Pattern Scan Laser (PASCAL) Photocoagulation
Raul Velez-Montoya
Gerardo García-Aguirre
Mark Blumenkranz
Hugo Quiroz-Mercado
INTRODUCTION
Thirty years ago, in the 1970s, the Diabetic Retinopathy Study (DRS) established the foundation of modern panretinal photocoagulation (PRP). The study results demonstrated a benefit from the application of laser photocoagulation to the retina by reducing the risk of severe visual loss in patients with proliferative diabetic retinopathy (PDR) by 50% (1). Later, the Early Treatment Diabetic Retinopathy Study (ETDRS) likewise showed similar results by decreasing the risk of moderate visual loss in patients with nonproliferative diabetic retinopathy from 16.3% to 6.4%, and up to 50% in patients with diabetic macular edema (2). Since then, the treatment of the retina with laser photocoagulation has become a fundamental part of the everyday medical practice for ophthalmologists and is the treatment of choice for ischemic and neovascular diseases (1, 2, 3 and 4).
Panretinal, direct focal, and macular grid photocoagulation have been the leading techniques of laser treatment to the retina for nearly 40 years. In ischemic diseases, patients usually receive 1200 to 1800 laser burns, divided into two to four sessions, each one separated at intervals of 2 to 4 weeks and with each session lasting 10 to 15 minutes. This treatment scheme has remained virtually unchanged for over 20 years (5, 6 and 7).
Since solar and xenon arc lamp photocoagulation were introduced in the late 1950s by Meyer-Schwickerath as a therapeutic method in ophthalmology, the indications for their use as well as the equipment used for their administration have evolved. The first device, successfully used in clinical practice, was the xenon arc lamp (8). This light source had the disadvantage of being composed of a polychromatic wavelength. This made it very inefficient in terms of the amount of energy absorbed by the tissue, and unpredictable in terms of tissue interaction. With the next generation of laser photocoagulators, more efficient equipment appeared, providing monochromatic wavelength (e.g., the ruby, argon, and krypton laser). Since then, advances in technology have focused on designing devices more convenient for the physician than for the patient. The emergence of systems with air-cooling modules and the advent of fiber optic allowed companies to significantly reduce the size of the equipment. However, despite the fact that today we have more compact and efficient solid-state lasers, the way in which the treatment is administered remains unchanged since the mid-1970s (8). In short, the procedure is tedious for the patient and physician and varies between uncomfortable and painful for the patient, occasionally requiring the administration of retrobulbar anesthetic injections.
LASER MECHANISM OF ACTION
The mechanism through which the laser exerts its therapeutic action is still undetermined. When photocoagulation was applied for the first time in PDR, it was thought that the mechanism of action was the photocoagulation and destruction of areas of neovascularization, thus preventing vitreous hemorrhage and tractional retinal detachment. In later observations, it was clear that the clinical effect of photocoagulation seemed to depend more on applying laser to healthy retina than to areas of neovascularization (9).
The first theory about the effectiveness of laser was based on the initial observation by Michaelson, in which he proposed the existence of a “growth factor X,” responsible for neovascularization of the hypoxic retina (10). Patz et al. took up this idea and suggested that the therapeutic effect of laser was exercised by destroying sick and hypoxic tissue. In such a way, the source of production of the “factor X” was destroyed and hence its intraocular levels were lowered. The problem with this theory was, in the case of PDR, that hypoxia is located in the inner retinal layers, being primarily a problem of microangiopathy and occlusion of the microcirculation, while the outer retinal layers remain apparently normal. Histological evidence demonstrated that mild to moderate laser burns destroy the outer layers and the retinal pigment epithelium (RPE), leaving the inner layers intact, which was the alleged source of the “growth factor X” (9,10).
Another theory, based on histological observations, stated that laser destruction of RPE cells produces the release of protective factors that slows the process of neovascularization. This theory was reinforced by Mori et al., who demonstrated the protection that a platelet-derived factor produced on delaying neovascularization of the retina and choroid. However, a direct relationship between the application of laser and the release of these factors has never been proven conclusively (9,11).
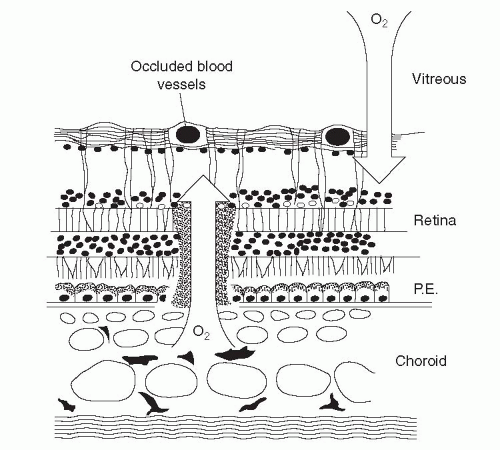
The oxygen theory suggested that photocoagulation destroys the photoreceptors, decreasing oxygen demands of the outer retina and improving oxygenation of the inner layers. This, in turn, decreases the production of growth factors and alters retinal hemodynamics. The acceptance of this theory is based in the fact that it explains the effect of laser not only in proliferative diseases but also on macular edema (9,12).
Under normal circumstances, oxygen and nutrients diffuse through the choriocapillaris to the retina to be consumed by photoreceptors, which have a high number of mitochondria and hence a high level of oxygen consumption. After a laser burn, the photoreceptor layer is replaced by glial tissue. This tissue then has fewer mitochondria and therefore lowers the overall oxygen demand (9,12). This means that laser injuries serve as “windows” in the outer retina, where oxygen consumption is low and may spread further to the inner retina, increasing the oxygen tension in this space (Fig. 11-1). Besides lowering the total consumption of oxygen, laser photocoagulation also decreases the production of growth factors (e.g., vascular endothelial growth factor [VEGF]) by destroying hypoxic tissue. Aiello et al. and Agustin et al. published that levels of VEGF were significantly elevated in the vitreous of patients with PDR and that these decreased significantly after laser treatment (13).
An important proof that laser treatment improves the effects of hypoxia in the retina is the observed changes in the vascular diameter. Under conditions of low oxygen tension, the arterioles are dilated, which increases local blood flow and thus the hydrostatic pressure within capillaries. When oxygen levels return to normal, the arterioles contract. This in turn decreases the blood flow and the hydrostatic pressure. In the ETDRS, fundus photographs were taken of all patients before and after the laser treatment. The analysis of this material
proved that blood vessel caliber decreased 10% to 15% after laser treatment with xenon arc or argon laser photocoagulation (9,14).
proved that blood vessel caliber decreased 10% to 15% after laser treatment with xenon arc or argon laser photocoagulation (9,14).
 Get Clinical Tree app for offline access 
|


