Invasive thyroid cancer is often asymptomatic and can take the surgeon and the patient by surprise. Maintenance of a high level of suspicion in patients who present with symptoms, an abnormal examination, recurrent disease, or documented metastatic disease lead the clinician to obtain appropriate cross-sectional imaging that helps to define the full extent of the disease. Specific guidelines are provided for the management of the various structures in the neck that are at risk for involvement by disease extension outside the gland or extracapsular extension outside a lymph node with involvement by metastatic disease. This article reviews the prognosis, diagnosis, management, and implications of invasive thyroid cancer affecting the various structures of the central and lateral compartments of the neck.
Gross involvement of the trachea or esophagus is almost a certain sign against curability, and yet one may be tempted into an extensive and dangerous operation to remove the diseased tissue…. D Balfour, Medical Record, 1918
The rapid increase in well-differentiated thyroid cancer, in particular papillary thyroid cancer, has led to a proportionate increase in the volume of thyroid surgery performed in the United States and abroad. The 3 primary disciplines involved in treating thyroid cancer are surgery, endocrinology, and nuclear medicine.
Surgery remains the initial form of treatment of virtually all patients who have well-differentiated thyroid malignancies. The surgeon performing that surgery is charged with the responsibility of removing all evidence of disease located in the central compartment of the neck, including the mediastinum, as well as nodal disease that is often present in the lateral compartments of the neck. That surgery is currently being performed by surgeons with a range of training experience in performing routine thyroidectomy, paratracheal node dissection, lateral compartment nodal dissection, and mediastinal dissection. Although most cases of well-differentiated thyroid cancer do not require the skill sets to manage aerodigestive tract involvement or nerve involvement, when the disease requires that such intervention is essential for a complete resection, it is incumbent on the surgeon to be able to manage such cases of advanced disease in the primary setting. Closing the wound after performing a more limited resection and referring the patient to a surgeon who performs that type of surgery after the patient develops a recurrence has been shown to lead to a less favorable outcome.
Specialties that are involved in the surgical management of thyroid cancer include otolaryngologists, endocrine surgeons, general surgeons, and surgeons with fellowship training in surgical oncology. Although statistics show that most of the incremental new cases of thyroid cancer that are treated each year are for early stage disease, there remains an ever-present danger that a patient presenting with thyroid cancer may have invasive disease that will complicate the surgical procedure and challenge the surgeon to perform a complete resection and render the patient functionally intact. It is imperative that all specialties performing thyroid cancer surgery are trained in all aspects of upper aerodigestive tract resection and reconstruction so that they are prepared to meet the demands that disease in these patients can present.
Identifying the patient with invasive thyroid cancer
One of the major challenges in treating patients with invasive thyroid cancer is that most patients with this form of the disease are asymptomatic and the disease takes the patient and the surgeon unawares. Four types of patients can be identified before surgery as having an increased likelihood of invasive disease:
- 1.
Asymptomatic patients who present with an abnormal examination related to either vocal cord dysfunction or evidence of a subglottic or tracheal mass. The identification of vocal cord paralysis is 1 of the first clues that the surgeon is dealing with invasive disease that has extended outside the normal bounds of the thyroid gland to involve the recurrent laryngeal nerve (RLN).
- 2.
Patients with recurrent thyroid cancer in the central compartment.
- 3.
Symptomatic patients with biopsy-proven thyroid cancer who present with a change in voice, dyspnea, hemoptysis, or dysphagia.
- 4.
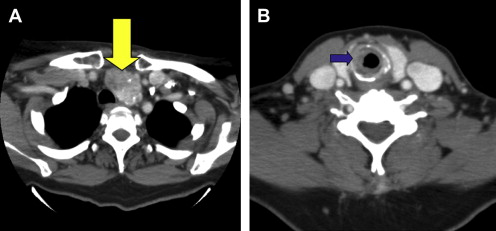
Patients with documented invasive disease based on preoperative cross-sectional imaging of the central compartment showing invasion of the central viscera, or lateral compartment nodal metastases showing extracapsular extension.
All patients in the first 3 groups should undergo cross-sectional imaging before surgery to better anticipate the extent of the surgery that is required to achieve a complete resection. One additional category of patient is the one who presents with pulmonary or other systemic metastases that are found to be of thyroid origin. Such patients should undergo cross-sectional imaging of the neck and the mediastinum.
Despite the ominous appearance of an intraluminal tracheal mass in a patient with biopsy-proven thyroid cancer, the surgeon should be aware that all that is present in the trachea is not always invasive thyroid cancer. In 1 of my own memorable cases of thyroid cancer arising in an opera singer, preoperative imaging showed the presence of what was believed to be intraluminal extension of her disease, only to find out on the final pathologic review that the tracheal component was actually a benign thyroid rest that was not identified as benign disease until after the tracheal resection had been performed. In another symptomatic patient with a biopsy suspicious for thyroid cancer, preoperative imaging identified an intraluminal mass that proved to be a chondrosarcoma arising from a tracheal ring. The fine-needle aspiration had traversed the thyroid and led to a false-positive cytologic report ( Fig. 1 ). A patient with a large thyroid mass and a suspicious cytology was found to have intraluminal narrowing on preoperative imaging performed because of her symptomatic respiratory difficulty. The thyroidectomy proved to be benign, and the tracheal narrowing was caused by a benign tracheal stenosis of unknown cause ( Fig. 2 ). Yet another patient developed severe airway compromise as a result of intraluminal extension of a paratracheal mass, which proved to be a schwannoma of the RLN ( Fig. 3 ). Although most patients with an intraluminal mass and biopsy-proven thyroid cancer do indeed have invasive thyroid disease, it is not always the case.

There is a well-documented entity know as a collision tumor of the upper aerodigestive tract that results from 2 separate neoplastic processes arising in a contiguous manner to involve either the thyroid gland alone with 2 separate histologic subtypes, or the thyroid gland and the aerodigestive tract. The author recently reported such a case in which a papillary thyroid cancer was diagnosed preoperatively and a coexistent vocal cord paralysis led to cross-sectional imaging. The computed tomography (CT) scan showed findings that were interpreted as invasive thyroid cancer. Fiberoptic examination did not show any signs of a mucosal-based neoplastic process; however, because of destruction of the cricoid in this older male patient, the decision was made to proceed with a total thyroidectomy and a total laryngectomy. Final pathologic review identified a subglottic squamous cell cancer that had caused the cartilage destruction, and abutted against the intraglandular papillary thyroid cancer.
Incidence of invasive well-differentiated thyroid cancer
It is difficult to know the true incidence of invasive thyroid cancer because it seems to be a moving target. With the increased incidence of small thyroid cancers detected as a result of more widespread use of ultrasonography, the percentage of cases of invasive disease has decreased accordingly. However, there are several institutional case series that give a glimpse of the reported incidence of aerodigestive tract invasion in tertiary referral centers. The range of invasive well-differentiated thyroid cancer is 1% to 23%. In the Mayo Clinic series reported by Djalilian and colleagues 18 patients had thyroid cancer extending into the lumen of the larynx or trachea out of a total of 2000 patients treated for thyroid cancer at that institution from 1913 to 1973. The risk of upper aerodigestive tract involvement, nerve involvement, and muscle involvement is directly related to the presence of extrathyroidal extension (ETE) of the primary tumor and extracapsular invasion in a metastatic lymph node. Numerous prognostic factors have been evaluated and adopted by the various staging systems for well-differentiated thyroid cancer; among them:
- 1.
Size of the tumor
- 2.
Age of the patient
- 3.
Presence of ETE.
The incidence of extrathyroidal disease increases with increasing size of the primary malignancy ; however, even micropapillary cancers can extend outside the thyroid gland to place the RLN, the tracheal cartilage, the larynx, and esophagus at risk. The risk of ETE is related to the biology of the tumor as well as its geographic location within the thyroid lobe, whether it is in the middle or on the periphery of the gland. The incidence of ETE in micropapillary carcinomas has been reported to be as high as 31.9%. The presence of ETE is associated with an increased incidence of recurrent disease and death caused by disease. Breaux and Guillamondegui reviewed the institutional experience with invasive thyroid cancer at MD Anderson Cancer Center and found that primary tumor size greater than 4 cm was associated with an increased incidence of mortality from disease. Involvement of more than 4 structures by the invasive disease was reported to be uniformly fatal. Similarly, primary tumor size greater than 4 cm was identified as a significant adverse prognostic factor by Andersen and colleagues in patients older than 45 years with invasive thyroid cancer.
The presence of disease extension outside the capsule of lymph nodes has been identified as a significant negative prognostic factor in patients with metastatic squamous cell cancer. Few studies have reported the incidence and prognostic significance of extracapsular extension in nodal metastases from papillary thyroid cancer. Yamashita and colleagues reported the results of a multivariate analysis in 1997 in which they concluded that disease extension outside the capsule of a lymph node harboring metastatic papillary thyroid cancer had a significant effect on the risk of distant disease as well as the risk of dying from disease. In addition, these investigators identified the risk of extranodal extension as being higher in larger lymph nodes than smaller nodes, and also found that large nodal deposits and extrathyroidal invasion correlated with the development of distant disease and death. In the Yamashita study, 50% of the patients who died of disease succumbed within the first 10 years following treatment. Akslen and colleagues reported that extracapsular extension of well-differentiated thyroid cancer was associated with a short recurrence-free survival interval, but not with increased 10-year mortality. It is unclear whether the lack of longer-term follow-up led to this discrepancy between these 2 studies.
Incidence of invasive well-differentiated thyroid cancer
It is difficult to know the true incidence of invasive thyroid cancer because it seems to be a moving target. With the increased incidence of small thyroid cancers detected as a result of more widespread use of ultrasonography, the percentage of cases of invasive disease has decreased accordingly. However, there are several institutional case series that give a glimpse of the reported incidence of aerodigestive tract invasion in tertiary referral centers. The range of invasive well-differentiated thyroid cancer is 1% to 23%. In the Mayo Clinic series reported by Djalilian and colleagues 18 patients had thyroid cancer extending into the lumen of the larynx or trachea out of a total of 2000 patients treated for thyroid cancer at that institution from 1913 to 1973. The risk of upper aerodigestive tract involvement, nerve involvement, and muscle involvement is directly related to the presence of extrathyroidal extension (ETE) of the primary tumor and extracapsular invasion in a metastatic lymph node. Numerous prognostic factors have been evaluated and adopted by the various staging systems for well-differentiated thyroid cancer; among them:
- 1.
Size of the tumor
- 2.
Age of the patient
- 3.
Presence of ETE.
The incidence of extrathyroidal disease increases with increasing size of the primary malignancy ; however, even micropapillary cancers can extend outside the thyroid gland to place the RLN, the tracheal cartilage, the larynx, and esophagus at risk. The risk of ETE is related to the biology of the tumor as well as its geographic location within the thyroid lobe, whether it is in the middle or on the periphery of the gland. The incidence of ETE in micropapillary carcinomas has been reported to be as high as 31.9%. The presence of ETE is associated with an increased incidence of recurrent disease and death caused by disease. Breaux and Guillamondegui reviewed the institutional experience with invasive thyroid cancer at MD Anderson Cancer Center and found that primary tumor size greater than 4 cm was associated with an increased incidence of mortality from disease. Involvement of more than 4 structures by the invasive disease was reported to be uniformly fatal. Similarly, primary tumor size greater than 4 cm was identified as a significant adverse prognostic factor by Andersen and colleagues in patients older than 45 years with invasive thyroid cancer.
The presence of disease extension outside the capsule of lymph nodes has been identified as a significant negative prognostic factor in patients with metastatic squamous cell cancer. Few studies have reported the incidence and prognostic significance of extracapsular extension in nodal metastases from papillary thyroid cancer. Yamashita and colleagues reported the results of a multivariate analysis in 1997 in which they concluded that disease extension outside the capsule of a lymph node harboring metastatic papillary thyroid cancer had a significant effect on the risk of distant disease as well as the risk of dying from disease. In addition, these investigators identified the risk of extranodal extension as being higher in larger lymph nodes than smaller nodes, and also found that large nodal deposits and extrathyroidal invasion correlated with the development of distant disease and death. In the Yamashita study, 50% of the patients who died of disease succumbed within the first 10 years following treatment. Akslen and colleagues reported that extracapsular extension of well-differentiated thyroid cancer was associated with a short recurrence-free survival interval, but not with increased 10-year mortality. It is unclear whether the lack of longer-term follow-up led to this discrepancy between these 2 studies.
Structures involved by invasive thyroid cancer
A variety of different structures can be involved in invasive thyroid cancer. Central compartment disease can invade the viscera and nerves of the central compartment as well as to extend laterally or extend caudally to involve mediastinal structures. Those structures can be divided in several different ways: they might be classified based on visceral structures, muscles, nerves, and vessels; alternatively, dividing the structures at risk based geographically on central compartment and lateral compartment is the more common way to approach this topic.
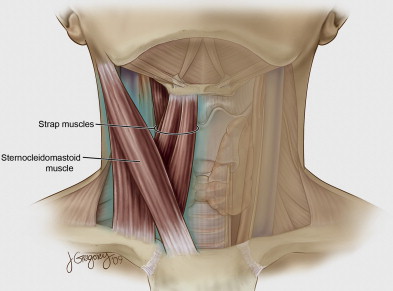
The central compartment viscera include the larynx, trachea, and esophagus. In addition, the strap muscles are the structures most commonly involved by invasive thyroid cancer. The RLN is the nerve most commonly affected by invasive disease in the central compartment. The superior laryngeal nerve is rarely reported separately in large series of invasive thyroid disease. The caudal portion of the central compartment extends to the mediastinum, where the innominate artery and vein are at risk.
In the lateral compartment, the major vascular structures are the internal jugular vein and the common carotid artery. The neurologic structures include the vagus nerve, cervical sympathetic chain, phrenic nerve, and the spinal accessory nerve. Although theoretically possible, it is rare that the hypoglossal nerve is invaded by nodal disease in the upper jugular region. The sternocleidomastoid (SCM) muscle can also be invaded by extracapsular extension of metastatic nodes.
Some series have identified the incidence of involvement of various cervical structures by invasive thyroid cancer. In the series reported by Breaux and Guillamondegui, 47 patients with invasive disease were analyzed. The RLN was involved in 22 (47%), the trachea was involved in 28 (60%), the larynx in 16 (34%), the esophagus in 8 (17%), and the strap muscles or platysma in 20 (43%) patients. In addition, the vagus nerve was involved in 2 (4%) patients, the jugular vein in 6 (13%), the carotid artery in 3 (6%), and the skin in 2 (4%) patients. In Nakao’s series of 31 patients requiring tracheal resection, the following structures also required resection: RLN (61%), phrenic nerve (10%), vagus (13%), and spinal accessory nerve (6%), strap muscles or SCM (78%), jugular vein (45%), and esophageal muscle in 29%. Transmural extension to involve the esophageal mucosa was reported in only 6% of patients. Nishida and colleagues reported the following structures involved by invasive thyroid cancer in 117 patients: trachea (59%), esophagus (31%), internal jugular vein (38%), carotid artery (7%), strap muscles and SCM (77%), vagus nerve (8%), and RLN (61%). Kowalski and Filho reported the following structures involved in 46 patients with invasive thyroid cancer: trachea (46%), muscle (41%), RLN (33%), larynx (24%), major vessel (13%), and esophagus (9%). From a review of these 4 series alone it is apparent that there is significant variability in the incidence of the various structures involved. The incidence of esophageal involvement ranges from 9% to 31%, the involvement of the RLN ranges from 33% to 61%, tracheal involvement ranges from 46% to 100%, and carotid artery involvement from 0% to 7%.
In the Mayo Clinic series reported by McCaffrey and colleagues, the invasion of different structures was found to have a different effect on survival. In that series, the involvement of muscle was found in 53%, the trachea in 37%, the RLN in 47%, esophagus in 21%, larynx in 12%, and a variety of other sites in 30%. Analysis of the different subsites identified the trachea and esophagus as having a statistically significant independent effect on survival, whereas completeness of resection approached statistical significance. Alternatively, invasion of muscle, the RLN, and larynx did not have a significant independent effect on survival. It is unclear why involvement of different structures should lead to a different effect on survival. The biology of ETE and extracapsular invasion from a lymph node is seemingly the same and is a reflection of the aggressiveness of the tumor, although the actual structures involved are in part a product of the geographic location as well as the size of the tumor within the thyroid gland or the location of the lymph node within the central or lateral compartments of the neck or mediastinum.
Decision making in management of invasive thyroid cancer
The central premise of managing patients with invasive thyroid cancer is to clear the central compartment of the neck to protect the patient’s vital functions of being able to breathe comfortably, speak, and maintain nutrition through oral alimentation. Although a tracheostomy and a feeding gastrostomy tube can be placed, the unchecked growth of disease in the central neck challenges the patency of even a surgically created airway. The histology of the tumor, the degree of differentiation and the age of the patient are critical parameters in determining the opportunity and the likelihood of success of treating invasive thyroid cancer with adjuvant therapy once a resection has been performed. The likelihood of disease response to radioiodine ( 131 I) therapy has significant importance for the surgeon in terms of how complete a resection must be accomplished and what the implications are of leaving macro- or microscopic disease.
Recurrent thyroid cancer most often presents as nodal recurrence and often has a documented biology that is resistant to 131 I therapy. The decision to perform extensive central compartment resections in patients with metastatic disease involves a complex decision-making process. It raises the issue as to how extensive the work-up should be before performing surgery. The most commonly reported sites for metastatic thyroid cancer are the lung and bone. The liver and brain are less frequently involved. In contemporary thyroid cancer management, the performance of a positron emission tomography CT scan can provide valuable information regarding the extent of disease as well as the likelihood of 131 I uptake. However, the luxury of obtaining that information is lost when the invasive nature of a thyroid cancer is unsuspected before the initiation of the surgery.
Site-specific management of invasive thyroid cancer
Strap Muscle and SCM Muscle Invasion
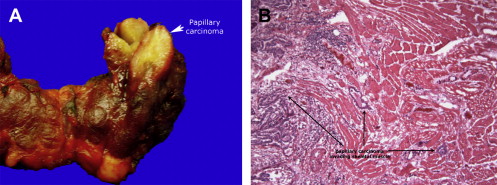
Involvement of the strap, platysma, and the SCM muscles rarely causes any specific symptoms ( Fig. 4 ). The initial approach during thyroid surgery involves elevation of the sternothyroid muscle off the surface of the thyroid gland. Adherence of the strap muscles to the surface of the gland can be seen with thyroiditis but it is often the first indication for the surgeon of the biologic aggressiveness of the thyroid cancer. Resection of the strap muscles and the SCM muscles causes little functional effect on most patients, except for professional voice users, who may be negatively affected by loss of the accessory muscles of voice production. Resection of the SCM muscle has little functional effect but does lead to loss of volume in the lateral neck, producing a contour deformity. In most instances, a cuff of muscle should be resected to obtain clearance around a biologically aggressive thyroid cancer ( Fig. 5 ).
Laryngotracheal Complex
Because most patients who die of thyroid cancer die of airway obstruction due to invasion of the structures in the midline visceral compartment with encroachment on the airway, surgeons probably should expend as much effort on the problem of what to do at the primary operation when there is invasion of the visceral compartment, superficial or otherwise, as they do on the problem of cervical lymph node metastasis. Djalilian M, 1974
Involvement of the larynx and trachea led to preoperative symptoms in 28% and 18% of patients, respectively with documented invasive thyroid cancer in Kowalski’s series ( Fig. 6 ). In the series by McCarty and colleagues, 40 patients with frank airway invasion were analyzed and 11% reported hemoptysis, dyspnea was reported in 5%, and only 22% were found to have hoarseness. The poor correlation between voice changes and the presence of vocal cord paralysis is discussed in the section on nerve involvement. However, the development of dyspnea is seen only when the cross-sectional airway of the trachea has been narrowed by at least 50%, either by intrinsic disease or extrinsic compression. The rate of narrowing of the airway also affects the patient’s awareness of dyspnea. When the process occurs slowly, patients often report that they accommodate in remarkable ways and often are incorrectly diagnosed with reactive airway disease or sleep apnea before the correct diagnosis is established.
Virtually all patients who are advised to undergo thyroid surgery have had an ultrasound examination as part of their preoperative evaluation. The performance of cross-sectional imaging is less common unless symptoms, the presence of recurrent disease, or physical findings warrant that intervention. Shimamoto and colleagues reported the sensitivity for ultrasound detection of tracheal invasion was 42.9% and for esophageal invasion it was 28.6%. Yamamura and colleagues reported a higher level of sensitivity, with 9 of 10 patients with intercartilaginous involvement predicted by ultrasound along with 9 of 10 patients with mucosal involvement. The experience of thyroid ultrasonographers varies greatly. In addition, the number of cases of invasive thyroid cancer that are seen regularly by most endocrinologists who are performing thyroid ultrasound and ultrasound-guided biopsies makes it unlikely that most patients with invasive disease are accurately diagnosed before surgery.
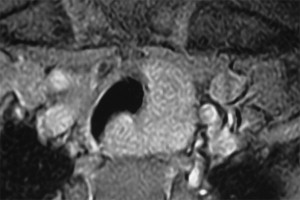
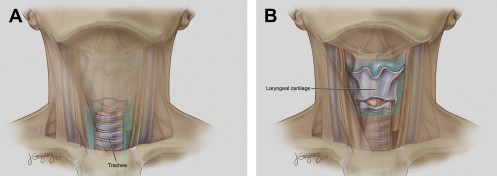
The mechanism for invasion of the upper aerodigestive tract by an invasive thyroid cancer has been delineated by McCaffrey and colleagues. Disease may gain access to the airway by way of the primary tumor in the thyroid or via a paratracheal node involved by metastatic disease. Fig. 7 A illustrates the routes of invasion around the posterior thyroid ala to gain access to the paraglottic space. In Fig. 7 B the entry is from a paratracheal node, which can directly invade the tracheal cartilage or gain entry to the membranous wall of the trachea at the level of the tracheoesophageal groove. Direct invasion of the thyroid cartilage may occur through larger primary thyroid malignancies (see Fig. 7 C). Anterior airway invasion may occur through primary tumors involving the isthmus or from delphian or pretracheal lymph nodes involved by metastatic disease manifesting extracapular extension (see Fig. 7 D). A delphian lymph node involved by metastatic papillary thyroid cancer is shown in Fig. 8 .




