Key points
- •
Detailed evaluation of preoperative imaging is essential for appreciating variants involving the skull base, orbital wall, bony irregularities, and critical structures such as the optic nerve and internal carotid artery (ICA).
- •
Orbital hemorrhage remains among the most feared surgical complications of sinus surgery. Once recognized, there should be a low threshold to perform lateral canthotomy/orbital decompression should conservative management fail.
- •
Topical corticosteroids have become a mainstay in the treatment of chronic rhinosinusitis (CRS) because limited systemic effects decrease the incidence of adverse effects. When systemic corticosteroids are necessary, potential deleterious sequelae to consider include metabolic derangements, gastrointestinal (GI) irritation, avascular necrosis, insomnia, and adrenal suppression.
- •
Potential complications of medical and surgical management of CRS should be discussed in a comprehensive informed consent process, which enhances the physician-patient relationship and minimizes medicolegal liability in the event of an unsatisfactory outcome.
| CRS | Chronic rhinosinusitis |
| CSF | Cerebrospinal fluid |
| CT | Computed tomographic |
| EOM | Extraocular muscles |
| ESS | Endoscopic sinus surgery |
| GI | Gastrointestinal |
| ICA | Internal carotid artery |
| IGS | Image guidance system |
| NLD | Nasolacrimal duct |
The hardest part of the operation is to recognize the limits of this [posterior ethmoid] cell. It is in this cell that he can get into the most trouble. Working in this cell, especially in its upper outer posterior angle, is the most dangerous part of the whole procedure. Experience has proved that it can be easily fatal to the patient if the operator loses his bearings in this locality.
Despite significant strides in the surgical and medical treatment of CRS over the past century, a potential for unfavorable outcomes persists because of the intimate relationship between the paranasal sinuses and the surrounding structures. Familiarity with the complex anatomic relationships between the skull base and other critical structures and knowledge of pharmacologic properties of commonly used medical therapies are essential for preventing serious and harmful complications. The authors hope that this review serves as a valuable addition to the otolaryngologist-in-training’s therapeutic armamentarium and also serves as a reminder of potential pitfalls for the experienced sinus surgeon. Rather than providing an all-encompassing listing of complications, this review focuses on some of the most common and most severe adverse events encountered as a result of therapy for CRS ( Tables 1 and 2 ).
| Complication | Cause | Prevention |
|---|---|---|
| Orbital | ||
| Extraocular muscle injury (dysmotility, transection, entrapment, CN III injury) | Direct injury; medial orbital wall disruption resulting in orbital fat prolapse and poor visualization; entrapment of medial rectus/inferior oblique muscle by fracture fragments | Evaluate CT preoperatively for MOW variant, stop dissection if MOW breached |
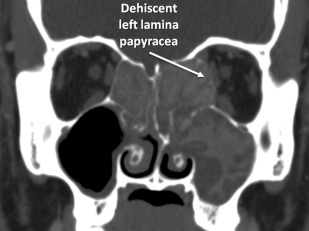
| Violation of lamina papyracea | Disruption of uncinate when its attachment is to the lamina, poor visualization | Evaluate CT preoperatively for uncinate attachment |
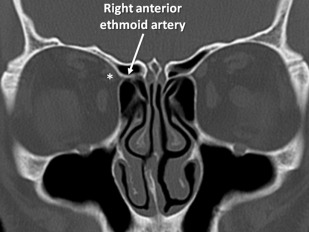
| Hemorrhage/hematoma | Venous or arterial causes; disruption of anterior ethmoidal artery located in ethmoid sinus mesentery | Note location of ethmoidal arteries on preoperative CT; divide anterior ethmoidal artery closer to cribiform, away from orbit |
| Nasolacrimal duct injury | Injured anywhere along its course, most commonly during inferior turbinectomy or uncinectomy | Use of 30°/45° endoscope to see maxillary ostia (anterior limit of dissection) |
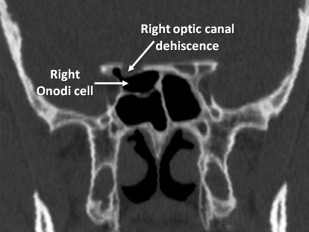
| Direct optic nerve injury | Disruption of Onodi cell during sphenoid sinusotomy | Evaluate preoperative CT for location of CN II and presence of Onodi cell |
| Neurologic/Intracranial | ||
| Cerebrospinal fluid rhinorrhea/direct injury to the brain | Aggressive skeletonization when disease abutting SB; not appreciating skull base variants | Evaluate preoperative CT for SB variants including Keros, determine extent of SB-abutting disease, consider IGS use in complicated cases |
| Anosmia | Disruption of olfactory nerve fibers | As above |
| Vascular | ||
| Ethmoidal artery injury (see hemorrhage/hematoma above) internal carotid artery injury | Dehiscence in sphenoid; Onodi cell | Evaluate preoperative CT |
| Medication | Side Effects/Complications |
|---|---|
| Antibiotics a | |
| Macrolides (roxithromycin, azithromycin) | QT prolongation, ototoxicity |
| Fluoroquinolones | GI disturbance, tendon rupture (increased risk with corticosteroid use), QT prolongation, peripheral neuropathy |
| Cephalosporins | GI disturbance, rash |
| Penicillins | GI disturbance (diarrhea), rash |
| Doxycycline | Teeth/bone defects (children), teratogen, rash (during sun exposure) |
| Trimethoprim/sulfamethoxazole | GI disturbance, thrombocytopenia, hyperkalemia, neutropenia, jaundice/hepatitis |
| Antifungals a | |
| Amphotericin B | Infusion reaction, renal toxicity, liver toxicity, hypokalemia |
| Terbinafine | GI disturbance, paresthesias, pancytopenia/leukopenia, insomnia, agitation, rashes, jaundice |
| Corticosteroids a | Weight gain, hyperglycemia/diabetes, psychosis, GI disturbances, avascular necrosis, striae, ophthalmologic disturbances (glaucoma exacerbation, cataracts), hepatotoxicity, acne, adrenal suppression |
| Allergen immunotherapy | Urticaria/rash, flulike symptoms, anaphylaxis, GI disturbance/ulcers (aspirin desensitization therapy) |
a Side effects/complications listed refer to systemic therapy; these adverse events are exceedingly rare/not associated with topical therapies.
Complications of surgical therapy
Orbital Complications
The close proximity of the orbital contents to the paranasal sinuses necessitates a detailed understanding of the anatomy and encountered complications. Complications can be as severe as direct optic nerve injury, which is uncommon but generally not treatable, or mild orbital emphysema, which is usually managed conservatively. Several of the more common and treatable complications are detailed in the following discussion.
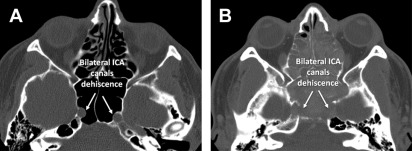
Orbital complications from endoscopic sinus surgery (ESS) are fortunately uncommon, with recent analyses offering varying rates from 0.07% to 0.23%, significantly less than the rates reported before the endoscopic era. Compromise of orbital structures can have significant vision-related consequences. Accordingly, diligent preoperative preparation is invaluable. Appreciation of anatomic variants is paramount. The preoperative computed tomographic (CT) image should be examined for integrity of the lamina papyracea ( Fig. 1 ), as well as whether the uncinate process is positioned against the medial orbital wall. It should be determined if Onodi cells, posteriorly located ethmoidal air cells directly superior to the sphenoid sinus, are present. The optic nerve and ICA may be located within or in close proximity to Onodi cells and may be exposed by dehiscences within these cells; therefore, identifying whether Onodi cells are present on preoperative CT is crucial in avoiding optic nerve and ICA injuries during posterior ethmoidectomy ( Fig. 2 ).
Imaging should also be done to determine the position of the lacrimal apparatus (sac and duct) as well as the location of the ethmoidal arteries ( Fig. 3 ). The opening of the nasolacrimal duct (NLD) (the Hasner valve) is typically located 3 to 4 mm behind the insertion of the inferior turbinate, while the duct and sac lie just anterior to the root of the uncinate process. The NLD has a variable but close relationship to the maxillary sinus ostium, putting this structure at risk during maxillary antrostomy. The occult incidence of injury to the NLD during ESS was reported to be 15% in Bolger and colleagues’ cohort, although epiphora from injury occurred in less than 2% of injuries. Hence, even though NLD injury is relatively common, clinical complaints are not. Patients experiencing postsurgical epiphora should be referred for ophthalmologic examination. Sinus surgeons should include epiphora in the list of potential risks in the preoperative informed consent discussion, because this troublesome symptom has been raised in medicolegal proceedings.
Although uncommon, disruption of the extraocular muscles (EOM) is another serious injury that can occur during ESS. Significance can range from dysmotility alone, which can be simply observed, to direct EOM injury, entrapment, and injury to the oculomotor nerve. Orbital fat prolapse can be problematic because of its attachments to the EOM, with the medial rectus being most commonly affected. There are a variety of therapeutic approaches for muscular transection, which are beyond the scope of practice for otolaryngologists, but entrapment associated with medial orbital wall compromise is a surgical emergency that can be addressed by debridement of fractured bony fragments. Immediate ophthalmologic consultation is usually helpful. Failure to obtain timely ophthalmologic consultation in these instances has been a factor in malpractice litigation. Iatrogenic medial rectus injury may also be associated with orbital hemorrhage; one series found that one-fourth of patients had hemorrhage and required subsequent orbital decompression.
Orbital hematoma remains one of the most feared complications of ESS. It is the most common orbital adverse event, with a wide variety of presentations, ranging from edema and chemosis to blindness. Hematoma can be either venous or arterial in origin, and understanding the differences in presentation and management is critical. The anterior ethmoidal artery is a common culprit, because this structure is located in the ethmoid sinus, adjacent to the superior oblique muscle in as many as 40% of cases (see Fig. 3 ). The authors cannot emphasize enough the importance of preoperative radiographic evaluation, which involves identifying the location of this structure. If it is located extracranially, awareness of its location and planned transection (if necessary) away from the orbit and closer to the cribriform plate may prevent its retraction into the orbit, or leave more remaining vasculature (for adequate vascular control) if partial retraction occurs, minimizing the chances of retrobulbar hemorrhage. Retrobulbar hemorrhage usually results from an arterial source with significant and sudden swelling occurring over a period of minutes, significant pain, visual abnormalities, bruising, and proptosis. Once recognized, orbital hemorrhage should be managed emergently by removing nasal packing, elevating the head from a horizontal position, and taking other measures such as administration of mannitol and systemic steroids. These measures should usually precede surgical management. If no relief is noted, further measures include immediate ophthalmologic consultation, lateral canthotomy, and orbital decompression. Notably, a lower threshold should exist for pursuing more aggressive surgical therapy when the cause of the bleed is thought to be arterial. Tonometry is important in diagnosis, because the degree of proptosis may not necessarily correlate with intraocular pressure.
Neurologic and Intracranial Complications
Cerebrospinal fluid (CSF) leak remains among the more common major complications of ESS. Although older studies have estimated the incidence of intracranial complications, including CSF leaks, at approximately 0.5%, these figures likely overestimate this complication, particularly in light of advances in technology facilitating enhanced visualization and image guidance. An analysis of clinical characteristics of patients undergoing primary ESS in California and Florida from 2005 to 2008 noted “skull base complications” in 103 of 78,944 patients (0.13%). This figure may be higher in certain scenarios, such as revision sinus surgery or in patients with complicated chronic sinus disease. Furthermore, a significant number of CSF leaks may go undetected clinically. Bachmann and colleagues reported an incidence of occult CSF fistula of 2.9% through β-trace protein testing; further study with greater study population sizes may be needed for more definitive estimates.
CSF rhinorrhea may lead to several serious sequelae, the most common of which is meningitis. Reviewing charts from 111 patients with CSF rhinorrhea over a 12-year period, Daudia and colleagues reported an overall risk of meningitis approaching 20% before repair, calculating incidence at 0.3 episodes annually. Although the risk of developing meningitis is highest in the first year after diagnosis, it persists beyond this period while a leak is active. This risk may vary with the cause of CSF leak (traumatic, iatrogenic, or spontaneous). The management and indications for antibiotic prophylaxis remain an active area of study, with varying strategies reported. Consideration should be given to include meningitis as a risk in the informed consent process.
Preoperative assessment of variable skull base anatomy is key to preventing skull base compromise and intracranial complications. Any dehiscence in the skull base should be noted on imaging in the preoperative assessment ( Fig. 4 ). The presence of disease abutting the skull base with suspicion or confirmation of dehiscence alerts the operating surgeon to be more careful during the procedure and to consider limiting the degree of skeletonization of the skull base to prevent intracranial penetration (see Fig. 4 ). Keros’ classification of skull base topography is important in the preoperative evaluation. The length of the lamina lateralis ( Fig. 5 ) affects the likelihood of skull base violation and can be used to determine how aggressive a surgeon should be in this area. A type III Keros lamina lateralis (depth of 8–16 mm), as identified on preoperative imaging, is much more likely to be breached intraoperatively (see Fig. 5 C). Although present in only approximately 1% of the population, recognition of this anatomic variant is crucial; a sinus surgeon may want to be much more conservative in cases with this skull base configuration. Preoperative CT evaluation should note any asymmetry in Keros configuration between the 2 skull base sides because this may also lead to complications when not recognized.

Anosmia and Endoscopic Sinus Surgery
Olfactory deficits can be iatrogenic, particularly when olfactory elements in the cribriform area are disrupted during sinus and skull base surgical intervention. As nearly two-thirds of patients with CRS complain of dysosmia preoperatively, it is difficult to estimate the extent to which iatrogenic disruption leads to this complication. One survey of 184 patients undergoing nasal surgeries noted that 4 patients (2.5%) reported new olfactory deficits postoperatively. Despite the unclear incidence of this complication, postoperative anosmia has been anecdotally noted as a factor in patients pursuing medicolegal action, and most litigations relating to anosmia involve patients who had undergone rhinologic procedures, with average jury-awarded damages exceeding $400,000. Many surgeons do not include this potential complication in the preoperative informed consent process, but perhaps should given the litigation history involving anosmia.
Other Vascular Injuries
Disruption of the ethmoidal arteries and the potential for associated orbital complications has already been discussed. An exceedingly rare but far more critical complication is ICA injury, most often occurring during sphenoid sinusotomy. Profuse bleeding during a case and subsequent poor visualization of the surgical field often accompany this event. Knowledge of skull base anatomy as well as appropriate surgical technique is important for prevention. The operating surgeon should be aware that the ICA is only protected by a thin wall (<0.5 mm), which may be entirely dehiscent in up to a quarter of patients ( Fig. 6 ). ICA dehiscence can be a normal anatomic variant (see Fig. 6 A) or may be secondary to destruction or deossification from disease processes (see Fig. 6 B). This fact again emphasizes the importance of carefully reviewing CT scans preoperatively and identifying unique anatomic considerations in each patient. Suggested protocols for management vary, but nasal and pharyngeal packing while applying pressure on the ipsilateral common carotid artery before transfer to an angiographic suite for endovascular management is a commonly suggested strategy.