 0.140, P >.999 and P = .895, respectively, Table 3 ).
Heidelberg Retinal Tomography, Spectral-Domain Optical Coherence Tomography, Visual Field
The visual field was tested before and after 12 sessions of eye-related and before and after 12 sessions of non-eye-related acupuncture treatments, while optic disc measurements with HRT and RNFL thickness with SD OCT were obtained at baseline and after the last acupuncture treatment in the study. None of the visual field indices (mean deviation and pattern standard deviation), optic disc, or RNFL thickness measurements demonstrated any statistically significant changes ( Tables 4–6 ).
| Before 12 Treatments | After 12 Treatments | P Value (Paired Student t Test) | |
|---|---|---|---|
| Eye-Related Acupuncture Treatment | |||
| Average mean deviation (dB) | −5.44 ± 7.58 | −5.75 ± 5.22 | .409 |
| Average pattern standard deviation (dB) | 5.47 ± 4.46 | 7.28 ± 4.34 | .259 |
| Non-Eye-Related Acupuncture Treatment | |||
| Average mean deviation (dB) | −4.98 ± 6.11 | −4.99 ± 5.78 | .997 |
| Average pattern standard deviation (dB) | 5.61 ± 4.77 | 5.78 ± 4.83 | .554 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


