3 Preoperative and Postoperative Diagnosis
The old wisdom that a surgeon’s excellence is based more on his skill in diagnosing and indicating than on his manual dexterity is particularly valid for endoscopic sinus surgery. Since chronic sinusitis with all its variations is one of the most frequent diseases in normal populations, its surgical treatment cannot be planned for every case but must be selected appropriately for the candidate. The following paragraphs will summarize the related algorithm for this task.
Endoscopic surgery of the paranasal sinuses is also indicated for the treatment of tumors or trauma and the removal of foreign bodies, but essentially for chronic sinusitis and recurrent acute infection of the sinuses and its complications. A diagnosis of chronic hyperplastic sinusitis is not always an automatic indication for surgery, since not all these lesions need surgical treatment. Only a small proportion of patients with inflammatory mucosal lesions present to the otorhinolaryngologist. If a symptom-free sinusitis is discovered coincidently, careful assessment is required to determine whether surgery is advisable, because it carries risks and complications that may make the patient worse. On the other hand, symptom-free chronic sinusitis contributes more often than is commonly thought to the genesis of a wide range of serious diseases, including lesions of the orbit and the optic nerve, otitis media, laryngotracheobronchitis, and inflammation of the heart, the joints, the urinary tract, and the skin.
History Taking
The typical symptoms of sinusitis (Table 3.1) include anterior nasal discharge, postnasal drip, catarrh, and nasal obstruction. The cause and effect often overlap: septal deviation may cause nasal obstruction, which is made worse by the resulting hypertrophy of the turbinates and thickening of the mucosa due to sinusitis. Pain, a feeling of pressure, and loss of the sense of smell are not universal symptoms and are more common in acute than in chronic sinusitis. Questioning should be systematic and encompass the most important symptoms, and should also cover the symptoms of ear disease (variable hearing loss, crackling and itching in the ears, feeling of pressure, etc.), pulmonary symptoms (coughing, spitting, wheezing, etc.), diseases of the teeth and jaws, allergic symptoms, inflammatory disease of the joints, the urogenital system,the orbital apparatus, and the skin, and autonomic disorders, dizziness, and fatigue. You should not forget to ask about ear symptoms like hearing loss, low-tone tinnitus, or pressure sensation. Chronic throat symptoms such as pain and dryness in the throat, hawking, globus and hoarseness are often due to discharge from a chronic sinusitis flowing down the pharynx. Thus, the ear, nose, and throat area should always be examined carefully.
| Nasal obstruction | 64% |
| Facial pain, pressure, or headache | 51% |
| Troublesome nasal discharge | 44% |
| Discomfort in the throat and hawking | 9% |
| Bronchitis and cough | 9% |
| Globus | 9% |
| Disorders of smell | 7% |
| Eustachian tube dysfunction | 7% |
| Hay fever | 5% |
| Bronchial asthma | 5% |
A record of the symptoms should be kept and the patient’s quality of life should also be assessed using a scoring system. Examples are given in the literature (Kennedy 1992; Lund and Mackay 1993; Lund 2001; Birch 2001). The author’s presentation of results (see Chapter 12) includes some of these most important parameters. A preoperative interview will, naturally, concern the patient’s own history of related diseases such as ASA intolerance, mucoviscidosis, or nasal trauma, but one should also ask about rhinological syndromes in the family.
Rhinoscopy and Nasal Endoscopy
Inspection of the nose by anterior and posterior rhinoscopy, preferably with a 30° angled telescope, may show a stream of pus running from the semilunar hiatus over the inferior turbinate (Fig. 3.1), tenacious plugs of mucus lying in the ostium of the antrum, or polyps. These cases are almost always associated with a polypoid ethmoiditis if small granulations or large polyps are found protruding from under the middle turbinate or lying in the superior meatus in the region of the posterior ethmoids (Fig. 3.2). Isolated nasal polyposis without sinusitis is exceptional, although edematous swellings of the end of the turbinate can occur. The pedicle of a choanal polyp often arises in the antral cavity, but can originate from the posterior ethmoid or the middle turbinate. Nasal mucosa that appears normal does not exclude chronic sinusitis: conversely, it is not possible to deduce anything about the sinus mucosa from the swelling or color of the nasal mucosa. Nevertheless, reddening, lichenification, or eczema of the nasal vestibule and the external skin at the nasal introitus strengthen suspicions arising from the history. Nasal endoscopy in children is inevitably handicapped. The use of flexible rhinoscopes is helpful to detect gross abnormalities and to check the nasopharynx. While straight or lowangled optics are sufficient for the initial rhinoscopies, the use of wide-angled rigid endoscopes (70°–90°) becomes indispensable after surgery if the frontal sinus infundibulum and the maxillary sinus have to be inspected. Flexible endoscopes are only useful within the borders of their limited sharpness.
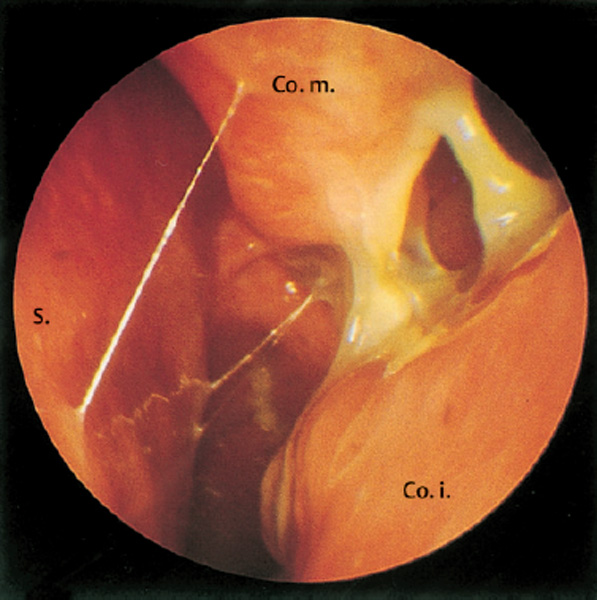
Fig. 3.1 Pus in the left middle meatus between the inferior and middle turbinate (30° telescope).
Endoscopy is useful for taking swabs from distant areas for bacteriological and mycological examination. This investigation makes sense for conservative treatment of chronic rhinosinusitis, but is more rational in surgical candidates after the intervention. Special testing of nasal mucus for the diagnosis of eosinophilic fungal rhinosinusitis (Ponikau et al. 2002) is still a matter of controversy.
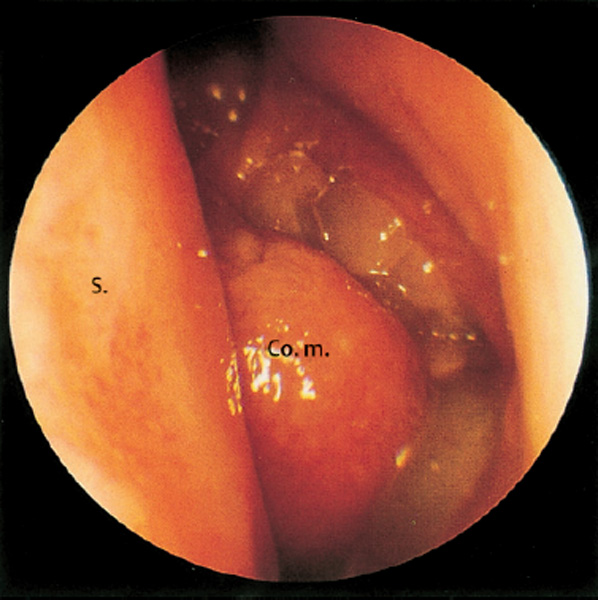
Fig. 3.2 Polyp in the left middle meatus. Only the head of the middle turbinate can be seen (straight telescope).
Ultrasound
In comparison with the precise imaging of pathological abnormalities by computed tomography and magnetic resonance imaging, ultrasound scanning is of little value. Its signals are blurred and can only trace changes within large hollow cavities, thus excluding bone and the ethmoid cells from diagnosis. Also, the sphenoid cavity lies beyond a practicable distance. However, if one confi nes the application of ultrasound to simple questions, such as presence of air or fluid, size, growth, or persistence of a lesion despite treatment, it has certain advantages: the avoidance of radiation, low economic investment, and ease of accommodation in a normal office. For these reasons, many rhinologists use ultrasound in particular for initial screening and for repetitive follow-up examinations. Technical details and critical evaluation can be drawn from specialized monographs (Iro et al. 2000).
Ultrasound A Scan
A normal echogram (Fig. 3.3) contains an initial complex of spikes corresponding to 20–30 mm distance representing the anterior wall of the sinus with overlying skin and subdermal tissue. If there are echoes beyond these layers, one can expect pathological contents. Figure 3.4 a–c shows examples of a mucosinus and a cyst. While ultrasound waves are poorly transmitted through air, their propagation through fluid is enhanced. A fl uid-fi lled cavity thus allows the appearance of a reflected spike from the dorsal wall. Polyposis may produce two or three separate echoes of decreasing intensity (decrescendo).
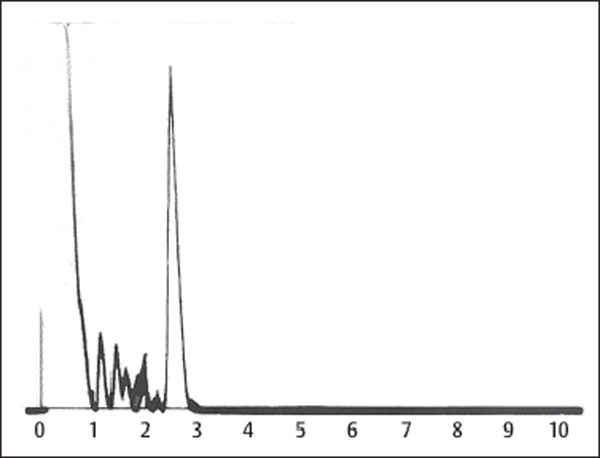
Fig. 3.3 Normal ultrasound A echogram.
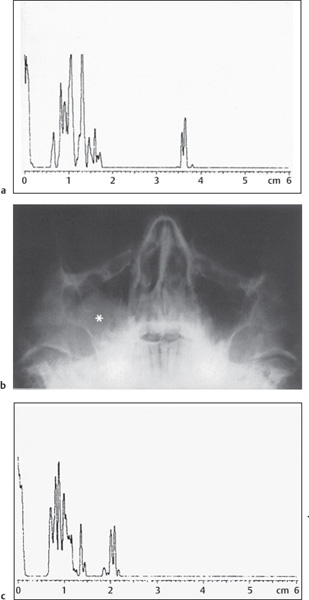
Fig. 3.4 a–c Pathological ultrasound A echograms.
a. A second echo at a distance of 3.5 cm represents the dorsal wall of the maxillary cavity, thus giving evidence of a fluid-filled sinus.
b. Radiograph of a large cyst (“) in the right maxillary cavity.
c. The related A-scan shows a second echo at a distance of 1 cm behind the first group of spikes, representing the anterior wall echo.
Ultrasound B Scan
According to the physics of ultrasound, due to the change of impedance between soft tissue and bone–as between bone and air–a total reflection of the waves occurs behind the anterior wall of the maxillary cavity. Therefore, only the echo of its anterior wall is produced. The thickness of the soft-tissue layer amounts to 0.8–1.0 cm at the maxillary cavity and to 0.5 cm at the frontal sinus. When the cavities are filled with fl uid or thickened mucosa, or when polyps lie in direct contact with the anterior wall, the waves continue into the depth and may be refl ected at the dorsal wall.
A cyst or a tumor can thus be imaged (Fig. 3.5). Single internal echoes may occur. Multiple reflections indicate a solid space-occupying lesion with uneven surface. However, when there is an air-filled space, and it may be very thin, between the anterior wall and the pathological contents, a “dorsal echo” is suppressed.
Defects of the anterior wall due to osteitis or malignancy are represented by gaps within the end of spikes of the anterior wall complex.
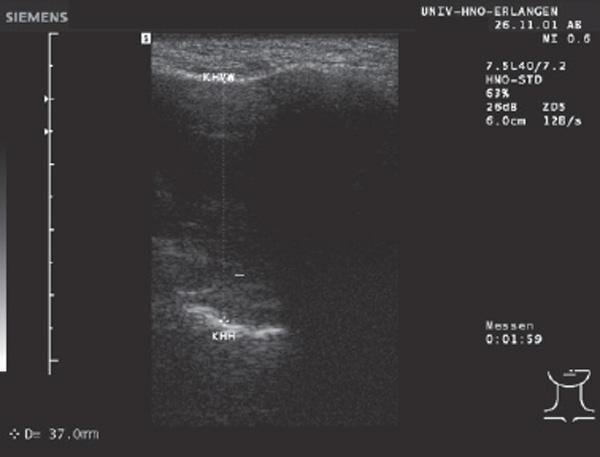
Fig. 3.5 Ultrasound B echogram. The picture must be read from above downward. The sector transducer has produced a broad horizontal echo band representing the anterior wall of the maxillary sinus. The appearance of a second echo band inferiorly at a distance of about 6.0 cm proves the displacement of air by fluid and/or mucosal hyperplasia, here in a case of chronic sinusitis.
Radiography, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI)
H. Greess
Diagnostic imaging of the paranasal sinus even today starts out with conventional radiographic examinations. These are well suited as a fundamental diagnostic tool and, if normal, may avoid further costly examinations. They facilitate basic orientation, may demonstrate fractures of the viscerocranium, and may answer fundamental questions concerning pneumatization of the paranasal sinuses (e. g., frontal sinuses following surgery; air–fl uid levels or cysts in the maxillary sinuses) without further expense. Low cost, low radiation exposure (most important in children and pregnant women), and wide availability represent additional advantages. Abnormal findings on conventional imaging or persisting symptoms despite unremarkable radiographs should be clarifi ed using CT or, in special cases, MRI.
Conventional Radiography
The standard conventional examination of the paranasal sinuses is the occipitomental (OM) projection. This shows the frontal and maxillary sinuses as well as the sphenoid sinus, the latter being projected inside the open mouth, the former being magnified due to the chosen projection. Imaging of the paranasal sinuses without magnifi cation of the frontal sinuses can be achieved using occipitofrontal (OF) focusing. This projection is most commonly used before percutaneous surgery of the frontal sinuses. The ethmoidal sinuses are evaluable only to a very limited extent because the radiation projects many cells over each other. An additional lateral projection can be helpful todifferentiate between hyperplastic shallow frontal sinuses and increased density caused by fluid retention in acute sinusitis. Further indications for the use of lateralprojections are fractures close to or involving the frontalsinuses, especially if the dorsal osseous boundaries are affected.
The ENT practitioner can easily read from a plane OM view that the patient’s complaints stem from an acute sinusitis when the projection shows only horizontal or concave air–fluid levels (Fig. 3.6a, b) . Convex spherical opacity and broad marginal shadows, in contrast, indicate chronic hyperplastic sinusitis featuring cysts or polyps (Fig. 3.7a, b) . A translucent picture of the frontal and maxillary cavity, however, does not excluded pathological alterations in the ethmoids (Fig. 3.8a, b).
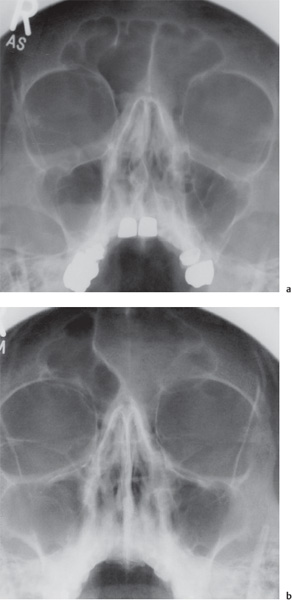
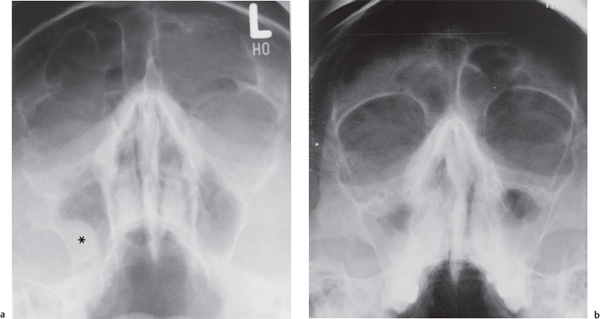
Fig. 3.7a Convex semi-lunar shadow in the right maxillary sinus (*) with marginal opacification of both antral cavities together with shadows in the left frontal sinus indicating chronic hyperplastic mucositis. The probable primary focus in the ethmoids is not verified by this imaging. b Thick marginal shadows in both maxillary sinuses and cloudy opacification in the frontal sinuses allow the diagnosis of chronic sinusitis from this plain radiograph.
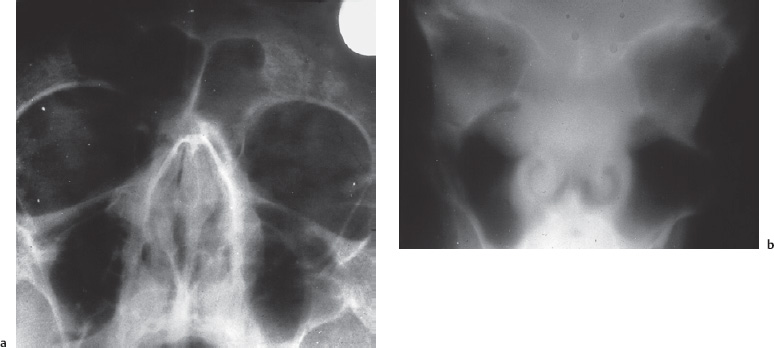
Fig. 3.8 a, b Occult ethmoiditis demonstrated by radiology.
a. Apparently normal occipitomental view.
b. Massive opacity of the ethmoid and ethmoid recess of the antrum shown by polytomography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


