Purpose
To analyze the predictive factors associated with success of iris recognition and dynamic rotational eye tracking on a laser in situ keratomileusis (LASIK) platform with active assessment and correction of intraoperative cyclotorsion.
Design
Interventional case series.
Methods
Two hundred seventy-five eyes of 142 consecutive candidates underwent LASIK with attempted iris recognition and dynamic rotational tracking on the Technolas 217z100 platform (Techolas Perfect Vision, St Louis, Missouri, USA) at a tertiary care ophthalmic hospital. The main outcome measures were age, gender, flap creation method (femtosecond, microkeratome, epi-LASIK), success of static rotational tracking, ablation algorithm, pulses, and depth; preablation and intraablation rotational activity were analyzed and evaluated using regression models.
Results
Preablation static iris recognition was successful in 247 eyes, without difference in flap creation methods ( P = .6). Age (partial correlation, −0.16; P = .014), amount of pulses (partial correlation, 0.39; P = 1.6 × 10 −8 ), and gender ( P = .02) were significant predictive factors for the amount of intraoperative cyclodeviation. Tracking difficulties leading to linking the ablation with a new intraoperatively acquired iris image were more with femtosecond-assisted flaps ( P = 2.8 × 10 −7 ) and the amount of intraoperative cyclotorsion ( P = .02). However, the number of cases having nonresolvable failure of intraoperative rotational tracking was similar in the 3 flap creation methods ( P = .22).
Conclusions
Intraoperative cyclotorsional activity depends on the age, gender, and duration of ablation (pulses delivered). Femtosecond flaps do not seem to have a disadvantage over microkeratome flaps as far as iris recognition and success of intraoperative dynamic rotational tracking is concerned.
Misalignment between the eye and the ablation beam during laser in situ keratomileusis (LASIK) may result into suboptimal correction. Use of iris registration and online tracking during surgery has been shown to improve results after LASIK, especially for astigmatic errors. Online tracking was carried out only for horizontal and vertical (x-y) and depth (z) movements of the eye until recently. Some of these systems had an iris registration-driven static preablation cyclotorsion assessement. However, cyclotorsion is an active phenomenon having effects in fields as diverse as toric intraocular lens evaluation, effects on macular translocation surgery, and contact lens fitting.
Studies have confirmed substantial amounts of intraoperative cyclotorsion during excimer laser ablation. The benefits of incorporating a rotational tracking have been demonstrated by Arba-Mosquera and associates in a mathematical model and by Wang and Koch in a simulation model. Recently, Chang documented intraoperative cyclotorsion during treatment with dynamic rotational eye tracking. Neuhann and associates and Venter demonstrated good clinical outcomes with intraoperative cyclotorsion tracking on 2 different laser platforms. However, the factors predictive for the amount of intraoperative cyclotorsion and its successful performance have not been studied in detail. Furthermore, a previous noncomparative case series suggested that femtosecond flaps may lead to difficulty in online tracking. In this study, we considered the various preoperative and intraoperative factors associated with dynamic rotational eye tracking and analyzed the predictive nature of these variables in successful dynamic rotational tracking in cases undergoing femtosecond laser and microkeratome-assisted flap creation for LASIK or epi-LASIK.
Methods
In this prospective study, consecutive candidates undergoing LASIK with dynamic rotational eye tracking from October 2008 through March 2009 were evaluated. The preoperative evaluation included of history, uncorrected and best-corrected visual acuity, refraction, slit-lamp biomicroscopy, corneal topography, iris image capture and Hartmann Shack wavefront aberrometry, biometry, anterior segment optical coherence tomography, and dilated fundus evaluation.
Aberrometry, Corneal Analysis, and Iris Image Acquisition
These steps were performed on the Zyoptix diagnostic workstation (Bausch & Lomb, Inc., Rochester, New York, USA). The acquisitions, consisting of iris image capture and undilated and dilated aberrometry, were carried out on a Zywave II aberrometer (Bausch & Lomb, Inc.), which is a device based on the Hartmann Shack principle. The recent version of the Zywave workstation also has been described briefly by Neuhann and associates. Corneal analysis was carried out by the Orbscan IIz Anterior Segment analyzer (Bausch and Lomb, Inc.). The data was stored as an Orbscan Technolas Export file or an Aberrometer Technolas Export file, which was accessed using the Treatment Calculator Software (Bausch & Lomb, Inc.). On the basis of the data from these files, along with the desired flap thickness, the software calculated a Technolas Laser Session file for wavefront-based treatment and Standard Session file (Bausch & Lomb, Inc.) for nonwavefront-guided tissue-saving treatment. These files were then transferred to a network server (Trulink; Bausch & Lomb, Inc.) that performs central storage between the diagnostic workstation and the T217z100 laser.
The treatment methods used were either wavefront guided (Zyoptix Personalized) or nonwavefront guided (Zyoptix Tissue Saving), both using preablation iris recognition and dynamic rotational eye tracking. Although both methods use truncated Gaussian beams of 1- and 2-mm spot size, the tissue-saving mode ablates the lesser cornea because it does not attempt to correct the higher-order aberrations. The difference between the 2 methods of treatment becomes useful in cases with higher power and thinner corneas.
The wavefront-guided treatment used the Technolas Laser Session file. The ablation data for the tissue-saving mode either was loaded from the Standard Sessions file or was entered manually in the laser delivery software. The iris data for tissue-saving mode was loaded from the Iris Reference Data file or the Aberrometer Technolas export file.
The attempted flap thicknesses (and devices used) were 65 μm (Zyoptix XP epi-separator, for epi-LASIK), 90 to 120 μm (Intralase, Abott Medical Optics, Chicago, Illinois, USA, for femtosecond laser flaps), and 120 and 140 μm (Zyoptix XP, Bausch & Lomb, for microkeratome-assisted flaps). The choice of the procedure was determined by a target of residual bed thickness of more than 300 μm and the patient’s preference of femtosecond, microkeratome, or epi-LASIK procedures.
In all cases that underwent femtosecond laser-assisted flap creation, a 60-KHz femtosecond laser (Intralase, Irvine, California, USA) was used for flap creation. The default flap diameter was kept at 8.7 mm in all patients. However, to adjust the applanation cone, the flap diameter was reduced in certain cases. Therefore, the flap diameter varied from 8.7 to 8.5 mm. The rest of the parameters were: flap thickness, 120 μ, 110 μ, 100 μ, 90 μ; hinge, superior; hinge angle, 55 degrees; bed energy, 0.9 μJ; spot separation, 7 μ; line separation, 7 μ; side cut energy, 1.5 μJ; side cut angle, 70 degrees; pocket enable, on; pocket width, 0.250 mm; pocket start depth, 220 μ; pocket tangent and radian spot separation, both 5 μ.
The excimer ablation system used in all cases was the Technolas 217z100 (Techolas Perfect Vision, St Louis, Missouri, USA) with advanced control eye tracking with dynamic rotational eye tracking. This new laser platform (217z100) has a software Keracor V 4.21, which allows for an intraoperative dynamic rotational correction activity, in addition to static preablation rotational misalignment assessement. The dynamic rotational tracking and compensation occurs independent of x-y-z tracking. The sampling rate is 240 Hz, 50 Hz, and 25 Hz, respectively, for x-y-z and rotational tracking. The sampling range is 3 × 3 mm, ± 0.5 mm and ±15 degrees, respectively, for x-y-z and rotational tracking. The device was used in the study by Nuehann and associates with good clinical results.
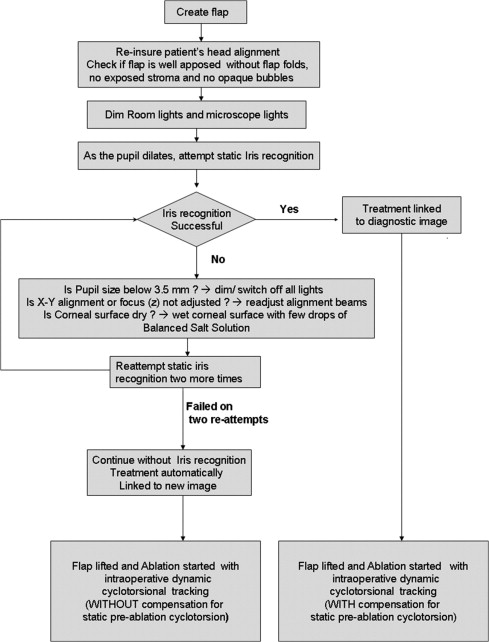
All the procedures were performed under topical anesthesia. After creation of the flap (and after sufficient clearing of the bubble layer in femtosecond flaps), static preablation iris recognition was attempted by matching a diagnostic iris image (obtained at acquisition on Zywave in the sitting position) to an image of the iris obtained by the laser platform in supine position. All the precautions, including reducing operating room and microscope illumination, preventing dryness of surface and defocusing, and waiting for the scotopic pupil to dilate to a size of more than 3.5 mm, were observed ( Figure 1 ).
Successful Preablation Static Iris Recognition
In case the iris was recognized successfully, the treatment was linked to the diagnostic image and the difference in cyclotorsion was accounted for and compensated for (static iris recognition and compensation). Further intraoperative dynamic tracking was performed by the laser platform by using the diagnostic image as the reference.
Failure of Preablation Static Iris Recognition
In case of failure of static recognition after 2 more attempts, the treatment was continued without iris registration and without compensation for misalignment between acquisition and treatment. However, these cases underwent dynamic rotational eye tracking during surgery, which was carried out with the help of a preablation new image obtained by the laser machine ( Figure 1 ). Preablation new image linking is a facility provided by the Techolas 217z100 in which a new intraoperative iris picture is obtained automatically in case of failed iris registration and is used as a guideline for measurement of cyclotorsion from that point onward. This ensures that at least intraoperative cyclotorsional movement is compensated for.
Tracking Difficulties After Successful Preablation Static Iris Recognition
In cases with successful iris recognition, the tracking was linked to the diagnostic image by the software and dynamic rotational tracking was continued. If there was an intraoperative failure of rotational intraoperative tracking, which was not tackled by realignment of the trackers and removal of ablation-induced debris and haze, an intraablation new iris image was captured during surgery and was linked with the treatment ( Figure 2 ). This user-triggered intraablation new image is different from the preablation new image, which is obtained automatically by the laser platform to ensure that at least dynamic intraoperative cyclotorsional tracking is continued in case of failed preablation iris registration. The intraablation new image took the cyclotorsional misalignment reference as the value noted last before tracking failure.
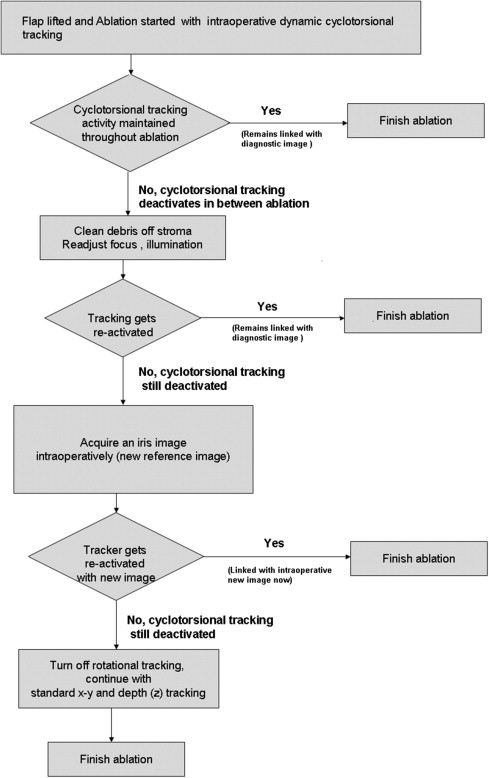
Nonresolvable Failure of Intraoperative Dynamic Rotational Tracking After Successful Preablation Static Iris Recognition
If the intraoperative new image also did not reactivate dynamic rotational tracking, the rest of the procedure was continued without rotational tracking, with active x-y-z tracking. The last recorded value of cyclotorsional misalignment was used in this scenario by the software to complete the ablation.
Intraoperative displays consisted of static post-iris recognition cyclotorsion and centroid shift measurements and mean and highest–lowest values of the intraoperative dynamic cyclotorsion. The amount of ablation performed in terms of depth of ablation, and number of laser pulses delivered was also noted.
Results
Patient Demographics
The study cohort comprised 275 eyes (140 right eyes and 135 left eyes) of 142 candidates undergoing LASIK surgery. There were 63 males and 79 females. One hundred thirty-three candidates underwent bilateral simultaneous surgery, 7 right eyes only and 2 left eyes only. The mean preoperative spherical error was −5.46 ± 3.40 diopters (D), ranging from −11 to 2.25 D; mean cylindrical error was −1.5 ± 1.09 D, ranging from 0 to −6.25 D. The mean age was 25.94 ± 5.05 years.
Treatment Interventions
Of the 275 procedures, 136 were Femtosecond laser flaps (Intralase 90- to 120-μm flaps); 96 were microkeratome-assisted stromal flaps (XP 120- or 140-μm flaps), and 43 were epi-LASIK flaps (XP episeparator 65-μm epithelial flaps). The ablation algorithm used was Tissue Saving Surgery mode for 115 eyes and Zyoptix Personalized (wavefront guided) for 160 eyes.
Preablation Iris Registration
Preablation iris registration was performed successfully in 247 of 275 eyes (89.8%). In all these cases, the procedure was linked to the diagnostic image. The mean amount of preablation static cyclotorsion (C S ) was −1.09 ± 4.46 degrees, ranging from −12.7 to 12.5 degrees ( Figure 3 ). Of these 247 eyes, 142 eyes had incyclotorsion, 95 had excyclotorsion, and only 10 had no cyclodeviation. The mean absolute value of static cyclotorsion (C S ) was 3.64 ± 2.79 degrees. Failure to have preoperative iris recognition was seen 28 eyes. There was no difference between number of eyes having successful or failed static iris recognition in the 3 flap groups: femtosecond (122/14), microkeratome (88/8), and epi-LASIK (37/6; P = .6, chi-square test).
Mean Intraoperative Position of Cyclodeviation
The mean intraoperative position during (C I ) during ablation was −1.03 ± 4.73 degrees, ranging from −13.5 to 13.5 degrees ( Figure 4 ). The absolute value of intraoperative cyclotorsion (C I ) was 3.81 ± 2.97 degrees. There was a strong correlation between C S and C I ( r = 0.9; P = 7.03 × 10 −94 ; Figure 5 ).
Absolute Range of Intraoperative Cyclotorsion
The absolute range of cyclotorsion movement seen during surgery was calculated as the absolute value of difference highest and lowest value of cyclotorsion. It was found to be 2.99 ± 1.53 degrees, ranging from 0.0 to 9.3 degrees. An overlay line and dot plot was drawn to show the trend of change in intraoperative cyclodeviation parameters as a function of preoperative cyclodeviation ( Figure 6 ).
Factors Predicting Absolute Range of Intraoperative Cyclotorsion
Regression analysis models were used to predict factors governing for absolute range of intraoperative cyclotorsion. Significantly predicting quantitative variables were age of the patient (partial correlation, −0.16; P = .014), amount of pulses (partial correlation, 0.39; P = 1.6 × 10 −8 ), and gender ( P = .02; males, 2.76 ± 1.46; females, 3.2 ± 1.5). There was no independent effect of eye (right or left, P = .1), method of flap creation (IntraLase, stromal XP flap, or epi-LASIK, P = .1), or ablation type (Tissue saving [TS] and Wavefront guided [WG], P = .08) on the absolute range of intraoperative cyclodeviation. There was poor, nonsignificant correlation with amount of static preablation cyclotorsion (partial correlation, 0.1; P = .1), spherical equivalent (partial correlation, 0.32; P = .6), optical zone (partial correlation, 0.05; P = .4), and depth of ablation (partial correlation, 0.02; P = .7).
Factors Predictive for Acquisition of an Intraoperative New Iris Image During Surgery After Successful Initial Recognition and Diagnostic Image Linkage
Of the 247 eyes in which iris registration could be performed successfully, 169 remained linked to the diagnostic image throughout the procedure. The remaining 78 required a new intraablation iris image because of failure of the dynamic tracker. Multivariate logistic regression was used to analyze the predictive variables for intraoperative new image linkage (suggestive of tracking difficulty). Significant likelihood ratios were seen with type of flap ( P = 6.8 × 10 −7 ) and the amount of intraoperative cyclotorsion ( P = .02). There was no significant association with age ( P = .7), gender ( P = .4), eye ( P = .4), ablation profile ( P = .8), pulses delivered ( P = .67), and spherical equivalent ( P = .7) had no effect on the requirement of a new image during surgery. Intragroup analysis of femtosecond flaps did not show a significant difference in number of cases requiring intraoperative linkage to a new image (diagnostic/new: 120 μm, 15/12; 110 μm, 14/11; 100 μm, 23/18; 90 μm, 12/17; P = .6, chi-square test). Intragroup analysis of microkeratome-based stromal flaps also did not reveal a difference in the requirement of intraoperative linkage to a new image (140 μm, 43/8; 120 μm, 34/3; P = .2, chi-square test).
Intragroup cross-tabulation evaluation of the flap creation method revealed significant differences between femtosecond (diagnostic/new, 64/58), epi-LASIK (28/9), and microkeratome (77/11) flaps, with the femtosecond group having maximum episodes of new image linkage ( P = 2.8 × 10 −7 ). For a similar attempted flap thickness (120 μm), the femtosecond flaps had a significantly higher number of episodes of flap linkage compared with microkeratome flaps (femtosecond, 15/12; microkeratome, 34/3; P = 7.1 × 10 −5 , chi square test). The detailed split of cases in terms of flap thickness attempted and achieved and diagnostic and intraoperative new image linkage is given in Table .



