Vitreous surgery has been applied successfully to a wide spectrum of ocular diseases. The complex set of biologic, systemic risk, technique, and technology considerations confronting the surgeon creates a difficult decision-making environment. Rather than emphasizing a search for good prognosis or easy cases, the goal must be to avoid bilateral or irreversible visual disability. Many potential vitreous surgery patients have profound socioeconomic problems as a result of blindness and/or systemic disease. A significant attempt to understand the patient’s medical and socioeconomic situation is essential to effective and compassionate health care delivery.
Since the introduction of the first edition of this book, the scope of vitreous microsurgery has expanded greatly. Whereas vitrectomy surgery was initially considered only on the most advanced and complicated clinical situations, we can safely perform 25-gauge vitrectomy with minimal discomfort to the patient and, most importantly, with low surgical complication rates. This allows the use of vitrectomy for epimacular membranes (EMMs) with relatively good preoperative visual acuity, relieving patients’ symptoms and improving functional outcomes in ways that would not have been possible in decades past.
The surgeon must examine both eyes personally to reach the best clinical decision. The surgeon must develop an open, direct, and warm relationship with the patient before surgery can be considered. It is probably better to discuss specific statistical results of surgery on similar patients rather than to discuss the details of a specific methodology. Rather than using qualitative words such as “excellent” or “poor,” using a percentage success rate is a more meaningful way to communicate. The frequency of the most important complications should be mentioned as well as the range and mean of postoperative vision in functional and numeric terms. All available family members and the surgeon’s secretary, technician, assistant, or nurse should witness this conversation. A complex, legalistic permission document is far less important than meaningful, compassionate, understandable, personal communication with the patient. The patient should be informed about postoperative positioning, pain, medications, operating time, type of anesthesia to be used, the requirement for postoperative examinations, and limitations on activity.
The surgeon must take personal responsibility for obtaining financial support for the economically disadvantaged patient and act as a consumer advocate concerning facility fees. It is unconscionable to turn away a patient or permit the facility to do so because of the patient’s financial status.
It is the surgeon’s responsibility to organize the scheduling process so that the preoperative assessment or logistical/bureaucratic delay does not affect the prognosis. Waiting lists are highly inappropriate for patients with significant visual problems. If surgery is performed within a few days of the original examination, the surgeon will be more acutely aware of significant aspects of the patient’s history, findings, and imaging during surgery.
SYSTEMIC FACTORS
Age
Age is a consideration at both extremes of the timeline. While age cannot be used as an arbitrary criterion, it is clear that both the neonate with severe pulmonary problems and the elderly patient with multisystem systemic disease have higher anesthesia risks. Surgery on the premature infant can be delayed until pulmonary function and body weight increase, allowing safer anesthesia. Most vitreoretinal surgery today is performed under local anesthesia with anesthesia monitoring, but children and certain adults require general anesthesia.
Sensory deprivation from poor vision may contribute to disorientation and agitation in certain elderly patients. Unilateral visual loss is well tolerated in many elderly patients because of less demanding occupational and recreational needs. While it is the surgeon’s obligation to determine ocular status and needs, medical consultants and anesthesia team can help determine and manage systemic risk.
Diabetes
As diabetes is common in vitrectomy patients, the vitreous surgeon must be quite familiar with the complications of this multisystem disease. An individualized approach is superior to arbitrary surgical criteria. The presence of a systemic infection is a contraindication to vitrectomy. All ocular conditions except endophthalmitis and severe glaucoma can wait until a systemic infection has been treated.
End-stage renal disease decreases life span and creates difficult socioeconomic as well as medical problems. The stable transplant patient can undergo successful vitrectomy, although immunosuppressant drugs create increased infection risk, especially with general anesthesia. The dialysis patient has increased risk with general anesthesia risk and may have increased bleeding with vitrectomy. While surgical conservatism is indicated for patients with end-stage renal disease, many carefully selected patients can benefit from vitrectomy.
Cardiopulmonary Disease
Specific guidelines in the area of cardiopulmonary disease again must be replaced by an individualized approach with reliance upon medical and anesthesia consultations. Although local anesthesia is safer than general, there remains some risk associated with local anesthesia, pointing to the need for careful medical assessment and a monitored approach by an anesthesiologist or a certified registered nurse anesthetist (CRNA) with anesthesiology supervision. Pulse oximetry, EKG, continuous blood pressure monitoring, and frequent blood glucose assessments are mandatory.
The recent trend of vitrectomy surgery moving from the hospital setting, where subspecialized consultants are readily available, to the ambulatory surgery center requires the surgeon to be aware of the anesthesia risk of each patient. We feel that high-risk patients require hospital-based surgeries.
Obesity and Obstructive Sleep Apnea Syndrome
A major practical problem that has become more prevalent in the recent years is morbid obesity and associated obstructive sleep apnea. These patients require surgical tables that can withstand extreme weights. In addition, surgical bed designs that have an off-centered pedestal to allow room for the surgeon’s legs can tip over with morbidly obese patients. These patients may not be able to lie flat during surgery due to orthopnea, requiring either delaying elective surgery until the patient loses enough weight to safely undergo the procedure or operating on patients on uncomfortable angles for the surgeon if the bed is positioned with the head elevated enough for adequate ventilation.
Pickwickian, morbidly obese, patients can become hypoxic postoperatively. If an inexperienced certified nurse assistant increases the concentration of inspiratory oxygen to improve orthopnea, the oxygen-driven respiratory drive (since these patients have chronic hypercapnia that desensitizes the CO2 chemoreceptors) can be suppressed and lead to immediate postoperative hypoxia.
OCULAR FACTORS
Examination of the vitrectomy patient embodies the same steps, but with different emphasis, that required for other ophthalmic specialties. A problem-oriented approach with emphasis on specific factors that have a high impact on decision making is more effective than a nonstructured, “routine” examination.
Visual Function Testing
Visual function testing can be the most difficult component of previtrectomy evaluation unless approached properly. Careful, precise measurement of visual acuity is more relevant than an array of laboratory tests.
Visual Acuity
The inherent subjectivity of visual acuity testing demands random presentation of stimuli, multiple repetitions, and sophisticated examiners. Total coverage of the other eye with the patient’s palm, not fingers, pressed against the bridge of the nose is essential to determine light perception. Specifically, the examiner cannot ask, “Can you see the light?” but rather should say, “Tell me when the light goes on and off.” The patient must describe the direction of randomly presented motion when testing for “hand motion.” Multiple repetitions increase reliability because of problems stemming from patient guessing. The patient’s neurological/psychological status and educational level may interfere with accurate testing.
The light perception determination is of particular significance because patients without light perception should never have vitrectomy unless it is clearly understood that the procedure is to prevent the spread of infection or, in rare instances, for cosmetic preservation of the globe. Dense opaque media requires a bright testing light such as that from an indirect ophthalmoscope at 7.5 volts.
The finger-counting method is fraught with error because of the great variance in finger size, position, color, and illumination. It is preferable to use a printed, 20/200-sized “E” on a white card. This can be presented in random orientation with multiple repetitions, and the distance can be measured to determine acuity as a fraction (e.g., 1/200). A patient with 1/200 vision typically cannot see well enough to walk, while a 5/200 patient typically is ambulatory, and an individual with 9/200 vision can read large print with magnification. Placing all these patients into the finger-counting category is misleading.
Flat screen display, computer-driven vision testing devices are accurate and rapid ways of testing visions of 20/400 or better and can replace more traditional projector charts (1). The printed charts with special illumination used by the Early Treatment of Diabetic Retinopathy Study (2) are very accurate but cumbersome.
Current refraction must be in place for visual acuity testing at the 20/400 or better level. Pinholes are difficult for retinal patients to use and may reduce contrast sensitivity in the presence of retinal disease, resulting in underestimating visual function. Near vision testing is essential because of hereditary myopia and induced myopia from nuclear sclerosis and encircling buckles.
Contrast Sensitivity
The ability to detect changes in contrast is a significant measure of macular function. Not infrequently a patient’s perception of visual changes and visual recovery is more dependent on contrast sensitivity than on visual acuity, since most real world scenarios involve reduced contrast. We do not routinely perform formal contrast sensitivity testing on our patients. On the other hand, an adequate history from the clinician can gather information regarding visual function in reduced light that can help orient surgical decision making in patients with macular disease, even when formal contrast sensitivity testing is not performed.
Metamorphopsia
Amsler grid evaluation can help explain a patient’s visual complaints and can assist in the recommendation of surgery in patients with EMMs and macular striae. No objective evaluation has been developed for metamorphopsia analysis, but adequate history and proper Amsler grid testing can demonstrate the presence of visual distortion that may be visually disabling and that can be improved with surgery. We do not recommend using only visual acuity testing for determination of need for macular surgery, since many high-functioning patients with relatively good visual acuity can have disabling, correctable metamorphopsias.
Projection and Field Testing
Marked opaque media creates light scatter and might cause a false impression of being able to perceive the direction of projection, while recent retinal detachments can have normal projection. Occasionally, an advanced glaucoma patient with opaque media will respond only in the temporal field, but frequently, the patient indicates a larger field due to light scattering.
Entoptic Phenomenon
The patient should be able to see the shadows of the retinal vessels if a focal light source (transilluminator) is rubbed against the closed lids. Care must be taken because these lights generate heat. If the light source is turned on after skin contact is made and the skin contact is never broken, heat dissipation is usually adequate. Many patients report the shadows as appearing like leaves or cracks, and there appears to be excellent correlation with attachment of the posterior 30 degrees of retina. However, many patients with normal retinas cannot respond in a positive manner to this test, greatly reducing its value.
Color Discrimination
Patients with recent total retinal detachments and many long-term, low detachments have excellent color discrimination with large targets. Because 90% of the cones are extramacular, patients with large macular scars have normal color function with large targets. Standardized color testing methods are highly dependent on 20/200 or better visual acuity, negating their value in opaque media cases. Hemorrhagic vitreous acts as a red filter, altering color discrimination.
Maddox Rod
Detection of the orientation of a Maddox rod is said to correlate with good postoperative function in opaque media cases. Patients with recent total detachments and advanced glaucoma can provide accurate answers to this test, thereby eliminating its value. Certain inoperable patients respond positively to this test, further decreasing its value.
Two-Point Discrimination
Two-point sources of light (transilluminators) can be moved laterally, initially touching and then progressing to 1-m distance. Reporting of “two lights” at close distance (< 2.5 cm) corresponds with better retinal function. Patients with recent or partial retinal detachments can respond normally to this test, and light scatter can cause false negatives, dramatically reducing the value of this test.
Laser Interferometry
Dense cataracts and vitreous hemorrhage prevent visualization of laser interference fringes. Although laser interferometry can be used with minimally opaque media, it measures vernier-type acuity, with only moderate correlation with Snellen acuity.
VALUE OF PSYCHOPHYSICAL TESTING
In general, patients with a positive response to all of the above psychophysical tests show better postoperative results and, conversely, those with a negative response typically achieve poor visual function (3). The subjective nature of these tests and the many instances of false positives and false negatives greatly decrease their value. Examiners may use these methods to seek out good prognosis cases, some of which do not really require surgery, but a negative response to these tests frequently indicates an operable retinal detachment demanding immediate vitrectomy. At present, the authors use only visual acuity testing to assess function.
PUPIL TESTING
An afferent pupillary defect discovered with the swinging flashlight test can be of great value in preoperative evaluation. Glaucoma, retinal detachment, ischemic optic neuropathy, and optic nerve trauma are the most frequent causes of an abnormal response. If one afferent system (retina and optic nerve) and one efferent system (third nerve, ciliary ganglion, and iris sphincter) are intact, the test can have value. Bilateral iris disease eliminates the utility of this test. As in psychophysical methods, a negative response may indicate an operable retinal detachment rather than an inoperable eye. Large macular disciform scars can cause a moderate afferent pupillary defect.
SLIT LAMP EXAMINATION
A problem-oriented examination is far more effective than a “routine” examination. Specific, subtle details can have a major impact on presurgical decision making.
Cornea
Epithelial erosions are common in diabetics and some patients who have had recent surgery. Corneal edema may preclude the excellent visualization required for vitrectomy. Unless vitreous-corneal touch, lens-corneal touch, or glaucoma to be treated by vitrectomy is present, the net effect of vitrectomy will be to further decrease endothelial function. Guttata and low endothelial cell counts indicate the possibility of postoperative corneal edema and suggest more rigid vitrectomy indications. Blood staining, scarring, or edema, if very extensive, is an indication for penetrating keratoplasty, Descemets stripping endothelial keratoplasty (DSEK), or endoscopic surgery. Vitrectomies can often be performed by working around central corneal or lenticular opacities.
Iris-Anterior Chamber
The extent of pupillary dilation is important if the lens is to be retained. On occasion, a clear lens lensectomy will be necessary in an emergency vitrectomy only to allow the removal of anterior chamber or perilenticular blood or fibrin.
Iris and trabecular neovascularization is subtle in its early stages but of extreme importance. The iris surface overlying the sphincter should be examined using a magnification of 24× to 40× prior to dilation. Large vessels, ectropion uveae, and peripheral anterior synechia are late changes and are not required for a diagnosis of iris neovascularization. Capillaries on the iris or trabecular surface indicate activity, while larger vessels will persist after regression of the capillary activity. Examiners with red-green color discrimination problems find it difficult to recognize iris neovascularization and make this condition a negative factor in the decision to become a vitreoretinal surgeon. Dilated stromal vessels or exposed iris vessels due to prior cataract surgery or certain lens implants are usually quite easy to differentiate from iris neovascularization. Topical phenylephrine decreases the visibility of iris neovascularization due to vasoconstriction.
While significant trabecular meshwork neovascularization can be present with minimal iris neovascularization, this is somewhat unusual. Because gonioscopy is time-consuming and may damage the corneal epithelium, the iris is usually used as an indicator of anterior segment neovascularization, but gonioscopy detection of trabecular meshwork neovascularization is the most sensitive and relevant indicator of vascular endothelial growth factor (VEGF) levels in the anterior chamber. Cells and flare are present in the anterior chamber of many patients requiring vitrectomy and are at most a relative contraindication. Fibrin syndrome usually contraindicates all but emergency vitrectomies for endophthalmitis.
Lens Opacities
Blood or pigment on the anterior or posterior surface of the lens or lens implant may necessitate lens or implant removal for adequate visualization. Many vitreous hemorrhage cases have posterior subcapsular cataracts. The lens should be removed if significant posterior subcapsular changes are present to provide excellent surgical visualization and because these changes virtually always rapidly progress postoperatively. Cortical changes, if moderate, can be tolerated. Moderate nuclear sclerosis will permit adequate visualization and progresses more slowly than posterior subcapsular opacities following vitrectomy.
Intraocular Pressure
Indentation (Schiotz) tonometry is generally inadequate and outdated for the measurement of intraocular pressure (IOP). Applanation tonometry is adequate but is inaccurate with irregular corneas. The Tonopen is more accurate with irregular corneas and ocular rigidity problems, causes less corneal trauma, and does not result in fluorescein in the tear film and anterior chamber. Tonopen tonometry is easier than applanation tonometry for patients with marked blepharospasm and can be used with a contact lens in place.
Low pressure (hypotony) has an undeserved bad reputation. Most low pressures are due to reparable wound leaks or reparable retinal detachments with increased uveal-scleral outflow. Low pressure does not cause phthisis; rather, phthisis may cause hypotony. Phthisis might best be defined as ocular collapse from a cyclitic membrane. In no instance should hypotony delay an otherwise indicated vitrectomy. Ciliary body shutdown is an overrated, theoretical cause of hypotony, which occurs only after massive destruction of the ciliary epithelium by cryopexy, ultrasound, laser, or infection.
Elevated IOP has many causes, and a complete discussion is beyond the scope of this book. Pupillary block, hemolytic (erythroclastic), and phacolytic glaucoma are treated by vitrectomy. Neovascular glaucoma (NVG) can be made worse by vitrectomy unless anti-VEGF agents, panretinal photocoagulation (PRP) or retinal reattachment can be accomplished during the procedure, thereby decreasing VEGF levels.
SLIT LAMP BIOMICROSCOPY OF THE RETINA
An understanding of vitreoretinal anatomy and the forces acting on the retina is essential in the evaluation of potential vitrectomy cases. In large part, vitreous drawing is a useless exercise; the traction forces are evident from retinal contours and visibility of the vitreous is far better at the time of surgery. Small retinal breaks, macular edema, macular holes, EMMs, subretinal neovascular membranes, and subtle neovascularization are best observed with slit lamp biomicroscopy. Cloudy media decreases the value of slit lamp biomicroscopy. Plano-concave (flat, Goldman) contact lenses with antireflective coatings provide much better lateral resolution than 78- to 90-diopter (D) lenses and eliminate corneal asphericity. In addition, flat or three-mirror contact lenses provide better axial resolution, better depth of field, and improved stereopsis than 78- to 90-D lenses and wide-field contacts, although the noncontact lenses are easier to use and somewhat more comfortable for the patient.
INDIRECT OPHTHALMOSCOPY
An understanding of the vitreoretinal anatomy and the forces acting on the retina is a necessity in clinical decision making. The examiner cannot be a passive observer of vitreous “bands” but must grasp the concepts of the continuum of the anterior and posterior vitreous cortex (PVC) and the forces causing retinal contour changes.
The indirect ophthalmoscope is essential to vitreoretinal examination because of the stereopsis, wide field, and contrast obtained even with nonoptimal media. It should be used on its brightest setting (7.5 volts) in most instances. The 20-D lenses have greater light-gathering ability and increased contrast compared to the 28-D lenses, which are better for small pupils and gas bubbles. If possible, the pupil should be widely dilated, the room dark, and the examiner well dark-adapted. Continued dark adaptation, by keeping the entire examining unit dimly illuminated, is far more efficient than waiting for dark adaptation to occur during each examination. Noncognitive repositioning of the hand holding the condensing lens allows prism effect to enable peripheral viewing, reduced astigmatism, and viewing around opacities.
VITREOUS CONFIGURATION
The examiner must make a specific effort to look at rather than through the vitreous with the indirect ophthalmoscope. Much can be learned from the geometric configuration of opaque or semiopaque vitreous. A common tendency is for the clinician to give up and describe the opaque media case as “no view,” “no retinal detail,” or “red reflex.”
Vitreous consists of a three-dimensional (3D) matrix of collagen fibers suspended in hyaluronic acid. The normal shape of the vitreous is roughly spherical with a small anterior concavity for the lens. The continuity of the multilayered outer surface (cortex) is the most essential concept in developing an understanding of surgical anatomy. The vitreous base is not a space-occupying structure but a zone of adherence between retina and vitreous. The vitreous base represents a zone connecting the anterior vitreous cortex (AVC) and the PVC.
Posterior vitreous detachment (PVD or posterior vitreous separation) occurs in approximately 70% of the population and can be thought of as a normal process although it is a factor in many vitreoretinal problems. Cataract surgery and other anterior segment procedures such as refractive lens exchange, ocular trauma, vitreous, myopia, aging, and hereditary processes increase the likelihood of PVD. Syneresis is traditionally described as the development of cavities within the vitreous and vitreous “collapse,” which then causes separation from the internal limiting membrane (ILM) of the retina. A better way to think of PVD is that vitreous collagen becomes less adherent to certain parts of the retina, central vitreous collagen fibers cross-link and clump, and saccadic motion facilitates a separation from the retina. Cavities do not passively form in the vitreous. Collagen clumping creates this appearance. Collapse exerts minimal force because the vitreous collagen is nearly neutrally buoyant in hyaluronan and the high water content of vitreous.
Degenerative changes (syneresis), hemorrhage, inflammation, thermal effects, and cellular migration and proliferation can cause the shortening of vitreous surfaces, which is best termed “hypocellular vitreous contraction.” Dense hemorrhagic vitreous has been described as “organized” by many, while it should more correctly be termed “opacified.” “Organization” is a specific term applied to the proliferation of fibroblasts. It is usually observed only with severe ocular trauma or retinal necrosis.
Clear vitreous is fully capable of creating sufficient traction force to cause a total traction retinal detachment (TRD). Many examiners refer to “vitreous bands” in their analysis of vitreoretinal pathology. Discrete vitreous bands are markedly overemphasized and typically represent only a more opaque section of the continuous PVC. The clear contiguous portions of PVC often create a tremendous force on the retina, demonstrating that “band”-oriented vitreous description or surgical approach is useless.
As interaction between a few cells and the vitreous collagen fibers causes contraction, the PVC pulls away from the posterior retinal surface but remains adherent to the vitreous base. The vitreous is normally more adherent to the optic nerve head, macula, and retinal vessels. Abnormal adherence is common in areas of neovascularization, chorioretinal scarring, trauma sites, and prior photocoagulation. Further vitreous contraction will create a conical configuration of the PVC because of the posterior adherence areas. Epiretinal membranes (ERMs) may occur at the attachment sites but also occur independently of the vitreous in the form of proliferative vitreoretinopathy (PVR) star folds, EMMs, or the ridge or sheetlike ERMs seen in proliferative diabetic retinopathy and retinopathy of prematurity (ROP). Frequently, the vitreous will separate from the retinal surface in some areas, leaving scattered zones of adherence connected by the PVC. A large fenestration in the PVC may occur at the macula. Posterior vitreous separation is often accompanied by a Weiss ring, which is an elliptical condensation of PVC formerly adherent to the optic nerve head. Posterior vitreous separation is somewhat illusory in that an additional layer or layers of vitreous often remain adherent to the retina in the presence of an apparent PVD.
Saccadic motion of the eye and a change in head position can help differentiate between flaccid PVC with retinal adherence and taut PVC causing traction on the retina. Saccadically induced motion can create dynamic traction capable of creating a retinal break but incapable of causing TRD. The traction referred to in this book might more correctly be termed “static traction.”
The conical surface of the PVC in diabetic vitreous hemorrhages, TRDs, or penetrating trauma may have one or more apices created by zones of adherence. The most typical apex of the single point cone is the optic nerve. Two-point conical PVC surfaces are usually attached to the optic nerve and a vascular arcade (most frequently superotemporal). It is essential to understand that the PVC must bridge between these vitreoretinal attachment points. Nasal location of the apex of the conical surface usually precludes traction detachment of the macula. The apices can be acute angles or broad truncations of the conical PVC, indicating small or larger zones of adherence, respectively. If the vitreous is taut, the shape of the PVC apex can be thought of as a mirror image of the shape of the traction detachment. Single acute angle apices result in simple conical traction detachments. Ringlike apices along the arcades and disk create ringlike traction detachments. A broad area of adherence of the contracted PVC to the retina causes “tabletop” traction detachments. The continuity of the PVC between each apex must always be kept in mind. If the retina can be seen in some areas but not others, the shape of the retina in the visible areas can be used to extrapolate the contour as well as attached or detached configuration of adjacent nonvisible retina.
VITREOUS CLARITY
Some assessment of the age of a vitreous hemorrhage should be made. Discrete blood clots must go through thrombolysis and dispersion phases before clearing can occur. Subposterior vitreous detachment (sub-PVD) and preretinal hemorrhage clear much more rapidly than hemorrhage within the vitreous and should be described and managed accordingly. The retina can frequently be seen through semiopaque vitreous. It is useful to grade vitreous hemorrhage from 1+ to 4+ or clear, semiopaque, and opaque, to permit subsequent examiners to assess the rate of clearing. Fresh blood is bright red; the color of older hemorrhages becomes less saturated red and finally becomes yellow or gray.
RETINAL CONFIGURATION
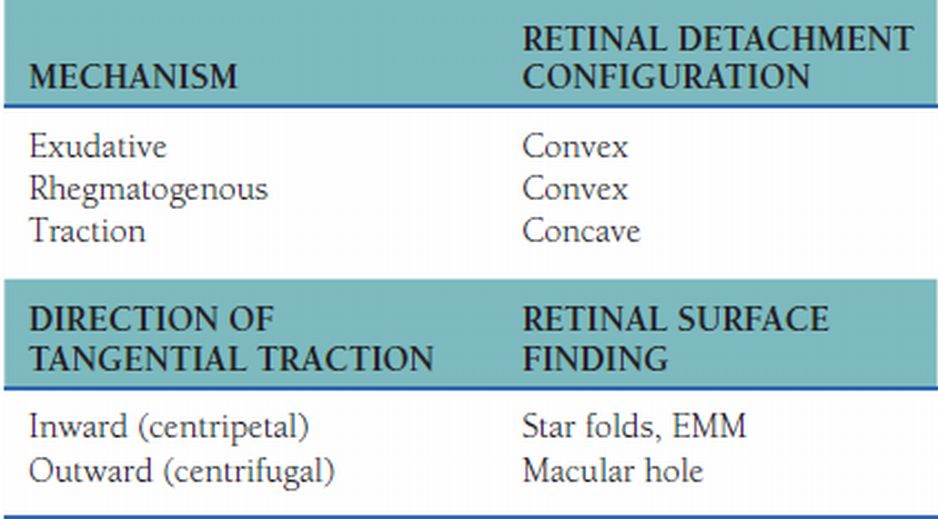
The transition from retinal to vitreoretinal surgery necessitates a change in examination goals. A compulsive, ritualistic quest for retinal breaks must be replaced in large part by an approach that emphasizes understanding of the forces acting on the retina. Retinal breaks eliminate the 0.8 mm Hg pressure gradient normally existing across the retina, resulting in a convex contoured rhegmatogenous retinal detachment. Damage to the retinal pigment epithelium (RPE) pump mechanism or increased vascular permeability also results in loss of the transretinal pressure gradient, which produces a convex configuration of the retina termed exudative retinal detachment. In contrast, the transretinal pressure gradient causes the concave shape of the retinal surface in TRD cases. A concave configuration with the presence of one or more retinal breaks means the normal transretinal pressure gradient is still present and proves the presence of traction. In contrast, convex retinal detachment with no visible retinal break must have a rhegmatogenous or exudative component.
Perpendicular or oblique traction on the retina is best recognized by alterations in retinal contour. Steep changes in retinal contour result only from PVC adherence and traction at the apex of the elevated retina. Broader zones of PVC adherence create truncated cones (mesa-like) of retinal elevation. Ridge-like changes in the retinal surface result from perpendicular (vitreous sheet) or ERM traction. Star folds and EMMs result from traction directed inward. Macular holes result from forces due to ILM elasticity, fenestrated ERMs, and/or residual vitreous and are directed outward. Retinal incarceration in a trauma or drainage site results in retinal foreshortening and must be relieved by retinal resection so that the retina can conform to the RPE.
RETINAL BREAKS
The detection of retinal breaks assists in surgical planning but can be more difficult in the patient with decreased vitreous clarity. In contrast to scleral buckling surgery, the view is always far better in the operating room than in the office. The reward for prolonged office examination of the patient can be examiner fatigue and patient discomfort.
Retinal breaks are frequently located adjacent to abrupt changes in retinal contour associated with vitreous traction. If the retina is concave, it is certain that these breaks have played a minor role in the retinal detachment. As any break may contribute to postvitrectomy detachments, all breaks must be recognized at the time of vitrectomy and treated. Retinal breaks are frequently located adjacent to retinal-RPE adherence areas or previous retinopexy sites acted on by vitreous traction. A drawing and description of the position of all retinal breaks should be made preoperatively and reviewed moments before or during surgery to avoid overlooking areas needing retinopexy. Too much emphasis is placed on the poor prognosis of so-called “combined” traction and rhegmatogenous retinal detachments associated with diabetic retinopathy.
RETINAL NEOVASCULARIZATION
Active neovascularization of the disk (NVD) or neovascularization “elsewhere” (NVE) can be thought of as a marker for the presence of VEGF in the vitreous cavity. Assessment of neovascularization is important not because of intraoperative bleeding, which is usually easy to control, but because it correlates with postoperative NVG and fibrovascular proliferation on the AVC and is an absolute indication for initial or supplemental PRP and anti-VEGF therapy. Large vessels in an ERM without active capillary budding remain present even after PRP and anti-VEGF agents markedly decrease VEGF levels. These larger vessels are more impressive but are not as significant as capillary activity.
EPIRETINAL MEMBRANE
Since “fibrosis” in the vitreous cavity is only present in the context of severe trauma or inflammation, this term should rarely be used. It should be recognized that an ERM is usually contiguous with the PVC in areas not having a posterior vitreous separation in the context of diabetic TRD. ERMs should be examined for color: a brownish pigment may indicate RPE etiology, while white coloration points more toward a glial mechanism although RPE cells dedifferentiate and lose pigment over time. It is essential to assess the relationship of the ERM to any retinal elevation. Broad areas of ERM, when contracted, cause larger areas of retinal elevation than do very small epicenters of ERM.
The ERMs in PVR are typically less opaque than the membranes associated with diabetic TRD or ROP. For this reason, they are frequently overlooked, and such misnomers as “retinal stiffening” are applied. Retinal stiffening in most disease processes is from periretinal membrane proliferation, even if the ERMs or subretinal membranes are transparent and difficult to see. Every fixed fold or star fold must have an ERM, subretinal membrane, or incarceration as its cause unless the problem is developmental. The surgical approach can only be planned by determination of the location of these membranes. The exact indications for removal are discussed in the chapters on appropriate disease states.
FOREIGN BODY LOCALIZATION
Localization of an intraocular foreign body (IOFB) has become somewhat of an end unto itself in the workup of trauma cases. Vitreous surgery has radically changed the approach to IOFB patients. For this reason, there is little need for extensive localization studies in most instances. If the fundus cannot be seen, in most cases, vitrectomy will be performed and accurate visualization of the foreign body will become possible intraoperatively. The relative inaccuracy of preoperative localization of foreign bodies near the ocular wall can contribute to mismanagement.
The nature of the injury causing the foreign body assists in localization. Most steel foreign bodies are created by hammering and seldom have the velocity to double penetrate the globe. For this reason, they may be assumed in most cases to be intraocular and managed with vitrectomy and forceps removal. In contrast, most shotgun injuries are double perforating because of the high velocity, and even if a lead pellet is intraocular, it need not be removed for 10 to 14 days. Computerized axial tomography is expensive and only moderately accurate, while magnetic resonance imaging (MRI) is contraindicated because a ferrous foreign body will be moved by the magnetic field. Foreign body localization techniques not utilizing a contact lens are extremely inaccurate and can give false information. Foreign body localization methods using a contact lens have the risks of infection and prolapse of ocular contents from the pressure of application of the contact lens. Ultrasonic methods, although better, are difficult to interpret when the foreign body is near the ocular wall. This will be discussed further in the section on diagnostic ultrasound. Anteroposterior and lateral x-rays of the orbit are important, however, to determine the presence and number of IOFBs but are not as useful in localization.
DIAGNOSTIC ULTRASOUND
Diagnostic ultrasound has greatly improved the management of the opaque media patient. This method, however, is best utilized in the hands of the potential surgeon rather than in a diagnostic laboratory setting. The surgeon has the entire clinical picture in mind at the time of ultrasonic examination, making possible better integration of the ultrasonic diagnosis into the thought process. If the ultrasound equipment is located in the surgeon’s primary examining room, it will be utilized much more frequently and can be done without charge if needed. Technicians should not be used for what should be thought of as acoustic ophthalmoscopy.
Clinical Acoustic Physics
An understanding of the physical principles involved in the interaction between ultrasonic energy and biologic materials is essential for accurate ultrasonic diagnoses. Ophthalmic ultrasonography utilizes pulse-echo reflection ultrasound. Brief pulses of ultrasonic energy having a 10-MHz, or greater, center frequency are repeated at a rate of 1 to 5 kHz, allowing time for the same transducer to receive the reflected echoes. Knowledge of the average speed of ultrasonic energy propagation through tissue (~1,540 m/s) permits the real-time calculation and display of the distance between the transducer and the echo-producing structure as a dimension on the two-dimensional (2D) display. Acoustic energy is reflected and refracted at interfaces between materials of different acoustic densities (Fig. 1.1).
Figure 1.1  Materials of different acoustic densities reflect and refract acoustic energy at their interfaces.
Materials of different acoustic densities reflect and refract acoustic energy at their interfaces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


