There are many approaches to obtaining a workable endoscopic surgical field in sinus surgery. With extended sinus and transdural endoscopic surgery, a more rigid approach must be taken. There are 3 main factors that invariably lead to poor surgical outcomes in endoscopic sinus and skull base surgery: bleeding, inadequate access, and unidentified anatomic anomalies. Bleeding is arguably the most common reason for incomplete resection. An understanding of microvascular and macrovascular bleeding allows a more structured approach to improve the surgical field in extended endoscopic surgery. The endoscopic surgeon should always be comfortable in performing the same procedure as an open operation. However, converting or abandoning an endoscopic procedure should rarely occur because much of this decision making should take place preoperatively. Along with poor hemostasis, inadequate access is an important cause of poor outcome. Evaluation of the anatomy involved by pathology but also the anatomy that must be removed to allow adequate exposure is important. This article reviews the current techniques used to ensure optimal surgical conditions and outcomes.
There are 3 main factors that invariably lead to poor surgical outcomes in endoscopic sinus and skull base surgery: bleeding, inadequate access, and unidentified anatomic anomalies.
Bleeding is arguably the most common reason for incomplete resection, and not just for endoscopic cases. Poor hemostasis can lead to increased difficulty in recognizing the most important anatomic landmarks and identifying the sinus outflow pathways. It enhances the risks of intraoperative complications and postoperative scarring. Most importantly, it can lead to an incomplete operation. Inadequate access is often a product of incomplete exposure and failure to identify the limitations of the endoscopic approach in preoperative assessment and planning. The paranasal sinus anatomy represents one of the most highly variable anatomic areas within the body. Since the beginning of sinus surgery, surgeons have stressed the importance of preoperative radiographic assessment of potential anatomic anomalies. Failure to identify simple abnormalities, such as dehiscent medial orbital walls and orbital contents in the ethmoid, can lead to lifelong debilitating diplopia.
This article discusses bleeding control and access as it relates to endoscopic sinus and skull base surgery. Much has been written about careful radiologic evaluation for anatomic anomalies, and this will be addressed in a separate article.
Hemostasis
There are many approaches to obtaining a workable endoscopic surgical field for sinus surgery. However, with extended sinus and transdural endoscopic surgery, a more rigid approach must be taken.
Diffferent techniques are required for control of arterial, venous, or microvascular bleeding. These include topical and local vasoconstriction, patient positioning, anesthetic technique, dissection techniques to reduce bleeding, surgical control of large vessels, embolization, and agents to control venous and microvascular bleeding.
The Vascular System of the Nose
The vascular system of the nose is supplied by large arteries, the most clinically important of which are the sphenopalatine and anterior ethmoid. These progressively divide into smaller arteries, then arterioles. The arterioles are the resistance vessels, and regulate blood flow into capillary beds and arterovenous anastomoses. The main adrenergic receptor subtype is α 1 , which has implications for the use of vasoconstrictive agents. There is a copious system of fenestrated capillaries under the nasal mucosa. In addition, there are venous sinuses or capacitance vessels that have a thick layer of smooth muscle. The blood volume within the capacitance vessels to a large extent determines swelling of the nasal lining, such as in the nasal cycle. The predominant adrenergic receptor subtype in these vessels is believed to be α 2 . In addition to these capacitance vessels, there are many arterovenous anastomoses, which are believed to bypass the capillary beds and capacitance vessels and have a role in temperature and humidity control. Postcapillary venules, also predominantly α 2 , drain the capillary beds, capacitance vessels, and arterovenous anastomoses. In addition to the adrenergic receptors, there are other receptor types and neural control of the nasal mucosa. An understanding of this adrenergic organization is important in determining vasoconstrictor use.
Exposure of bone, intentionally through drilling and unintentionally through mucosal stripping, has a significant effect on hemostasis. The bone haversian canal system comprises 15 to 20 μm–wide endothelial-lined structures. These blood-filled channels have no smooth muscle (and thus are not responsive to adrenergic stimulation) or elastic fibers. Hemostasis only occurs with clotting pathway activation.
Microvascular Control (Capillary, Postcapillary Venules, and Small Arterioles)
Preoperative
Reducing obstructive inflammation and infective processes
The use of preoperative antibiotics and steroids is common, although there is only a small evidence base for their use. Anecdotally, the authors have found that large tumors predispose to obstructive inflammatory sinus changes. This predisposition results in a moderate degree of edema in the mucosal lining of areas not directly involved with tumor. Preoperative steroids are potent antiinflammatory agents, potentially reducing intraoperative bleeding. In addition to their antiinflammatory actions they potentiate the effect of adrenalin on smooth muscle, possibly prolonging topical vasoconstriction. Sieskiewicz and colleagues found an improvement in surgical field in 18 patients with severe nasal polyposis undergoing endoscopic sinus surgery (ESS) with preoperative steroid treatment compared with placebo.
Preoperative antibiotic use is intended to reduce bacterial load (or treat overt infection) and resultant inflammation to reduce intraoperative bleeding and optimize postoperative healing.
This practice affords better operative conditions and earlier recovery of regenerating mucosa. Comorbidities allowing, the authors start oral prednisone and antibiotics for 7 days before surgery. This decision is based on endoscopic and radiological assessment and not on clinical symptoms.
Bleeding diathesis
The hemostatic system is a complex cascade of enzyme activation and inhibition that results in a balance between pro- and anticoagulation. It consists of 3 main components: platelets and other blood cells, plasma proteins, and the vessel wall. The response to vascular injury consists of platelet adherence and plug formation (primary hemostasis), protein activation and the coagulation cascade (secondary hemostasis), feedback mechanisms to control coagulation, and lysis and recannulation.
Inherited coagulopathies
The most common inherited abnormalities of the coagulation system are von Willebrand disease and hemophilia ( Table 1 ). Von Willebrand disease is a heterogeneous, autosomally inherited condition affecting 1% to 2% of the population in which there is a defect in production of von Willebrand factor (vWF). VWF has 2 functions: to act as glue between platelets and subendothelial collagen, thereby promoting formation of the platelet plug, and to transport factor VIII (FVIII). Defects in vWF can result in impaired platelet adhesion and reduced levels of FVIII. Most cases are mild, with severe disease occurring in 1:10,000 to 2:10,000 people. Patients are often asymptomatic and present only after surgery, or may present with mucosal bleeding, petechiae, and purpura. There are several subtypes of vWD depending on the type (quantitative vs qualitative) and severity of the defect in vWF (see Table 1 ). Most cases will respond to desmopressin (DDAVP) (intravenous infusion of 0.3 μg/kg over 20 to 30 minutes; nasal use is variable and not recommended preoperatively ), which causes release of vWF, FVIII, and plasminogen activator from storage sites. Type III is not responsive to DDAVP and use in type IIB is debated because of platelet aggregation resulting in a reversible reduction in platelet count. A test dose can be given with measurement of FVIII and vWF: ristocetin cofactor at 30 minutes after infusion to determine responsiveness.
| Name | Effect |
|---|---|
| Alfalfa | Contains coumarins Also high levels vitamin K |
| Arnica | Platelet aggregation inhibitor Contains coumarins |
| Bilberry | Platelet aggregation inhibitor |
| Black currant | Platelet aggregation inhibitor |
| Bladderwrack | Platelet aggregation inhibitor Fibrin formation inhibitor |
| Black cohosh | Bradycardia, peripheral vasodilation |
| Capsicum | Platelet aggregation inhibitor Contains coumarins Hypertension |
| Cayenne fruit | Platelet aggregation inhibitor Fibrin formation inhibitor |
| Celery | Platelet aggregation inhibitor Contains coumarins |
| Chamomile | Contains coumarins |
| Da huang | Platelet aggregation inhibitor |
| Dandelion root | Inhibits clotting |
| Danshen | Platelet aggregation inhibitor |
| Devil’s claw | Platelet aggregation inhibitor |
| Dong quai | Platelet aggregation inhibitor |
| Ephedra | Arrhythmias, myocardial infarction, stroke |
| Evening primrose seed oil | Platelet aggregation inhibitor |
| Fenugreek | Contains coumarins |
| Feverfew | Platelet aggregation inhibitor |
| Fish oil | Platelet aggregation inhibitor |
| Flax seed oil | Platelet aggregation inhibitor |
| Garlic | Platelet aggregation inhibitor Fibrin formation inhibitor |
| Ginger | Platelet aggregation inhibitor Bradycardia |
| Gingko | Platelet aggregation inhibitor (inhibits platelet activation factor) |
| Ginseng | Platelet aggregation inhibitor Fibrin formation inhibitor Hypertension |
| Grape seed extract | Platelet aggregation inhibitor |
| Horse chestnut | Contains coumarins |
| Horseradish | Contains coumarins |
| Kava kava | Platelet aggregation inhibitor May cause liver failure Sedative |
| Licorice | Platelet aggregation inhibitor Contains coumarins Hypertension Hypokalemia |
| Meadowsweet | Platelet aggregation inhibitor |
| Motherwort | Contains coumarins |
| Papaya | Platelet aggregation inhibitor |
| Passionflower | Contains coumarins |
| Poplar | Platelet aggregation inhibitor |
| Red clover | Contains coumarins |
| St John’s wort | Cytochrome P450 inducer; increases metabolism of many drugs including warfarin |
| Sweet clover | Contains coumarins |
| Tamarind | Increases bioavailability of aspirin and ibuprofen |
| Tumeric | Platelet aggregation inhibitor |
| Valerian | Potentiate sedative effects of anesthesia |
| Vitamin E | Platelet aggregation inhibitor |
| Willow bark | Platelet aggregation inhibitor |
Hemophilia A and B are X-linked recessive deficiencies of FVIII and factor IX (FIX) respectively. There is a spectrum of disease from mild to severe. Presentation is typically with muscle hematomas and hemarthrosis, in contrast to platelet disorders and vWD. Treatment of hemophilia A may be with DDAVP in mild cases, or with FVIII concentrates in moderate to severe cases. FIX concentrate is used for hemophilia B. Other, rare conditions of primary and secondary hemostasis are summarized in Table 2 .
| Disorder | Types | Mechanism | Typical Presentation | Inheritance | Incidence/Prevalence | Treatment |
|---|---|---|---|---|---|---|
| von Willebrand disease | All | Defects in vWF with secondary FVIII deficiency | Mucosal bleeding, petechiae, purpura may be asymptomatic, basic laboratory tests variable, may be normal or have abnormal PFT Specific tests: vWF:Ag vWF:RCo vWF:CB vWF:FVIIIB | Prevalence mild: 1%–2% severe: 1:5000–10,000 | Antifibrinolytics (tranexamic acid, ε-aminocaproic acid) may be useful for mucosal bleeding | |
| I | Quantitative vWF deficiency | Autosomal dominant with variable penetrance | 70%–80% of cases | DDAVP | ||
| IIA | Qualitative vWF deficiency | 15%–20% of cases, IIa most common | DDAVP | |||
| IIB | Cryoprecipitate or concentrates containing vWF DDAVP debated; causes drop in platelet count | |||||
| IIM | DDAVP | |||||
| IIN | Autosomal recessive | DDAVP | ||||
| III | Severe quantitative vWF and secondary FVIII deficiency | May present as hemophilia | Autosomal recessive | 5% of cases | Cryoprecipitate or concentrates containing vWF Not responsive to DDAVP | |
| Hemophilia | A | FVIII deficiency | Hemarthrosis, muscle hematomas APTT prolonged PR normal | X-linked recessive | 1:5000 male births | DDAVP for mild cases FVIII concentrate |
| B | Factor IX deficiency | X-linked recessive | 1:25,000 male births | FIX concentrate or cryoprecipitate | ||
| C | Factor XI deficiency | As mild hemophilia A | Autosomal recessive | Rare | FXI concentrate | |
| Rare clotting factor defects | Factor I (fibrinogen) deficiency | Severe cases: difficulty with implantation of embryo into uterine wall, miscarriage, bleeding | Autosomal recessive | All rare. FVII deficiency most common, FII deficiency least common | Fibrinogen | |
| Factor II (prothrombin) deficiency | As hemophilia | Plasma or prothrombin complex concentrate | ||||
| Factor V deficiency | All autosomal recessive, heterozygotes may be mildly symptomatic | Plasma | ||||
| Combined FV and FVIII deficiency | Prolonged PR and APTT | Plasma or FVIII concentrate | ||||
| Factor VII deficiency | PR prolonged, APTT normal | FVII concentrate | ||||
| Factor X deficiency | PR and APTT prolonged | Plasma or prothrombin complex concentrate | ||||
| Factor XIII deficiency | PR and APTT prolonged | Plasma or FXIII concentrate | ||||
| Rare platelet defects | Adhesion defects (eg, Bernard-Soulier syndrome | Gp Ib-X deficiency (platelet membrane receptor for vWF) | Mucosal bleeding, petechiae, purpura | Autosomal recessive | Rare | Platelet transfusions if required |
| Aggregation defects (eg, Glanzman thrombasthenia) | Gp IIb–IIIa deficiency (platelet membrane receptor for fibrinogen) | |||||
| Secretion defects (storage pool disorders) | Defective release of mediators | Variable | ||||
Acquired coagulopathies
Clotting abnormalities can be due to a wide variety of conditions and a thorough medical and drug history should be taken ( Tables 3 and 4 ). Anticoagulant and antiplatelet medications are a common cause of clotting abnormalities ( Table 5 ). Antiplatelet and anticoagulant agents should be stopped for surgery. Most patients will have strong indications for anticoagulation and require the use of bridging medications (heparin, low molecular weight heparin, or nonsteroidal antiinflammatory drugs [NSAIDs]). The authors generally cease bridging therapy within 7 days for extradural and between 7 and 14 days for intradural procedures.
| Bleeding Type | Suggestive of: |
|---|---|
| Epistaxis | Very common; does not necessarily indicate bleeding disorder but is most common presentation of vWD Hereditary hemorrhagic telangectasia |
| Oral mucosal bleeding | Platelet disorders/vWD Bleeding with tooth eruption suggestive of moderate to severe hemophilia |
| Excessive bruising | Platelet abnormality/vWD Blood vessel abnormalities (Ehlers-Danlos syndrome, chronic steroid use, aging) |
| Muscle hematomas or hemarthroses | Hemophilia/factor deficiencies |
| Excessive bleeding after surgery or trauma | Nonspecific |
| Menorrhagia | Nonspecific |
| Postpartum hemorrhage | Nonspecific |
| Component | Problem | Causes | Examples |
|---|---|---|---|
| Platelet plug | Decreased production | Drugs Nutritional deficiencies Infections Bone marrow disorders | Alcohol, thiazides, cytotoxics Vitamin B 12 , folate HIV Aplastic anemia, myelodysplastic syndromes, leukemia, lymphoma |
| Decreased survival | Autoimmune Drug induced Infections Sequestration Consumption | Primary: idiopathic thrombocytopenic purpura Secondary: SLE Heparin, quinine, vancomycin HIV, infectious mononucleosis Hypersplenism Thrombotic microangiopathies, giant hemangiomas, DIC | |
| Impaired function | Autoimmune Drug induced Uremia; complex effects on adhesion, aggregation, and secretion | Acquired vWD (autoantibodies vs vWF; see Table 5 ) | |
| Clotting factors | Decreased production | Drugs Nutritional deficiency Liver failure | Warfarin Vitamin K deficiency |
| Decreased survival | Consumption Autoimmune | DIC Inhibitory autoantibodies | |
| Impaired function | Drugs | Heparin |
| Medication | Actions | Stop Before Surgery | Antidote |
|---|---|---|---|
| Warfarin | Inhibits vitamin K–dependent clotting factor synthesis (factors VII, IX, X, II) Also inhibits protein C synthesis (procoagulant effect); can result in hypercoagulable state in first 24 h of therapy | 2–4 d | Vitamin K Fresh frozen plasma or factor IX complex (purified factor IX preparations do not contain II, VII, and X) |
| Heparin | In combination with antithrombin III, inactivates factors Xa and IIa Risk of heparin-induced thrombocytopenia (HIT, up to 30%) Type I most common, mild, direct effect of heparin on platelets. Onset 1–4 d after commencement of therapy Type II: antibody-mediated activation of platelets resulting in severe intravascular coagulation. Onset 7–11 d after commencement of therapy | 6 h | Protamine |
| Low molecular weight heparin | As heparin, major action on factor Xa Low risk of HIT but contraindicated in patients who have had HIT | 12–24 h | Protamine (partial reversal) |
| Aspirin and NSAIDs | Blocks production of thromboxane A2 in platelets by inhibiting cyclooxygenase. Aspirin, irreversible inhibition; NSAIDs, reversible | Aspirin: 7–10 d | None |
| Thienopyridines (clopidogrel, ticlopidine) | Inhibit ADP-induced platelet aggregation by altering a platelet receptor for ADP | Clopidigrel: 5–10 d Ticlodipine: 10 d | None |
| Gp IIb/IIIa receptor antagonists | Bind to Gp IIb/IIIa receptor inhibiting platelet binding to fibrinogen and vWF | 24–72 h | None (Tirofiban; hemodialysis) |
Many alternative therapies and dietary supplements have reported or potential effects on coagulation (see Table 1 ). Their use is ubiquitous, with up to 27% of presurgical patients taking supplements or alternative therapies that are believed to affect bleeding, whereas 70% of patients do not report their use to their doctor. The American Society of Anesthesiologists recommends cessation of all herbal medications 2 to 3 weeks before surgery, although more specific recommendations are available for certain products.
Preoperative assessment of bleeding risk
A careful history should be taken to assess the risk of bleeding. Medical conditions and the use of medications and alternative therapies should be assessed as well as a specific bleeding history (see Table 3 ). The routine use of coagulation studies in asymptomatic patients has not been shown to be of any benefit in predicting the risk of bleeding, changing management, or altering outcomes. In patients with a history suggestive of bleeding tendency, laboratory testing may be indicated.
Testing of platelet function has traditionally been with platelet count and an assessment of bleeding time; however, the reliability of bleeding time testing is low and it has not been found to predict operative bleeding. Tests of clot viscoelastic strength, such as the thromboelastogram (TEG) and the Sonoclot, test all the components of the coagulation system and are better at predicting perioperative bleeding than routine tests. Results from the platelet-activated clotting factor test (PACT, Coulter Electronics, Hialeah, FL) and the PFA100 (Dade International, Miami, FL) are mixed and they are believed to be less sensitive than the TEG.
Suggested tests in patients with a history suggestive of a bleeding abnormality include activated partial thromboplastin time (APTT), prothrombin ratio (PR), platelet count, fibrinogen, and vWD panel (see Table 1 ) or TEG. If abnormalities are detected, specific factor assays can be performed to further evaluate the bleeding abnormality.
Intraoperatively
Anesthetic technique
Anesthetic techniques can potentially affect bleeding and the surgical field. These include the type of airway, the degree of hypercapnia, and the anesthetic agents used.
The airway used in ESS is typically a reinforced laryngeal mask airway (LMA) or endotracheal tube (ETT). Early concerns regarding airway protection with the LMA have not been borne out, with one study showing significantly fewer instances of blood in the upper airway with LMA compared with ETT (20% vs 85%). There was a trend toward increased blood in the distal airway with LMA but no complications related to this. The pressor effect of LMA insertion is significantly lower than for ETT. Atef and Fawaz compared LMA with ETT in ESS. The ETT group had higher heart rate (HR) and blood pressure (BP) and worse surgical field at 15 minutes, which resolved by 30 minutes after insertion.
The use of spontaneous ventilation may result in normal to high CO 2 levels, whereas the use of muscle relaxants and mechanical ventilation allows normal or low levels to be achieved. Increasing CO 2 levels cause smooth muscle relaxation and vasodilation, potentially increasing bleeding. However, Nekhendzy and colleagues examined the effect of different end tidal CO 2 levels on the surgical field and blood loss in patients undergoing ESS. There was no difference in blood loss or surgical field between hyper-, hypo-, or normocapnia groups. However, the hypocapnia group had significantly greater requirements for remifentanyl and antihypertensive medications, suggesting limited benefit for the use of hypocapnic techniques.
A summary of studies of the effects of various anesthetic techniques on bleeding in ESS is given in Table 6 . Nine studies compared an intravenous propofol/opioid-based anesthetic with an inhalational agent supplemented with opioid. Seven favored the propofol arm, with lower blood loss or improved surgical field. Of the remaining 2 studies, 1 compared 3 arms and showed improved surgical field with propfol/remifentanyl and sevoflurane/sufentanil compared with isoflurane/fentanyl. There was no difference in BP and the HR was not reported in this study. The final study in this group compared propofol/fentanyl with sevoflurane/fentanyl. There was no difference in surgical field or, importantly, HR between the 2 groups.
| Study | Comparison | Outcome Measures | n | Findings |
|---|---|---|---|---|
| Ahn et al, 2007 | Total intravenous anesthetic (TIVA) (P/R) vs S/R | Blood loss Surgical conditions (numeric rating scale 1–10) | 40 | BP: no significant difference (NSD) HR: lower in propfol/remifentanyl group Lund-Mackay≤12: NSD Lund-Mackay>12: Blood loss: P/R significantly improved Surgical field: P/R significantly improved |
| Atef and Fawaz, 2008 | Laryngeal mask vs endotracheal intubation (all TIVA with P/R) | HR, BP Surgical field: Boezaat rating scale | 60 | Laryngeal mask: shorter time to achieve target BP Lower doses of remifentanyl required |
| Beule et al, 2007 | S/F vs P/F Lund-Mackay>12 | HR Blood loss Blood loss/min Platelet function Surgical field (VAS) | 52 | HR: NSD Blood loss: NSD Blood loss/min: NSD Surgical field: NSD Platelet function: impaired in both groups, worse in P/F group |
| Blackwell et al, 1993 | P vs I. Retrospective review, groups different age, sex, weight | Blood loss | 25 | Blood loss: improved in P group |
| Boezaart et al, 1995 | Sodium nitroprusside vs esmolol. Hypotension induced and assessments made at 5 mm BP increments | Surgical field: rating scale 0–5 at different BPs | 20 | Esmolol group: HR lower Surgical conditions improved |
| Cincikas and Ivaskevicius, 2003 | Normotension vs hypotension (induced with captopril premedication and GTN infusion) Unblinded | HR Surgical field: Boezaart rating scale Blood loss | 52 | Hypotension group: HR lower Surgical field significantly improved Blood loss lower |
| Dogan et al, 1999 | I, S, P | In vitro effects on platelet aggregation | 30 | P, S: inhibit platelet aggregation. No difference between groups I: no effect |
| Durmus et al, 2007 | Dexmedetomidine (α2-receptor agonist) vs placebo in tympanoplasty and septorhinoplasty | HR, BP Bleeding score (nonvalidated 1–4) | 40 | Dexmedetomidine group: Reduced requirements for anesthetic agents HR, BP lower Surgical field improved |
| Eberhart et al, 2003 | TIVA (P/R) vs I/A | BP, HR Surgical conditions: VAS+Boezaart scale Dryness of field: VAS Blood loss | 90 | BP: NSD TIVA: HR lower Surgical conditions improved Blood loss: NSD |
| Eberhart et al, 2007 | D/R vs R/D: comparison between D-accentuated and R-accentuated anesthesia | Surgical conditions: VAS+Boezaart scale HR, BP, postoperative recovery | 100 | Surgical conditions, HR, BP: NSD Dryness: improved in D-accentuated group Recovery: slightly faster in R-accentuated group, no difference at 1 h after operation Summary: NSD between techniques |
| Elsharnouby and Elsharnouby, 2006 | MgSO 4 vs saline (both groups S/F) | HR, BP Surgical field (Boezaart rating scale) | 60 | MgSO4 group: HR, BP lower Surgical field improved Decreased requirements for F,S Emergence time increased |
| Jacobi et al, 2000 | Normotension vs nitroprusside+captopril induced hypotension | BP Dryness of field ACTH, AVP, cortisol | 32 | Hypotensive group: HR higher BP lower Surgical field: NSD ACTH, AVP, cortisol: NSD |
| Kaygusuz et al, 2008 | D/R vs I/R in tympanoplasty and sinus surgery | HR, BP, blood loss Surgical field: VAS Postoperative recovery | 64 | Blood loss, HR, BP: NSD Recovery: quicker with D |
| Manola et al, 2005 | Sufentanil/S vs TIVA(P/R) vs I/F | BP Surgical field (Boezaart scale) Blood loss | 71 | BP: NSD HR not reported Surgical field significantly better in sufentanil/S and TIVA groups |
| Nair et al, 2004 | Metoprolol vs placebo premedication | HR, BP Surgical field (Boezaart scale) | 80 | HR: lower in metoprolol group Surgical field: NSD between groups correlated with HR Significantly better with HR <60 Not correlated with BP |
| Nekhendzy et al, 2007 | Hypercapnia vs hypocapnia vs normocapnia | Blood loss Surgical field | 180 | Blood loss: NSD Surgical field: NSD Hypocapnia group: higher requirements for antihypertensives Increased blood loss with increased CT score, duration of surgery |
| Okuyama et al, 2005 | Hypotension with prostaglandin E1 (PGE1) and diazepam premedication vs normotension with clonidine premedication vs normotension with diazepam premedication (control group) | BP, HR Blood loss | 24 | PGE1 group: lower BP, higher HR, blood loss NSD from control Clonidine group: BP NSD, HR lower, blood loss lower than control |
| Pavlin et al, 1999 | TIVA (P/A) vs I/A | Blood loss Surgical field Postoperative recovery HR, BP not reported | 56 | Surgical field: better in P group Blood loss: NSD Postoperative recovery: shorter time to discharge in P group |
| Sivaci et al, 2004 | P/F vs S/F | BP, HR Blood loss | 32 | BP, HR: NSD Blood loss: lower in P/F group |
| Tirelli et al, 2004 | TIVA (P/R) vs I/F | BP, HR Surgical field (Boezaart) | 64 | Surgical field: better with TIVA HR, BP: NSD (trend to be lower in TIVA group) |
| Wormald et al, 2005 | TIVA (P/R) vs S/F | BP, HR Surgical field (Boezaart) | 56 | TIVA: Surgical field improved Improved field correlated independently with lower BP and lower HR |
| Wormald et al, 2005 | Pterygopalatine fossa injection vs no injection (compared sides in same patients) | BP, HR, Surgical field (Boezaart) | 55 | Injection: improved surgical field BP, HR: NSD Field correlated independently with HR |
The importance of relative bradycardia is shown in several other studies. A correlation between decreased HR and improved surgical field has been shown. Hypotension achieved with infusion of esmolol (a short acting β-blocker) or magnesium sulfate, or premedication with clonidine or dexmedetomidine (centrally acting α 2 agonists that, acting on the presynaptic α 2 receptor, result in decreased sympathetic tone) result in lower HR and improved surgical field. In contrast, hypotension achieved with the use of vasodilators (nitroprusside or prostaglandin E 1 ) results in reflex tachycardia and no improvement in the surgical field or blood loss (respectively) compared with normotensive anesthesia.
Many anesthetic agents also have effects on platelet function. Of the inhalational anesthetics, isoflurane and desflurane do not seem to affect platelet function, whereas sevoflurane and nitrous oxide seem to inhibit platelet aggregation. Of the intravenous agents, propofol is believed to inhibit platelet aggregation, whereas the opioids do not. A direct comparison of the effects of propofol, isoflurane, and sevoflurane in sinus surgery found propofol to have a larger inhibitory effect than sevoflurane or isoflurane. However, the clinical significance seems to be minimal in the operative setting.
In summary, the optimal anesthetic technique seems to be relative bradycardia with associated hypotension. All groups in which these conditions were met showed benefit, whereas no group with an increased HR had improved field or blood loss.
Patient positioning
The reverse Trendelenberg position is used to reduce venous pressure and thus improve bleeding ( Fig. 1 ). Between 5° and 15° of reverse Trendelenberg tilt is sufficient to reduce central venous pressure from an average of 9.2 mm Hg to 1.7 mm Hg. At 25° of reverse Trendelenberg tilt, the mean pressure in the confluums sinuum is zero. Cerebral perfusion pressure is the difference between mean arterial pressure (MAP) and intracranial pressure (ICP). Positional decreases in MAP are offset by decreased ICP, probably due to increased venous outflow and hydrostatic displacement of cerebrospinal fluid (CSF), therefore cerebral perfusion and blood flow are preserved up to 20 to 30° of tilt.
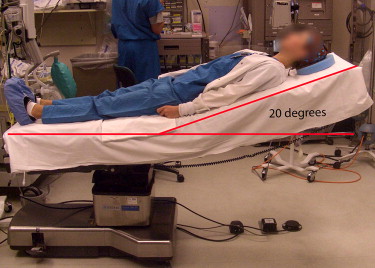
Position also affects mucosal blood flow. Gurr and colleagues showed a 38% decrease in blood flow to the head of the inferior turbinate with 20° of reverse Trendelenberg tilt with a corresponding increase in blood flow in the head-down position. Ko and colleagues found an improvement in blood loss and surgical field in ESS with 10° of reverse Trendelenberg tilt compared with patients laid supine.
Topical vasoconstriction
A variety of topical agents have been used alone or in combinations. Adrenalin causes a dose-dependent response at α 1 and α 2 receptors, resulting in vasoconstriction of arterial and capacitance vessels. Topical use in up to 1:1000 concentration has been widely used without evidence of systemic hemodynamic response. Cocaine blocks the reuptake of noradrenalin at the nerve ending, resulting in a vasoconstrictive effect in addition to its local anesthetic properties. However, it has not been shown to be superior to other agents and has been associated with dose-related and idiosyncratic reactions including cardiac arrhythmias and death. Oxymetazoline and phenylephrine are partial α agonists, with predominantly α 1 effects. They therefore have limited effect on the capacitance vessels and are likely to be less effective in hemostasis. Theoretically, the use of one of these partial agonists may result in competitive inhibition with adrenalin, reducing its effect. For these reasons, the authors’ preference is to use adrenalin alone as a topical nasal preparation.
Local infiltration
Infiltration of the nasal mucosa, commonly with adrenalin containing local anesthetics, has complex hemodynamic effects. There is a hypotensive response to injection of low doses of adrenalin, probably due to activation of high-sensitivity β 2 receptors in skeletal muscle, causing vasodilation. At higher doses, increasing vasoconstriction in skin, mucosa, and kidney, as well as activation of cardiac β 1 receptors, results in increased BP. Lignocaine also has a hypotensive effect, and the relative influences of adrenalin and lignocaine infiltration are difficult to separate in the current literature Cohen-Kerem and colleagues compared saline with lignocaine/adrenalin injection. There was an improved surgical field and lower requirement for topical adrenalin in the lignocaine/adrenalin group. There was a hypotensive response to the lignocaine/adrenalin injection, and a tachycardic response to the saline injection. Increased MAP was correlated with plasma noradrenalin levels, which were lower in the lignocaine/adrenalin group. These findings were believed to be to the result of decreased sympathetic stimulation (less pain) in the lignocaine/adrenalin group.
Infiltration of the pterygopalatine fossa (PPF) via the greater palatine canal has been proposed to reduce blood flow to the nasal cavity by inducing vasoconstriction or compression of the terminal branches of the maxillary artery. PPF injection with lignocaine/adrenalin has been shown to improve the surgical field in sinus surgery. Other clinical studies have shown PPF injection to be effective in posterior epistaxis with plain xylocaine, water, or glycerine, presumably on the basis of physical compression of the artery. PPF injection may have limited effect in the anterior nose. Laser Doppler studies have shown only a 4% reduction in blood flow to the head of the inferior turbinate following PPF injection with bupivicaine.
Irrigation
Warm-water irrigation has been advocated for hemostasis in nasal mucosa, and warm saline is used in some skull base centers to control diffuse bleeding. We use copious irrigation at room temperature, which not only removes excess blood but also seems to have a hemostatic effect.
Hemostatic materials
A wide variety of hemostatic materials are available to provide intraoperative and postoperative hemostasis ( Table 7 ). In general, it seems that microfibrillar collagen, FloSeal, poly- N -acetylglucosamines, and fibrin glues are more effective than Surgicel or gelfoam in hemostasis. The main drawbacks of these agents are the potential for postoperative granulation and adhesion formation (see Table 7 ); however, not all have been studied in the nose and, of the studies available, many are small or uncontrolled. The use of human blood products such as thrombin and fibrinogen raises the possibility of transmission of viral diseases, whereas the use of bovine thrombin is associated with a high rate of antibody development, with reports of anaphylaxis and coagulopathy.



