8
Prevention of Complications in Stapes Surgery
Surgery for otosclerosis is simple in concept, yet good outcomes rely on successful execution of the fine details and the avoidance of complications. There are many descriptions of operative procedures for otosclerosis in the literature, including those by this author.1 These generally describe the basic elements of the operation in a sequential manner but do not focus on the particular critical points that are high risk for complications, nor do they describe how to avoid certain pitfalls. This chapter discusses the times during surgery in which the potential for complications is higher and proffers some thoughts on how to avoid them. Table 8–1 considers the potential difficulties as well as some solutions.
The procedure described here is the laser stapedot-omy, which itself reduces the probability of complications relative to conventional stapedotomy. The reader is referred elsewhere for a description of the laser stapedotomy procedure and the basic procedural steps.1 This chapter focuses on specific areas of preparation and technique to avoid complications.
■ Preoperative Preparation
The old saying “An ounce of preparation is worth a pound of cure” is extremely pertinent to avoidance of complications in stapes surgery. Preparation of the microscope, laser parameters, and patient as well as instrument care and surgical team training are extremely important in reducing complications. Many complications become more probable as a result of inadequate preparation before the first incision is made. The safety of an airplane flight does not begin with takeoff: it begins with the design of the airplane, the training of the support crews, the adequacy of maintenance systems, fuel checks before takeoff, and a well-trained and rested pilot. It is the surgeon’s responsibility to oversee all aspects of the preparation. The reader is encouraged to review the sections on preoperative preparation in the referenced chapter at the end of this article.
■ Patient Positioning, Draping, and Comfort
The patient’s head should be positioned to the surgeon’s side of the table so the surgeon does not add further stress by operating with outstretched arms. I prefer not to use a headrest, allowing the patient’s head to be dropped back with the chin turned toward the contralateral shoulder. This positions the external canal optimally and facilitates the entire procedure.
Another bit of patient preparation that provides comfort to the sedated patient is the use of a draping bar and face fan. After prepping the auricle and periauricular area, a drape is placed over the area with the auricle exteriorized through the hole in the drape. This drape is placed over an L-shaped bar that is fixed in the rail attachment of the operating table (Fig. 8–1).Attached to the bar is a small, low-volume desk fan that provides a cooling breeze to the patient’s face during the procedure. The plastic drape forms a canopy, allowing the patient to see from under the drape and reducing the feeling of claustrophobia, and provides a visual pathway for the circulating nurse to confer with the patient during the procedure, if needed.
| Problem | Prevention/Treatment |
|---|---|
| Analgesia and hemostasis | Effective canal injection in a classic quadratic fashion |
| Short tympanomeatal flap | Maximum flap depth at 10 O’clock position in right ear If flap does not adequately cover scutal defect, place temporalis fascia to bridge gap |
| Tympanic membrane perforation | Raise tympanomeatal flap by pushing with knife always on bone Separate the fibrocartilaginous annulus of the tympanic membrane from the annular sulcus of the tympanic bone |
| Chorda tympani nerve trauma | Begin curetting of scutum lateral to scutal edge Curette away from the chorda tympani nerve |
| Confirmation of disease | Inspect round window for patency Palpate medial surface of malleus manubrium Palpate lateral surface of incus to assess incus and stapes mobility Palpate stapes and note light reflex of the stapes annular ligament |
| Short prosthesis | Measure distance from medial end of long process of incus to stapes footplate, then add 0.5 mm to determine optimal length of prosthesis |
| Avoiding fracture of the lenticular process | Locate plane of joint by palpating incus in an anterior-posterior direction to see light reflex Incise joint capsule |
| Prevention of facial nerve damage | Study the facial nerve, its position, and status of fallopian canal |
| Perilymph protection | Maintain hemostasis prior to work on stapes footplate Change suction tip to a 24, 26, or 28 gauge Place prosthesis through the fenestration slowly to avoid a rapid pressure change in the vestibule Prevent heating of perilymph by spacing laser pulses 5–10 seconds apart |
| The binding prosthesis | If prosthesis does not move easily, push it anteriorly; resistance implies it is in the fenestra;lack of resistance implies it is out of the fenestra |
| Tympanic membrane collapse onto incus and prosthesis | Place tympanomeatal flap into anatomical position |
■ Analgesia and Hemostasis
Adequate analgesia and hemostasis are extremely important in stapes surgery. Any significant bleeding while working in the oval window is an invitation to disaster. To optimize hemostasis in the canal, use 2% xylocaine with 1:20,000 epinephrine solution in a classic quadratic injection and follow that with a special anterior canal injection. The anterior canal injection is done by orienting the bevel of a 1.5 in., 27 gauge needle parallel to the anterior canal bone, inserting it below the skin and slowly injecting a small amount of the solution so that it migrates toward the anterior sulcus area (Fig. 8–2). This not only provides analgesia to the medial third of the anterior canal wall (a must in tympanoplasty) but also tends to reduce the bleeding sometimes encountered in the medial portion of the inferior leg of the tympano-meatal incision.
Although it may seem to be a trivial part of the procedure, the tympanomeatal incision is an important part of avoiding complications. The appropriate incision helps prevent a short flap situation (described in later text) but, possibly more importantly, can provide better hemostasis throughout the operation. Through as large an oval-beveled speculum as possible, incisions defining the flap are created. The initial incision is made with a sickle knife just lateral to the inferior annulus of the tympanic membrane at the 6 o’clock location and brought laterally along the floor of the canal ~4 mm. A second incision is made with a 2 mm round canal knife beginning at the lateral extent of the initial incision and extending in a curvilinear manner, first posteriorly and then anterosuperiorly until it terminates~ 2 mm above the pars flaccida. This second incision is made in multiple small segments beginning inferiorly. Each segment is composed of an initial crushing application of the knife into the canal skin and a subsequent cutting action that connects that small segment with the previously cut segment. The crushing portion of this action seems to impart additional hemostasis, particularly in the thicker vascular strip area. An additional advantage of making this in multiple small segments is that it eliminates the tendency of the tissue to tear.
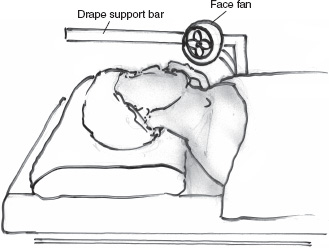
FIGURE 8–1 The drape support bar and face fan.
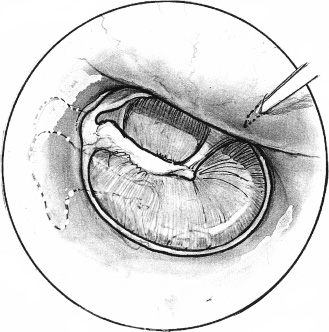
FIGURE 8–2 The anterior canal injection.
■ Prevention of the Short Flap
Although not a complication of catastrophic proportions a short tympanomeatal flap can add potential risk to the procedure as well as increased time to correct it. These occur by not allowing adequate canal length on the tympanomeatal flap in the area where the scutum is to be curetted. The maximum flap depth should be at ~10 o’clock on the annular clock (right ear) and should be ~4 mm to accommodate for the bone removed to visually access the oval window area. Should the tympanomeatal flap not cover the curetted scutal area, it can be corrected by placing a piece of temporalis fascia medial to the short flap and bridging it to the posterior canal bone.
■ Prevention of Tympanic Membrane and Canal Skin Perforations
A not uncommon complication of otosclerosis surgery is perforation of the tympanic membrane upon elevation of the tympanomeatal flap. Most common among inexperienced surgeons, it occurs from trying to elevate the skin flap and annulus from the bone rather than separate the skin flap from the canal bone and separate the fibrocartilaginous annulus from the bony annular sulcus. By pushing on the soft tissue with a round knife or elevator one can slide over the annulus and penetrate the knife or elevator into the tympanic membrane just anterior to the annulus. This can be easily avoided by never taking the knife off the bone surface. The flap will naturally elevate when it is separated. If one always keeps the knife on the bone surface, develops the separation on a relatively broad front, and never allows soft tissue beneath the blade, one cannot perforate the tympanic membrane. The important point is to recognize the annulus and annular sulcus, depress the knife edge into the sulcus, and separate the fibrocartilaginous annulus from the sulcus. Should a tympanic membrane perforation occur, inject a small amount of analgesic solution into the lower temporalis fascia area, harvest a small piece, and place it medial to the perforation. Bring it onto the bony posterior canal wall and bolster it with a small amount of Gelfoam¯ in the posterior tympanum.
■ Prevention of Damage to the Chorda Tympani Nerve during Tympanomeatal Flap Elevation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


