Introduction
To determine the feasibility of preloading endothelial tissues for Descemet membrane endothelial keratoplasty (DMEK).
Design
Laboratory investigation.
Methods
setting : Institutional. participants : Twenty human donor corneas unsuitable for transplantation with endothelial cell density in a range of 1600–2700 cells/mm 2 . Intervention : The endothelium was punched, stripped (8.5 mm diameter) and manually tri-folded with the endothelial side inward. The excised membranes were gently moved in a 2.2 intraocular lens (IOL) cartridge and pulled further in the funnel using 25 G end-grasping forceps. The cartridge was filled with transport media (TM) (sealed at its funnel and back entrance with a stopper) and the tissue was preserved for 4 days at room temperature in the bottles containing TM. main outcome measures : Success rate of preparation, processing time, endothelial cell loss (ECL), and active metabolism.
Results
The tissues were peeled and loaded successfully in all cases. Average stripping and loading time was 20 and 4.5 minutes, respectively. ECL after preservation was 4.35% with 3.55% (± 5.89%) mortality and 7.80% (± 14.12%) uncovered areas. A total of 0.55 (± 0.26) mg/mL of glucose was consumed by the cells showing active metabolism.
Conclusions
Tri-folded (endothelium-in) DMEK grafts can be preloaded using TM in an IOL cartridge and stored up to 4 days with limited endothelial damage. Direct injection of TM should be avoided because of the presence of bovine serum, but the tissue can be washed using balanced salt solution and gently injected. Alternatively, the graft can be easily delivered using a bimanual pull-through technique. Preloading DMEK grafts will simplify the surgery with reproducibility, reduced surgical time, and reduced tissue wastage, cost, and logistical requirements.
Endothelial keratoplasty (EK) is a selective transplantation technique and an effective alternative to penetrating keratoplasty (PK) for the management of corneal endothelial failure. Descemet membrane endothelial keratoplasty (DMEK) is a subtype of EK that foresees the transplantation of Descemet membrane and endothelium exclusively and offers an extremely fast recovery of vision, often at the 20/20 level.
Similar to other lamellar keratoplasty procedures, DMEK is gaining popularity and eye banks are confronted with new requirements from corneal surgeons. Recently, the eye banks have started the preparation and transportation of precut donor tissues with a desired diameter for Descemet stripping automated endothelial keratoplasty (DSAEK), ultra-thin DSAEK (UT-DSAEK), and prestripped tissues for DMEK.
As this reduces the efforts, time, and cost in the surgical theater, the popularity of precut/prestripped tissues is increasing rapidly. Moreover, it allows validation of the tissue to be grafted and quality control that cannot be done in the surgical theater, when the surgeons prepare the tissue themselves. The Veneto Eye Bank Foundation has now started providing preloaded tissues, a step beyond precut tissues for DSAEK and UT-DSAEK surgeries. This further reduces the time and efforts in the surgical theater, increases the efficiency of DSAEK surgery, and allows the use of a validated tissue. DMEK tissues can be prestripped or prebubbled at the eye bank and shipped to the operating room with the full cornea as a base support. Instead, if the DMEK tissue is stored without corneal support, it rolls with the endothelium facing outward, in contact with the solid walls of the cartridge, thus possibly being negatively affected by the storage process. We have investigated the possibility of preserving DMEK tissue rolled with the endothelium inward to avoid any damage caused by the contact with the cartridge wall and providing a ready-to-use tissue to the surgeons for direct transplantation. This paper is a proof of concept for a preloaded DMEK and the clinical relevance still needs to be tested.
Methods
Ethical Statement
Twenty human donor corneal tissues were collected from The Veneto Eye Bank Foundation, Venice, Italy, to be used for research, with a written consent from the donor’s next of kin.
Donor Characteristics
The average age of the donors was 67.6 (± 7.47) years with a male-to-female donor ratio of 14:6. The average postmortem time of 15.99 (± 5.56) hours and preservation time of 14.5 (± 4.83) days in tissue culture medium (TCM) were recorded, followed by 4.6 (± 6.27) days in transport medium (TM). TCM was composed of 2% newborn calf serum with MEM-Earle as a base medium along with 25 mM Hepes buffer, 26 mM sodium bicarbonate, 1 mM pyruvate, 2 mM glutamine, 250 ng/mL amphotericin B, 100 IU/mL penicillin G, and 100 mg/mL streptomycin. TM was composed of TCM + 6% dextran T500. TCM and TM were prepared in house (FBOV, Mestre, Italy) with full regulatory compliance. The endothelial cells were determined using a hypotonic sucrose solution and the mortality was estimated using trypan blue staining. The endothelial cells were checked using an inverted microscope (Zeiss, Jena, Germany). The average endothelial cell density recorded was 2070 (± 374.31) cells/mm 2 with no initial mortality or uncovered areas.
Stripping Method
The corneas (n = 20) were centered on a punch base of the suction. Vacuum was created using a syringe and the cornea was secured on the base. A 9.5 mm trephine (Moria, Antony, France) was used to make a superficial cut using a gentle tapping method. The endothelium was stained with trypan blue for about 20 seconds to determine the area of the cut. Excess peripheral membrane was removed using 120 mm acute forceps (e.janach, Como, Italy). The endothelium was kept moist during the entire procedure using TM to create a film of fluid on the top of the corneoscleral ring. The membrane was slightly lifted using a cleavage hook and the procedure was carried on along the entire circumference of the cut to ensure limited tearing of the very fragile DMEK tissue. The peripheral membrane was stripped with a longitudinal movement using a 3-quadrant method, ensuring no torsions were generated during this phase to limit the mortality. Once the tissue was stripped completely, it was re-stored on the corneal stroma.
Loading Method
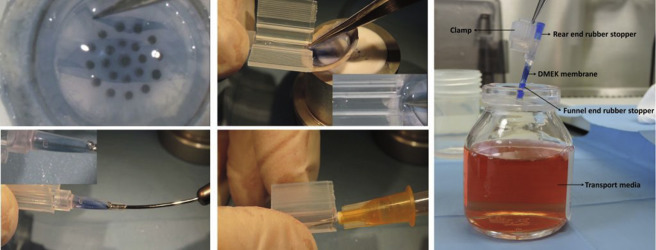
The prestripped membrane (9.5 mm) was trephined again with an 8.5 mm punch (Moria) and the excess periphery was removed, maintaining the endothelial side facing the air. The membrane was folded manually from 2 ends using an acute forceps, touching the Descemet side to avoid as much endothelial damage as possible ( Figure 1 , Top left; Supplementary Video 1 , available at AJO.com ). A small drop of liquid was added on the membrane to keep the tissue moist during the entire procedure. The purpose of the drop was only to support the moisture and not the opening of the membrane, as this may change the orientation. The membrane was gently moved from the tissue base to a 2.2 intraocular lens (IOL) cartridge (Viscoject, Wolfhalden, Switzerland) preservation chamber ( Figure 1 , Top middle). This step can be performed either using a contact lens as a scaffold, as shown by Busin and associates, or directly from the cornea to the cartridge, maintaining the architecture of the membrane. The membrane was pulled inside the funnel using a Grieshaber Revolution DSP 25 Ga+ end-grasping forceps (Alcon, Ft Worth, Texas, USA) from the funnel opening ( Figure 1 , Bottom left). A small amount of TM (<0.5 mL) was used to fill the funnel of the IOL cartridge for preservation of the DMEK membrane from its rear end ( Figure 1 , Bottom middle). The IOL cartridge was sealed with a rubber plug at both the funnel and the rear exit ( Supplementary Video 2 , available at AJO.com ). The entire unit was sealed with an in-house modified plastic clamp. The entire system was preserved in a sterile vial with TM for 4 days at room temperature ( Figure 1 , Right). The plug was removed and the tissues were released out from the funnel pore using the end-grasping forceps and analyzed post preservation.
Endothelial Cell Survival
The membranes were stained with trypan blue for 20 seconds and washed with phosphate-buffered saline. The endothelium was checked using an inverted microscope (Primovert; Zeiss, Jena, Germany) for endothelial cell survival and tissue integrity. The cells were counted using a 10 × 10 eyepiece reticule and the images were captured at 100× magnification.
Glucose Uptake
Glucose uptake was determined in the preservation media in which the tissues were preserved for 4 days. The metabolic activity of the endothelial cells was checked using this technique. A D-Glucose HK kit (Megazyme International Ireland Ltd, Bray Business Park, Bray, Ireland) was used for quantitative analysis post preservation.
Results
Endothelial Cells Survive After Preserving Preloaded Descemet Membrane Endothelial Keratoplasty Grafts
All 20 final experimental tissues were stripped and loaded successfully (100% cases). Average stripping and loading time was recorded at 20 and 4.5 minutes, respectively. Average endothelial cell density after stripping the tissues was 2070 (± 374.31) cells/mm 2 , which did not differ from the initial count. However, the mortality increased to 5.08% (± 12.61%). There were visible uncovered areas in the tissues post stripping, with an average of 0.73% (± 1.89%) (calculated manually at a magnification of 100× using a 10 × 10 calibrated reticule mounted in the ocular of the microscope—fixed frame technique) ( Figure 2 , Left). Average endothelial cell density post preservation was found to be 1980 (± 278.34) cells/mm 2 with mortality of 3.55% (± 5.79%) and 7.8% (± 14.13%) uncovered areas (area on the tissue without endothelial cells) ( Figure 2 , Middle). Endothelial cell loss (ECL) after preservation was 4.35%. Localized uncovered areas were observed in some parts ( Figure 2 , Middle). Apart from the areas where the end-grasping forceps come in contact with the endothelium for pulling the graft inside the funnel (approximately 0.25–0.5 mm 2 ), other areas of the periphery did not show any cell loss or mortality ( Figure 2 , Right). It was also observed that if the tissues are kept moist and folded just to orient the graft, then minimal to no mortality can be observed.




