Purpose
To determine in primary congenital glaucoma whether age of presentation influences surgical success, the degrees of angle surgery needed to achieve glaucoma control, and whether there are critical ages where glaucoma progresses, requiring further surgical management.
Design
Retrospective cohort study.
Methods
The medical records of patients with primary congenital glaucoma over a 23-year period were reviewed: 192 procedures were performed on 117 eyes (70 patients). The number and age of angle procedures and final visual acuity was analyzed. Surgical success was defined as stable intraocular pressure and optic disc appearance.
Results
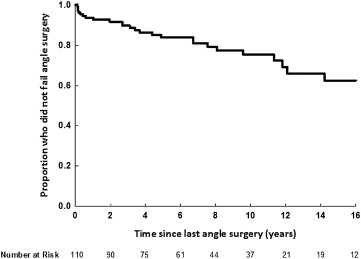
Procedures involving 83 of the 110 eyes (75.5%) undergoing angle surgery were successful, with 2-, 4-, 6-, and 10-year success rates of 92%, 86%, 84%, and 75%, respectively. Subgroup analysis (<3 months; 3–6 months; >6 months) comparing age of diagnosis to visual outcome (<20/200, 20/200–20/40, >20/40) was significant ( P = .04). The age at first operation ( P = .94), the number of angle operations ( P = .43), and their effect on angle surgery success was not significant. Seven of 192 operations were performed after the age of 8 years (3.6%). After the initial angle surgeries within the first year of life, the third procedure occurred at a median age of 2.4 years (interquartile ratio [IQR] 0.6–3.8 years) and the fourth procedure occurred at a median age of 5.3 years (IQR 2.5–6.1 years).
Conclusions
Children diagnosed at <3 months of age had a visual outcome of <20/200 despite successful glaucoma control. Age of presentation did not affect surgical success. A total of 78.9% of cases undergoing primary trabeculotomy were controlled with 1 operation: 4 clock hours of angle (120 degrees). Analysis of glaucoma progression suggests critical ages where further glaucoma surgery is required at around 2 and 5 years of age.
Primary congenital glaucoma, a congenital anomaly of the anterior segment of the eye, requires lifelong management and is associated with significant morbidity, including visual loss. The presumed pathogenesis is a delay or failure of angle development, thought to result from the arrested maturation of tissues derived from cranial neural crest cells. Although many cases are sporadic, primary congenital glaucoma is inherited in an autosomal recessive manner. The CYP1B1 gene is most consistently identified and the frequency of its involvement varies with ethnic group. The mechanism by which CYP1B1 mutations cause primary congenital glaucoma is not yet known.
Patients typically present in the first 12 months of life, with corneal clouding, buphthalmos, and observed photophobia. The Childhood Glaucoma Research Network expanded and standardized the definition of primary congenital glaucoma to require 2 or more of the following criteria: an intraocular pressure (IOP) >21 mm Hg, optic disc cupping, corneal findings (Haab striae, corneal edema, or diameter ≥11 mm in newborns, >12 mm infants less than 1 year of age, or >13 mm in any age), ocular enlargement by progressive myopia or axial length out of keeping with normal growth, or a visual field defect consistent with glaucoma. Eyes meeting these criteria are then subcategorized into 3 groups based on age of onset: neonatal or newborn (onset age 0–1 month), infantile (onset >1–24 months), late onset or late recognized (onset >2 years). Spontaneously arrested cases with normal IOP but typical signs of primary congenital glaucoma are also classified as primary congenital glaucoma. Initial treatment is angle surgery, which aims to eliminate the obstruction to aqueous outflow.
Most studies have assessed the outcomes of all forms of childhood glaucoma as a single cohort. This study examines the outcomes for patients with isolated primary congenital glaucoma. This large recent study of a pure primary congenital glaucoma cohort seen over a 23-year period at The Children’s Hospital Westmead, Sydney, Australia enables analysis of outcomes relating to modern surgical treatment, age of treatment, and visual outcome. Three main areas were investigated: (1) whether age at presentation (less than 3 months vs 3–6 months vs greater than 6 months) influences surgical success and/or visual outcome; (2) the number of degrees of angle surgery needed to achieve successful glaucoma control; and (3) whether there are critical ages where glaucoma progresses, requiring further surgery following previous successful angle surgery. These areas of study have not been thoroughly investigated previously.
Patients and Methods
Data Collection
A retrospective cohort study was conducted investigating the medical records of all patients with primary congenital glaucoma treated between 1989 and 2012 at The Children’s Hospital at Westmead from a diagnostic coding database. The study was approved by the Children’s Hospital Westmead Human Research Ethics Committee. Patients were excluded from the study if they had secondary pediatric glaucoma or an acquired diagnosis, inadequate length of follow-up (less than a year), incomplete follow-up, or initial management of glaucoma at another hospital.
Outcome Measures
The diagnosis of primary congenital glaucoma was based on the presence of corneal enlargement (buphthalmos), loss of corneal transparency/Haab striae, photophobia, and raised IOP with or without optic disc cupping. There had to be an absence of other forms of anterior segment dysgenesis. Following the publication of the Childhood Glaucoma Research Network Classification of Childhood Glaucoma, the clinical details were cross checked with these guidelines. The included patient cohort all met the Childhood Glaucoma Research Network guidelines.
The age at diagnosis, age of initial surgery, presence of unilateral or bilateral pathology, and information on the number and type of ocular surgeries was documented. Intraocular pressure, refraction, optic disc appearance, and visual acuity were also documented for the date of last available follow-up. Intraocular pressure was measured in the outpatient department with an Icare tonometer (Icare tonometer Helsinki, Finland) or in theatre during induction with a Perkins hand-held tonometer (Clement Clark, Haag-Streit, Essex, UK). Visual acuities were measured using fixation or Teller grating acuity cards for nonverbal children and Lea symbols, Kay’s pictures, Sheridan Gardner, and Snellen letters progressively for verbal children, as cooperation allowed. Any development of amblyopia was treated with glasses and patching as per the Pediatric Eye Disease Investigator Group (PEDIG) studies. At final follow-up, refractive error was recorded and deemed significant myopia/hyperopia if greater than ±2.0 diopters, and astigmatism if greater than 1.5 diopters.
Surgical Procedures and Success Criteria
The outcome of surgical intervention was analyzed and considered successful once no further glaucoma surgical procedure was necessary. This was based on IOP less than or equal to 21 mm Hg, stable optic disc appearance, and refraction. Patients were clinically managed by 1 of 5 pediatric ophthalmologists. The surgeries conducted were goniotomy, trabeculotomy, trabeculectomy, placement of an aqueous drainage device, cyclophotocoagulation, and Scheies procedure. There was 1 enucleation performed. Goniotomy and trabeculotomy were performed using standard procedures. The aqueous drainage devices used were the Baerveldt (Abbott Medical Optics, Santa Ana, California, USA) or Molteno implant (Molteno Ophthalmic Ltd, Dunedin, New Zealand) as a single procedure.
Statistical Analysis
All the statistical analyses were performed in SPSS Statistics (Version 21, IBM Corporation, Armonk, New York). Continuous data were reported using median and interquartile range (IQR) or mean and standard deviation. Visual acuity was converted into logMAR values and Spearman correlation coefficients were calculated to assess the relationship between age at diagnosis and visual acuity. Categorical data were analyzed with the Pearson χ 2 test. The Kaplan-Meier survival analysis was used to construct a time-to-progression curve. Time to progression of glaucoma was defined as the time from last angle surgery to the time resulting in non–angle surgery. Patients who did not experience progression over the duration of the study were censored at the date of last follow-up. Patients were often placed on topical or systemic glaucoma medications during the course of their treatment; this was not analyzed in this study. A P value of less than .05 was considered statistically significant.
Results
Demographic Data
During the 23-year study period, 152 eyes (97 patients) were identified with a diagnosis of primary congenital glaucoma, which averaged to 6.6 eyes (4.2 patients) per year. Thirty-five eyes (27 patients) were excluded owing to less than 1 year of follow-up or lack of data. Of the 27 patients, 15 had inadequate data, in that their original treatment had been overseas or elsewhere where we were unable to gain access to records or the records were so old that we could not find the previous notes pertaining to their original treatment, and 12 had less than 1 year of follow-up, which made them ineligible for the study. This was a mixture of patients who had just started care and those who had presented only once.
This left 117 eyes (70 patients) undergoing surgery for primary congenital glaucoma in our study. Of these, 47 patients had bilateral disease and 23 unilateral. Both right and left eyes and male and female patients were affected equally. The median follow-up was 7.0 years (range 1.0–22.8 years). Of the 117 eyes, 92 eyes (78.6%) were followed for greater than 5 years, 63 eyes (53.8%) greater than 8 years, 54 eyes (46.2%) greater than 10 years, and 28 eyes (23.9%) greater than 15 years ( Table 1 ). This included a large cross section of ethnic groups, including children with European-, Indian-, and Middle Eastern–derived backgrounds.
| All patients (n = 70) | |
| Sex, n (%) | |
| Male | 35 (50.0%) |
| Female | 35 (50.0%) |
| Laterality | |
| Unilateral | 23 (32.9%) |
| Bilateral | 47 (67.1%) |
| All eyes (n = 117) | |
| Median (IQR) age at diagnosis (d) | 120 (56–214) |
| Age at diagnosis, n (%) | |
| Birth | 7 (6.4%) |
| <3 mo | 33 (30.0%) |
| 3–6 mo | 39 (33.3%) |
| >6 mo | 38 (32.5%) |
| Median (IQR) age at first surgery (d) | 136 (73–220) |
| Median (IQR) age at first angle surgery (d) (n = 110) | 125 (71–210) |
| Median (IQR) age at first trabeculectomy (y) (n = 7) | 5.3 (4.3–6.1) |
| Years of follow-up, median (min-max) | 7.0 (1.0–22.8) |
| Eyes undergoing angle procedure as first operation (n = 110) | |
| First procedure | 110 (100.0%); 67 successful (60.9%) |
| Second procedure | 43 (39.1%); 23 successful (53.5%) |
| Third procedure | 20 (18.2%); 11 successful (55.0%) |
| Fourth procedure | 7 (6.4%); 0 successful |
| IOP results, all eyes (n = 117) | |
| IOP at final review (mm Hg), median (IQR) | 14 (12–16) |
| IOP >21 mm Hg at last follow-up, n (%) | 6/108 b (5.6%) |
a Total of 117 eyes with primary congenital glaucoma (70 patients), 110 eyes undergoing angle procedures (66 patients).
The median age at diagnosis was 120 days (IQR 56–214). The median IOP at final review was 14 mm Hg (IQR 12–16 mm Hg). Six of the 108 eyes (5.6%) available for analysis at final follow-up had an IOP >21 mm Hg. The final IOP for 8 eyes was not known and 1 eye was enucleated.
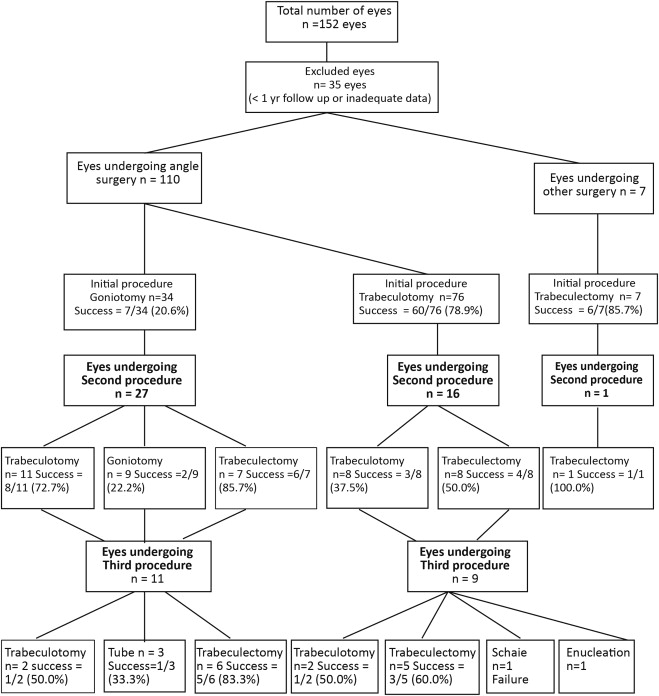
Surgery Treatment Algorithm
The surgical treatment algorithm ( Figure 1 ) describes the treatment paths and the relevant success rates. Trabeculotomy was far more common than goniotomy as a primary procedure (76/110 eyes, 69.1%). Thirty-four eyes (34/117, 29.1%) were treated medically before their first surgery. A single trabeculotomy (120 degrees angle opening) was successful in 60 of 76 eyes (78.9%). A single goniotomy (120 degrees angle opening) was successful in 7 of 34 eyes (20.6%). The median age when the first angle surgery (trabeculotomy or goniotomy) occurred was 125 days (IQR 71–210 days). Primary trabeculectomy was conducted in 7 eyes, with IOP successfully controlled in 6. All of these trabeculectomies were augmented with either 5-fluorouracil or mitomycin C. The median age for patients undergoing trabeculectomy as a primary/initial procedure was 5.3 years (IQR 4.3–6.1 years). Trabeculectomy bleb wound healing and suture manipulation were managed depending on the child’s cooperation. Children who could not tolerate slit-lamp management would have a further examination under anesthetic to modulate the trabeculectomy bleb healing.
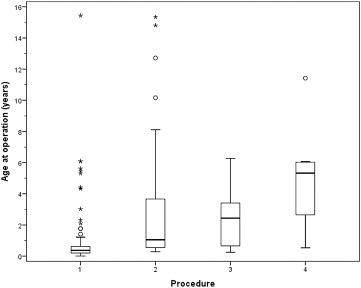
Distribution of Age for Each Operation
The distribution of age for each procedure was reviewed ( Figure 2 ). In the first year of life, there were 99 primary angle procedures, 20 secondary angle procedures, and 4 tertiary angle procedures. After the initial angle surgeries within the first year of life, the third procedure occurred at a median age of 2.4 years (IQR 0.6–3.8 years) and the fourth procedure occurred at a median age of 5.3 years (IQR 2.5–6.1 years). Five operations were conducted in 3 eyes and 6 procedures in only 1 eye. Only 7 of the 192 operations (3.6%) were performed after the age of 8 years ( Figure 3 ), of which 5 of the 7 occurred around puberty (12.9–15.7 years) ( Table 2 ).

| Patient | Ageat at Dx | Operation 1 | Operation 2 | Operation 3 | Operation 4 | Operation 5 | Operation 6 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at Sx | Sx | Age at Sx | Sx | Age at Sx | Sx | Age at Sx | Sx | Age at Sx | Sx | Age at Sx | Sx | ||
| 1 | 1.8 y | 1.8 y | Gonio | 15.6 y | Trab + MMC | ||||||||
| 2 | 0.6 y | 0.6 y | Gonio | 10.3 y | Trab + MMC | ||||||||
| 3 | 0.6 y | 0.6 y | Gonio | 15 y | Trab + MMC | ||||||||
| 4 | 0.6 y | 0.6 y | Trab | 12.9 y | Trab + MMC | ||||||||
| 5 | 0.4 y | 0.4 y | Gonio | 8.2 y | Gonio | 0.9 y | Trab | 11.6 y | Trab 5FU | ||||
| 6 | 0.3 y | 0.3 y | Gonio | 0.4 y | Gonio | 0.5 y | Molteno | 6 y | Deroof Molteno | 7.6 y | Trab 5FU | 22 y | Cyclodiode |
| 7 | 12.5 y | 15.7 y a | Trab + MMC | ||||||||||
a Previously treated medically; other eye goniotomy age 18 months.
Angle Surgery Success Rates
Up to 360 degrees of angle surgery was conducted over 1–3 sessions. Angle surgery success was obtained in 83 of the 110 eyes (75.5%). Kaplan-Meier analysis showed a success rate of 92% at 2 years, 86% at 4 years, 84% at 6 years, and 75% at 10 years ( Figure 4 ). Age at presentation and its effect on success or failure of surgery was also investigated—in particular, whether children who underwent their first surgical procedure prior to 3 months of age were more likely to fail angle surgery and need more operations than a child who has his or her first surgery after this date. No statistically significant relationship was found between age (<3 months, 3–6 months, >6 months) at first operation and success or failure of angle surgery ( P = .94, Table 3 ). Eighty-seven percent of the <3 months age group needed only 1 angle surgery to be successful compared with 79% and 74% for age 3–6 months and age >6 months, respectively ( P = .43). Eyes with the first operation occurring at birth (n = 7), defined as less than 1 week of age, were compared with those with the first operation occurring at 1 week to 3 months of age (n = 33). For the eyes operated on at birth 6 of 7 eyes had successful angle surgery. In these 6 cases only 1 angle surgery operation was needed. The remaining eye required 2 procedures: 1 trabeculotomy at birth and a further trabeculectomy and mitomycin C at age 3.3 years. Although the numbers are small, these results suggest that operation at birth was not associated with a requirement for an increased number of operations.