Medial rectus injury is an uncommon but often devastating complication of functional endoscopic sinus surgery. Prevention of these types of injuries is predicated on a thorough preoperative assessment of the position and integrity of the medial orbital wall coupled with excellent surgical technique. The use of powered instrumentation has led to more severe injuries and thus should be used with caution near critical structures such as the lamina papyracea. Early recognition and management of medial rectus and associated orbital injuries is critical to improve outcomes and prevent associated complications. Despite optimal surgical and medical interventions, the prognosis is relatively poor and patients should be counseled that the primary goal of these interventions is to reestablish a binocular single visual field.
Orbital penetration represents a rare but serious complication of functional endoscopic sinus surgery. The proximity of the orbit to the surgical field coupled with the relatively thin bony partition of the lamina papyracea make this region particularly vulnerable to iatrogenic injury. Although violation of the medial orbital wall places the entire orbit at risk, the medial rectus represents the most commonly injured extraocular muscle during sinus surgery. Consequently, early recognition of medial rectus and associated orbital injuries is critical, as immediate diagnosis and intervention may have a dramatic effect on the long-term outcome of these patients.
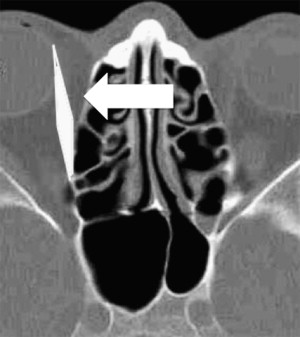
The lamina papyracea comprises the medial orbital wall and is bounded laterally by orbital periosteum. This layer, which may also be referred to as periorbita, completely surrounds a layer of extraconal periorbital fat that encapsulates the orbit. Medially, this orbital fat is bounded by a fascial layer that ensheaths the extraocular musculature known as Tenon’s capsule. The medial rectus muscle originates from the annulus of Zinn and travels along the medial aspect of the globe to insert on the sclera. As the muscle travels anteriorly, it takes a slightly lateral course away from the lamina papyracea ( Fig. 1 ). The medial rectus is innervated by the oculomotor nerve that traverses the superior orbital fissure and arborizes, giving off branches to the lateral aspect of the muscle.
Preoperative prevention
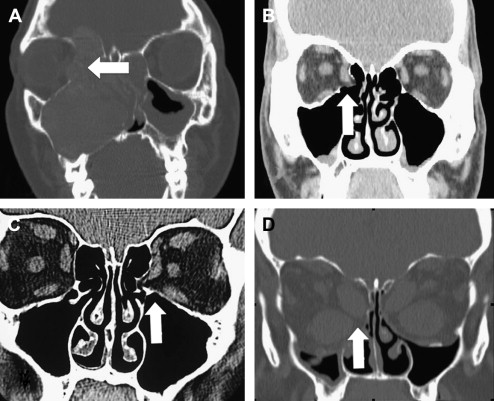
Prevention of medial rectus injury relies on a comprehensive history and physical examination that should include a detailed analysis of the preoperative imaging. A history of prior surgery, maxillofacial trauma, sinonasal neoplasm, expansile inflammatory lesion, or primary orbital pathology should raise the suspicion of a potential preexisting dehiscence of the lamina ( Fig. 2 ). Detailed analysis of the preoperative imaging should include an assessment of the morphology and integrity of the lamina including the position of ethmoid vasculature, complex sinus anatomy, and the presence of any prolapsed orbital contents within the sinonasal cavity. The presence of sinonasal disease may lead to obscuration of the lamina secondary to soft tissue and bleeding, and thus an accurate preoperative knowledge of its position allows the surgeon to safely proceed with the dissection. Image guidance may also be used to aid in the intraoperative identification of the medial orbital wall; however, it should not be used a substitute for rigorous preoperative planning.
Intraoperative prevention
Intraoperatively, the lamina should be identified early and skeletonized to provide a consistent anatomic landmark. When dissecting along the lamina, the force should be directed anteriorly, parallel to the face of the lamina, to prevent inadvertent penetration. When using powered instrumentation, the cutting aperture should always be visualized to ensure that tissue aspiration is highly controlled. The head of the debrider should never be pressed against the lamina but rather should remain several millimeters away, allowing the soft tissue to be pulled into the instrument. In regions of particular concern, the instrument should be activated intermittently to prevent the rapid suction and debridement of large volumes of tissue at any given time. During procedures in which the lamina is deliberately violated, such as during an orbital decompression, care should be taken to maintain integrity of the periorbita during the bony dissection ( Fig. 3 ). The bone is removed in an anterior to posterior direction, taking advantage of the wider extraconal periorbital fat layer between the medial rectus and lamina in the anterior ethmoid cavity. During incision of the periorbita, the medial rectus may be visualized and the incision should be made superficially and, if possible, away from the muscle itself.
The overall incidence of medial rectus injury during sinus surgery is difficult to accurately determine because of its low frequency. One of the largest published series gathered a total of 30 cases from 10 large centers and reported an incidence of 1 of 735 over a 5-year period. Although the incidence is low, when orbital injury does occur, the medial rectus is the most common extraocular muscle involved, followed by the inferior rectus.
Intraoperative prevention
Intraoperatively, the lamina should be identified early and skeletonized to provide a consistent anatomic landmark. When dissecting along the lamina, the force should be directed anteriorly, parallel to the face of the lamina, to prevent inadvertent penetration. When using powered instrumentation, the cutting aperture should always be visualized to ensure that tissue aspiration is highly controlled. The head of the debrider should never be pressed against the lamina but rather should remain several millimeters away, allowing the soft tissue to be pulled into the instrument. In regions of particular concern, the instrument should be activated intermittently to prevent the rapid suction and debridement of large volumes of tissue at any given time. During procedures in which the lamina is deliberately violated, such as during an orbital decompression, care should be taken to maintain integrity of the periorbita during the bony dissection ( Fig. 3 ). The bone is removed in an anterior to posterior direction, taking advantage of the wider extraconal periorbital fat layer between the medial rectus and lamina in the anterior ethmoid cavity. During incision of the periorbita, the medial rectus may be visualized and the incision should be made superficially and, if possible, away from the muscle itself.




