Endoscopic, expanded endonasal approaches (EEAs) were developed through the collaboration between skull base surgeons (otolaryngologists and neurosurgeons) and neuroradiologists. Full endonasal access to the skull base required a visualization tool (eg, the endoscope) and specialized instrumentation to work through the nostrils. Once these endoscopic technologies were applied, an understanding of sinus anatomy and its relationship to the skull base became the key to the EEA. This bridge between otolaryngologists and neurosurgeons was built through collaboration with skull base radiologists. The radiographic evaluation of skull base anatomy and its relationship with associated tumors remains critical for preoperative planning and intraoperative guidance.
Endoscopic, expanded endonasal approaches (EEAs) are being used with increasing frequency for accessing the sella, parasellar region, anterior cranial base, clivus, upper cervical spine, and petrous region . These approaches were developed as a result of collaboration between skull base surgeons (otolaryngologists and neurosurgeons) and neuroradiologists. Anatomically, these anterior approaches, using a binarial approach to the sinuses for access, often have a conceptual advantage when compared with posterior or lateral approaches that may require transgression or retraction of important neurovascular structures. Full endonasal access to the skull base, however, requires a visualization tool such as the endoscope as well as the development of specialized instrumentation to work through the nostrils. In addition, these approaches could be applied safely only with the aid of intraoperative image guidance. Once these endoscopic technologies were applied, an understanding of sinus anatomy and its relationship to the skull base became the key to the EEA. This bridge between otolaryngologists and neurosurgeons was built through collaboration with skull base radiologists. The radiographic evaluation of skull base anatomy and its relationship with associated tumors remains critical for both preoperative planning and intraoperative guidance.
Anatomic relationships and pathology
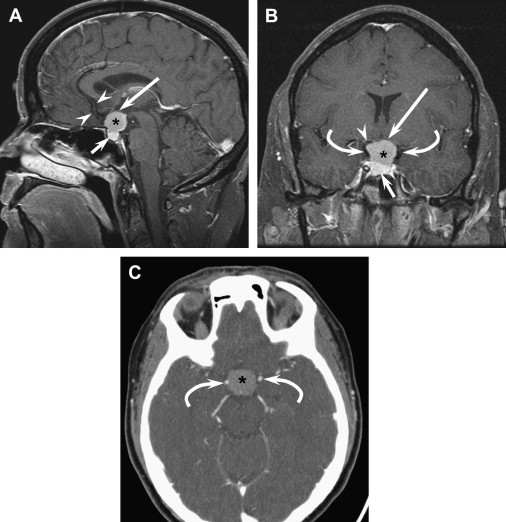
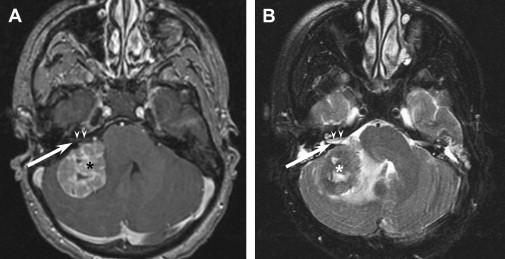
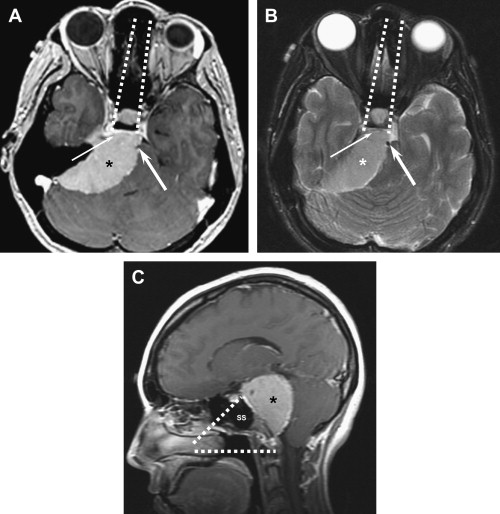
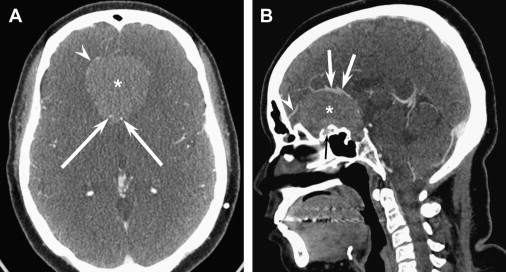
Virtually any anterior cranial base, clival, or anterior craniocervical pathology can be addressed by an EEA. The key conceptual advantage for these anterior approaches is that most of the lesions that occur in these locations originate medial and anterior to the multitude of neurovascular structures entering and exiting the cranial base. In addition to generating a differential diagnosis, the most critical function of imaging is to evaluate these relationships. For example, meningiomas are a common skull base pathology with multiple potential sites of origin. Tumors that originate from the tuberculum sellae or planum sphenoidale displace the optic nerves superiorly and laterally, the optic chiasm superiorly and posteriorly, the internal carotid arteries (ICAs) laterally, the anterior cerebral and communicating arteries superiorly, and the pituitary gland inferiorly ( Fig. 1 ). Frequently, the only structure between the sphenoid sinus and tumor is bone. In contrast to tuberculum meningiomas, cerebellopontine angle meningiomas often originate posterior to the involved cranial nerves (V through X) and basilar arterial arteries, thereby displacing them anteriorly ( Fig. 2 ). This location makes these tumors poorly suited for an anterior approach but ideally suited for a posterior approach, such as a retromastoid craniotomy. Finally, petroclival meningiomas originate around the petroclival junction, which can make the cranial nerve involvement and displacement very variable. Determination of the course of involved nerves and arteries (vertebral, basilar, and carotid) is necessary to know if these tumors can be addressed by an endonasal approach ( Fig. 3 ). A combination of MRI and CT angiography is usually best to evaluate these relationships fully. Fine-cut, axial T2-weighted MR imaging (fast-spin echo sequences) usually demonstrates the relationship of the tumor to neural tissue very well. CT angiograms, however, best reveal bony involvement and access as well as vascular relationships. Often, CT and MRI are used in combination during preoperative planning.
There are different concerns and considerations for an EEA depending on the location and pathology of skull base lesions. Obviously, the sinus anatomy through which access is gained varies depending on the location. In addition, the neurovascular constraints on an EEA are different in each location, from the crista galli to the dens and from infratemporal and middle fossa to midorbit. The degree of involvement with these structures and the surgical aggressiveness are dictated by pathology.
Transcribriform lesions
The ethmoid sinuses border the cribriform plate and, with the use of the endoscope, provide a natural corridor for approaching tumors in this region. One such tumor is esthesioneuroblastoma (a sometimes slow-growing, malignant tumor that originates from basal progenitor cells of the olfactory epithelium), which usually involves the anterior skull base both macro- and microscopically and is treated traditionally with an open, anterior craniofacial resection for removal of all involved and potentially microscopically involved structures, including the middle turbinate, olfactory bulb, and subfrontal dura mater through a bifrontal craniotomy. EEA provides an identical resection, lacking only the en bloc removal that is the goal of open surgery. Early results from the authors’ group and others suggest equivalence . These resections require a thorough understanding of the radiographically involved areas and careful histopathologic assessment of all margins to ensure an adequate and equivalent resection. To this end, intraoperative image guidance is critical in the learning phase for endoscopic surgeons. There is, however, no substitute for negative margins.
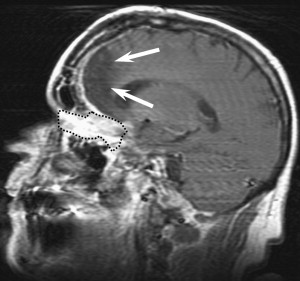
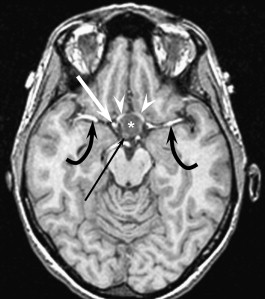
For comparison, olfactory groove meningiomas are extra-axial, intradural tumors that also abut the ethmoidal and frontal sinuses. EEA for resection of these tumors is as controversial among neurosurgeons as EEA for esthesioneuroblastoma is among otolaryngologists. Nevertheless, the authors’ group has had excellent results with endonasal resection of these tumors and is optimistic that the lack of brain manipulation associated with this approach will limit the longstanding and frequently devastating encephalomalacia associated with open, subfrontal approaches ( Fig. 4 ). As with an open approach to these tumors, it is critical to understand both the neurovascular structures involved (especially the anterior cerebral arteries and their branches) ( Fig. 5 ) and the presence of subpial invasion, suggested by increased signal change on flair MRI sequences ( Fig. 6 ). Subpial invasion increases the difficulty of resection, given the lack of a arachnoid plane between brain and tumor, and, as a result, increases the risk to involved neurovascular structures.

Planum/tuberculum/sellar lesions
The tuberculum sphenoidale, planum sphenoidale, and sella turcica are areas commonly involved in skull base surgery. Tumors ranging from meningiomas to craniopharyngiomas to giant pituitary adenomas to epidermoid cysts frequent this region. Pterional or subfrontal approaches are limited by the optic chiasm, because this structure intervenes between the surgeon and pathology when approached from above. This position has generated much discussion regarding the importance and surgical implications of a prefixed (overlying the tuberculum sellae) versus a postfixed (overlying the dorsum sellae) chiasm. Although it important to recognize this relationship when approaching these lesions endonasally, it is rarely as significant as the relationship to the pituitary stalk.
For example, some tumors originate directly from or invade into the pituitary infundibulum. Craniopharyngiomas are lesions that commonly have a suprasellar extension. As mentioned, when the lesion is approached by a craniotomy, it is critical to understand the position of the optic chiasm, because the window for tumor resection depends on that position. When the lesion is approached by an EEA, the position of the pituitary stalk and its involvement with the tumor is at least as important. The authors have designated three types of craniopharyngioma, based on this relationship. A type I tumor grows anterior to the infundibulum and has a plane between it and the infundibulum ( Fig. 7 ); a type II tumor grows within the stalk ( Fig. 8 ); and a type III tumor is posterior to and often is surgically separable from the infundibulum ( Fig. 9 ). This last type may grow superiorly into the anterior third ventricle or posteriorly into the interpeduncular cistern. The relationship to the stalk is important, because it has implications for the ability to preserve the pituitary stalk (and therefore gland function) and determines the particular endonasal approach used to access the tumor. This relationship is equally important for other, rarer lesions such as granular cell tumors and suprasellar epidermoids.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


