Posterolateral Neck Dissection
Jeffrey N. Myers
INTRODUCTION
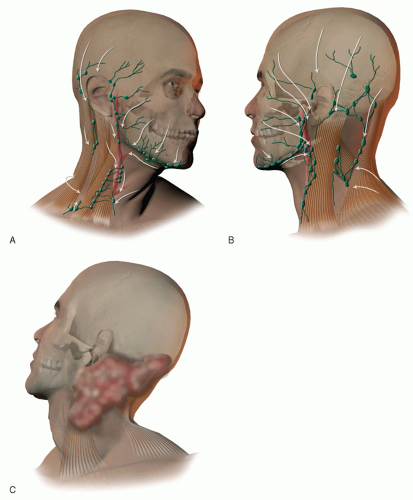
The posterolateral neck dissection is an operation that is typically used in the management of cutaneous cancers of the posterior scalp, auricle, or upper neck either electively to stage the clinically node-negative neck or therapeutically to treat the node-positive neck. In contemporary practice, this operation is most often used to treat a clinically node-negative neck that has been found to have microscopically positive nodal disease in one or more of the regional nodal basins. While a description of this operation was first published in 1962, Drs. Goepfert, Jesse, and Ballantyne of the MD Anderson Cancer Center wrote a definitive description of this procedure and their results with it in 1980. Typically, this operation involves the removal of the lymph nodes in the postauricular, suboccipital, spinal accessory and the jugular lymph node basins (Fig. 8.1). In experienced hands, this operation provides excellent oncologic, functional, and cosmetic results.
HISTORY
As the majority of patients undergoing this procedure will have skin cancer as the primary indication for the procedure, a history of prior skin cancers, including their histologic type, location, and treatment, will be very useful for treatment planning. In addition, sun exposure and family history are relevant to tumor management and surveillance after treatment. An occupational history is also useful, as this operation even when performed without complication can lead to decreased shoulder function for up to 10 to 18 months following surgery. Typically this is manifested by decreased range of motion and strength on shoulder abduction, which can be improved greatly with early intervention by a trained physical therapist with anticipated return to baseline.
PHYSICAL EXAMINATION
Visual evaluation and palpation of the extent of the primary tumor and nodal metastasis are traditionally part of the initial assessment of the patient for whom posterolateral neck dissection is being considered. This includes inspection of the scalp, auricle, and neck and palpation of the entire neck with particular attention to the post-auricular, suboccipital, spinal accessory and jugular nodal basins. The number and size of each involved node should be recorded and used as part of the clinical staging. Previous surgery in this area should be noted.
INDICATIONS
This operation is indicated in the management of cutaneous cancers of the posterior scalp, auricle, or the superior aspect of the neck either electively to stage the clinically node-negative neck or therapeutically to treat the node-positive neck. It is used most often to treat a clinically node-negative neck that has been found to have microscopically positive nodal disease in one or more of the regional nodal basins on sentinel lymph node biopsy.
CONTRAINDICATIONS
This operation is contraindicated in patients for whom the procedure would neither prolong survival nor provide significant palliation. This may include patients with disseminated metastatic cancer. Additionally, those patients with extensive lymph node metastasis with involvement of the deep muscles of the neck, vertebrae, or carotid artery are advised to consider systemic therapy options that could help decrease the risk of distantly metastatic disease and potentially make the local-regional disease burden more manageable by resection. Patients deemed to be medically high risk for general anesthesia, who have microscopic nodal disease, can often be managed successfully with radiation therapy alone.
PREOPERATIVE PLANNING
Imaging Studies
Cross-sectional imaging of the head and neck region is typically obtained to define the location and extent of the primary cancer and the presence of regional nodal metastases. This is most often accomplished with an axial computed tomography (CT) scan with contrast. However, a magnetic resonance imaging (MRI) or
positron emission tomography/computed tomography (PET/CT) may also be used. Systemic imaging may be indicated based on the histology and clinical stage of disease. For patients with melanoma or Merkel cell carcinoma with thick primary tumors or extensive lymph node metastasis, a PET/CT and brain MRI or brain MRI with CT scans of the head and neck, chest, and abdomen should be obtained.
positron emission tomography/computed tomography (PET/CT) may also be used. Systemic imaging may be indicated based on the histology and clinical stage of disease. For patients with melanoma or Merkel cell carcinoma with thick primary tumors or extensive lymph node metastasis, a PET/CT and brain MRI or brain MRI with CT scans of the head and neck, chest, and abdomen should be obtained.
Fine Needle Aspiration Biopsy
Patients found to have palpable lymph node metastasis may be recommended to have a fine needle aspiration biopsy (FNAB) of an involved node if the results will change the patient’s management. Such a case would be if the presence of histologically confirmed lymph node metastasis is part of the inclusion criteria for a protocol of neoadjuvant systemic therapy. In cases where the finding of lymph node metastasis is indeterminate by cross-sectional imaging criteria, ultrasound-guided FNAB may be used to confirm or rule out the presence of regional lymph node metastasis to facilitate treatment planning.
SURGICAL TECHNIQUE