, Rudolf Leuwer2, Konrad Schwager3 and Sören Wenzel4
(1)
Otology and Neurotology Division, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA
(2)
Otorhinolaryngology Head and Neck Surgery, HELIOS Hospital, Krefeld, Germany
(3)
Otorhinolaryngology Head and Neck Surgery, Klinikum Fulda, Fulda, Germany
(4)
Otorhinolaryngology Head and Neck Surgery, Pinneberg, Germany
Eustachian tube closing failure
Sniffing
Aetiology: loss of Ostmann’s fat pad, scars and hormonal factors
Therapy: medical and injection therapy and surgical methods
Dynamic stabilization by physiotherapy
3.1 Definition
The impairment of the physiological protection function of the Eustachian tube causes a distressing autophony and aural fullness, the so-called syndrome of the patulous Eustachian tube (pET) [13, 74, 130]. The pET as it is described here to a certain extent is just the “tip of the iceberg” in the general complex of Eustachian tube closing failure [108].
The Eustachian tube is closed at rest and is actively opened only under controlled conditions during respiratory rest in the nasopharynx. If the Eustachian tube is opened outside this limited range of time, there is a pathological communication between the nasopharynx and the tympanic cavity. This pathological communication causes an intermittent or constant transfer of pressure fluctuations from the pharynx towards the middle ear. Not only aural fullness and autophony, but also inner ear phenomena, such as sensorineural hearing loss and tinnitus or vertigo, and grave mental disorders are described as a result of a pET [62, 150].
The intensity and frequency of complaints vary inter- and intraindividually. In cases of rare symptoms or of low-intensity symptoms, it is enough to inform the patient of the diagnosis and of the harmlessness of the symptoms. On the other hand, there are patients who are so distressed by pET symptoms, that psychological problems arise, resulting in the inability to work or suicidal tendencies. These patients need an ENT specialist for the initiation of specific diagnostics and therapy.
The incidence of the pET is approximately 7 % [123]. Many of these patients can modify their symptoms by increasing the venous pressure of the mucosal vessels and the surrounding venous plexus of the Eustachian tube by compression of the jugular veins or by an inclined head position. In many cases “sniffing” is a useful manoeuvre to actively release the distressing symptoms. During sniffing the Eustachian tube and the middle ear are evacuated by a forced nasal inspiration, causing stiffening of the eardrum and the ossicular chain. This effect is temporary, and sniffing will be repeatedly used. The risk of a long-term sniffing habit is to produce a chronic negative middle ear pressure and the development of middle ear diseases [60, 84, 108]. On the other hand, the reduction of the intrathoracic pressure during sniffing causes a lower pressure of the cervical vein and, subsequently, of the peritubal veins and thus may even enhance the symptoms [106].
Usually the pET does not lead to a chronic middle ear inflammation because the negative pressure in the tympanic cavity is not prolonged.
3.2 Established Aetiological Factors and Therapeutic Procedures
The following factors are generally accepted as the main aetiological causes of the pET:
The reduction of the Ostmann’s fat pad during intended or compulsory weight reduction [79] is considered to be one of the main factors [151] causing the symptoms of a pET. Takasaki et al. [194] observed a pET in a patient with an oropharyngeal carcinoma who developed a loss of Ostmann’s fat pad during recurrence and cachexia. The autopsy showed a complete loss of the fat pad, resulting in a direct contact between the tensor veli palatini muscle and the lumen of the Eustachian tube. Using MRI Pahnke et al. [137] showed a reduction of the Ostmann’s fat pad in 7 of 10 patients with the symptoms of a pET.
Modifications of the nasopharyngeal anatomy by surgical procedures, such as adenoidectomy or tonsillectomy with postoperative scarring, can also be a cause of a pET [150]. Likewise, scarring after irradiation of the cranium can also result in a closing failure of the Eustachian tube, which can be shown using tubal manometry in about 50 % of the patients [22]. After a retrospective analysis of 16 patients with a pET, Todd and Saunders [199] postulated a correlation between the frequency of chronic suppurative otitis media during childhood and the occurrence of a pET in adults. The authors maintained that this was due to a loss of turgor and elasticity of the “tubal tissue” and a change of the surface tension of the tubal mucosa due to middle ear inflammations.
The compliance of the Eustachian tube can be affected by oestrogen [3, 25]. Miller [117] documented 17 female patients in 12 years who during pregnancy developed symptoms of a pET. The largest series of patients was published by Plate et al. [141] who examined 270 pregnant women. Of these, 19 appeared to have a closing failure of the Eustachian tube but only 5 showed the clinical symptoms of a pET. The symptoms were highly correlated to the level of oestriol in the serum. Oestrogen is supposed to have an impact upon the viscosity of the intratubal mucus [44] as well as on the compliance of the tubal cartilage [141]. In addition, increased oestrogen causes increased fat metabolism leading to a reduction of the Ostmann’s fat pad [188].
One neuromuscular factor is a disorder of the controlled tubal opening during respiratory rest in the nasopharynx, with a delayed closing and the consequence of a relative closing failure [89]. In addition, pathological changes of the central and peripheral nervous system must be considered, such as trauma or neurological system diseases, such as multiple sclerosis, Parkinson’s disease or poliomyelitis [149].
The range of the aetiological spectrum of a pET explains the multitude of interventions suggested in order to treat the symptoms. That is why there is not an accepted standard of therapy. Neither oedema-inducing drugs [130], paratubal injections at the pharyngeal orifice [148], ventilation tubes in the ear drum [102], surgical manipulations on the tensor veli palatini muscle [206], nor a complete obstruction of the Eustachian tube [13, 31] could show more than temporary effects on the symptoms. The latter two, on the other hand, can have an impact upon the opening function of the Eustachian tube and must be regarded very critically concerning the development of chronic middle ear disease [15, 92, 167, 198].
3.3 Diagnosis
There are usually no clinical signs of a pET. In many cases the tympanic membrane and the middle ear seem normal on ear microscopy. That is why the diagnosis is confirmed by taking the exact medical history. The description of intermittent as well as permanent symptoms is as important as the past history of weight loss, pregnancy and oral contraceptives. The history should include any surgery on the tonsils and adenoids, neuromuscular diseases and, especially, temporomandibular joint disorders. Some patients complain of a pET after otitis media. If the symptoms are present on examination, they can be relieved by compression of the jugular vein. Sometimes medial and lateral movements of the tympanic membrane are visible and can be confirmed when using tympanometry. Other classical functional tests can support these findings [41, 75, 81, 124, 125]. The pressure chamber investigation does not have relevance for clinical practice due to its immense technical expenditure. MRI or CT can help confirm morphological changes of the paratubal structures but does not replace thorough clinical observation (Fig. 3.1).
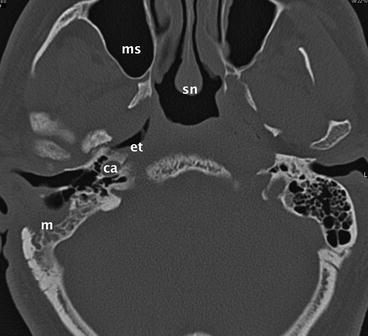
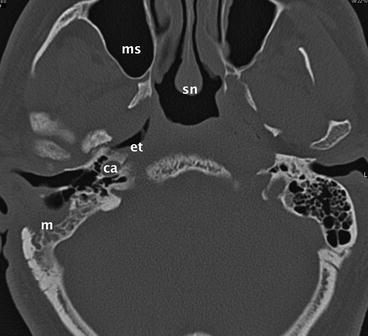
Fig. 3.1
Axial CT of the Eustachian tube with a patient suffering from a pET. He underwent several middle ear operations. m mastoid, ca carotid artery, et Eustachian tube, ms maxillary sinus, sn nasal septum
3.4 Therapy
Generally, the pET does not cause structural changes in the tympanic cavity, which thus could require a tympanoplasty. Hence, the middle ear-associated symptoms should primarily be treated on the level of the Eustachian tube. However, if a pronounced atrophy of the eardrum and a pET are present, tympanoplasty could be reasonable and should be performed using cartilage as a graft.
In cases of an oestrogen-induced pET, the cessation of hormonal contraception and other methods of birth control should be considered. Also inflammations of the upper aero-digestive tract, arterial hypotonia as well as a gastro-oesophageal reflux should be treated.
Moisturizing nasal sprays may have a supportive character in cases of a dry nasal mucosa; a sufficient therapy of the pET cannot be expected.
Oshima et al. [133] instructed their 59 patients to self-administer physiological saline solution into their noses. Their single dose was about 1 ml. The patients used the drops in a sitting position with their neck bent posteriorly. The outcome was measured after several weeks of self-therapy. They could show that this simple treatment could clinically relieve the symptoms of the pET with more than 60 % of their patients. Subsequently, they recommend this instillation treatment as an initial therapy for a pET.
Bartlett and colleagues [10] suggested loading the tympanic membrane with a putty-like substance, called Blu-Tack. Blu-Tack is a pale-blue pressure-sensitive adhesive that is produced to attach posters or sheets of paper to dry surfaces. It is a synthetic non-toxic rubber compound. They reported a temporary relief of the symptoms with 14 patients suffering from a pET.
3.4.1 Conservative Treatment
Most nonsurgical suggestions for the treatment of a pET aim at the obstruction of the pharyngeal orifice. Different authors described the local induction of a mucosal oedema by the transnasal administration of powdered boric acid, salicylic acid, trichloroacetic acid, nitric acid, phenol or silver nitrate [130, 131]. A temporary success was reported for intranasal treatment with diluted hydrochloric acid, benzyl alcohol and chlorobutanol [28], with conjugated oestrogen [31], with atropine [122] and with the oral application of potassium iodide solution [37]. The authors did not explain the mechanism of the latter medication.
An obvious consequence of the great number of patients presenting with a pronounced loss of weight within a short period of time is to suggest a “therapeutic” gain of weight first. Yet Pahnke et al. [137] could not show a positive effect after a significant increase of body weight in seven affected patients. They explained this observation by the anatomical structure of the Ostmann’s fat pad: the Ostmann’s fat pad is separated by strong connective tissue connecting the medial fascia of the tensor muscle and the membranous lateral Eustachian tube wall (paries membranaceus) [111, 216]. During the loss of weight, the fat and the connective tissue are affected and shrink. This process to a certain point seems to be irreversible, preventing the Ostmann’s fatty tissue from regrowing once the body weight has recovered [137].
3.4.2 Injection Therapy
A therapy frequently suggested is the augmentation of the nasopharyngeal orifice of the Eustachian tube. The success rate of the augmentation therapy depends on the long-term stability rather than the quantity of the injected substance. Pulec [148] used polytetrafluoroethylene paste (Teflon®). He injected this substance into the anterior–inferior margin of the nasopharyngeal Eustachian tube orifice and observed an improvement of the pET symptoms in 73 % (19 of 26 patients) within a 3-year follow-up. According to the author, the tissue compatibility of Teflon® is good. Officially, injection of Teflon® paste anterior to the mouth of the Eustachian tube has been stopped by the manufacturer of the paste because of serious complications caused by the Teflon paste being accidentally injected into the internal carotid artery [130]. Figure 3.2 shows an MRI of a young adult German patient treated by Pulec himself in the 1990s.
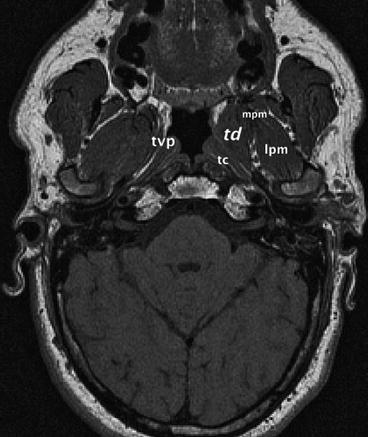
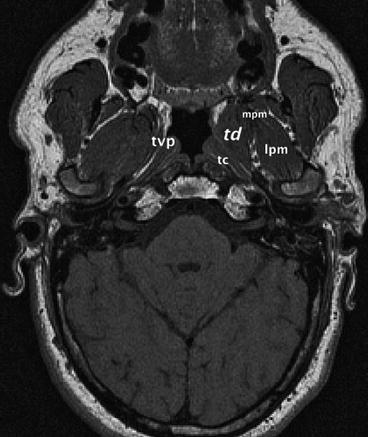
Fig. 3.2
Axial MRI study of a patient with pET after (successful) injection of Teflon® paste in the paratubal space. mpm medial pterygoid muscle, lpm lateral pterygoid muscle, tvp tensor veli palatini muscle, tc tubal cartilage, td Teflon depot
Other materials have been used for augmentation and/or obstruction, such as autologous fat, collagen and even silicone. Surprisingly there are no long-term results published. Kong et al. [85] injected paste-like minced autologous tragal cartilage submucosally into the pharyngeal orifice of the Eustachian tubes of two patients. Both patients remained free of symptoms for 18 and 24 months, respectively, after the procedure.
3.4.3 Surgical Therapy
The insertion of grommets into the tympanic membrane is the most frequently suggested procedure for pET [102]. The success rates are up to 50 % or higher [21, 150]. Seventy percent of these patients had breath-synchronous, tympanometric eardrum movements preoperatively. The insertion of grommets has no significant effect upon the annoying symptom of autophony. The tympanic ventilation shunt is only able to absorb the pressure changes in the tympanic cavity, which are due to swallowing and breathing. The transtubal sound transmission caused by the impaired protection function is not influenced. The uncertain and incomplete effect of grommets is additionally restricted by local side effects of the tympanostomy tubes, such as otorrhea.
Virtanen [205] suggested increasing the paratubal pressure by ligature of the internal jugular vein. Unfortunately, there are no published data on the long-term effect of this therapy. Due to the adaptability of the venous drainage, the intended increase of the paratubal pressure is temporary.
Surgical obstruction of the Eustachian tube can be performed in the nasopharyngeal or the tympanic orifice. By means of a urologic diathermy probe, Robinson and Hazell [157] could achieve a complete or partial removal of pET complaints in 9 of 13 patients. Data concerning the long-term effect (more than 3 months) are missing in the publications.
Poe [143] demonstrated a method of surgical augmentation of the nasopharyngeal orifice using autologous cartilage, an alloderm implant or calcium hydroxyapatite. He used a transnasal/transoral approach and inserted the graft under endoscopic control anterolateral to the tubal lumen. His success rates (six patients satisfied, eight patients dissatisfied) and the absence of surgical and physiological complications make it reasonable to think about a modification of this interesting technique (see below).
Yanez et al. [213] recently reported a laser-assisted curvature inversion technique of the medial and lateral lamina of the Eustachian tube cartilage. A Potassium-titanyl phosphate laser is used as a cutting tool. It is applied transorally and transnasally, respectively, using a fibre-optic tool. A cross-hatching cutting technique alters the tension of the cartilage of the pharyngeal orifice. The authors treated 11 patients and, according to their publication, they achieved a complete long-term relief of symptoms in more than 70 % of the cases.
In cases of a persistent pET after conservative therapy the authors use septal cartilage for the augmentation of the nasopharyngeal orifice. Harvested nasal septum cartilage splints measuring about 2.5 × 1 cm are implanted between the tensor veli palatini muscle and the Eustachian tube under full anaesthesia (Fig. 3.3a, b). For implantation a transpalatinal approach is used, which is controlled by nasal endoscopy. A navigation system can help to avoid misplacement (Fig. 3.4). Once the bed for the cartilage is formed by a scissor, the splint is pushed upward as far as possible (Fig. 3.5). Due to the good results of the physiotherapy, only seven patients have been treated using this augmentation method. One patient had no effect of the treatment between 6 and 12 months after surgery, two patients described a moderate relief, and four patients a marked relief of their symptoms. There were no surgery-associated septal or middle ear complications in this group; no patient reported sensations of a pharyngeal foreign body.
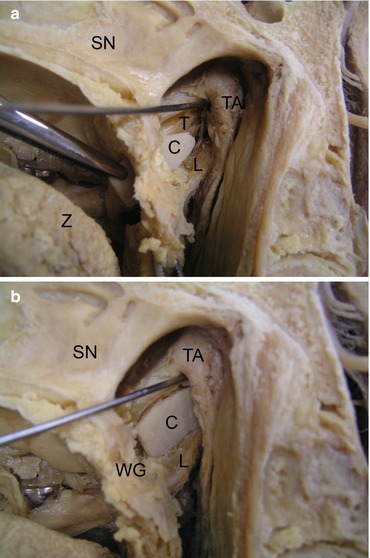
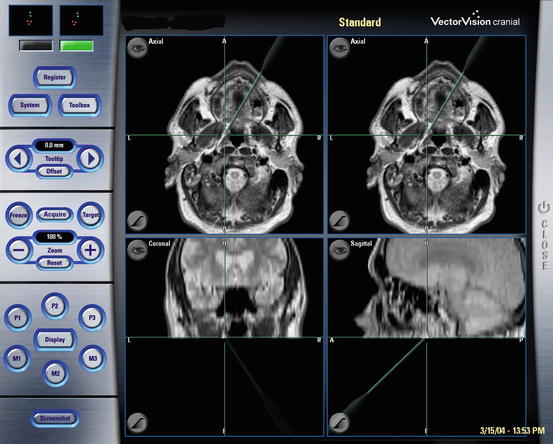
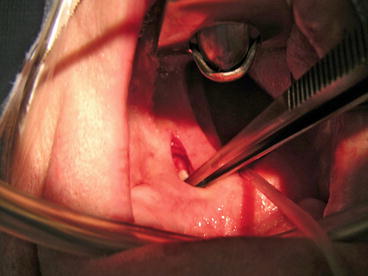
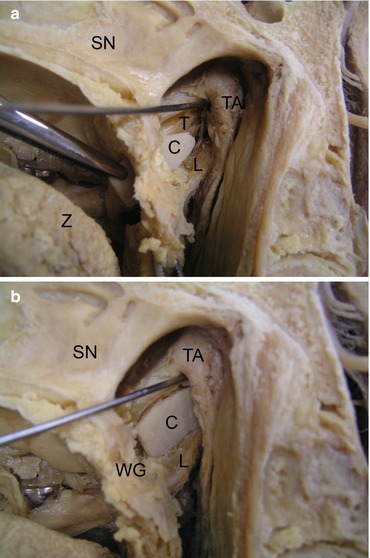
Fig. 3.3
(a) Transpalatinal paratubal implantation of septal cartilage. The testing probe is in the lumen of the Eustachian tube. SN nasal septum, Z tongue, C cartilage, T tensor veli palatini muscle, L levator veli palatini muscle, TA tubal cartilage. (b) Septal cartilage in final position. SN nasal septum, C cartilage, L levator veli palatini muscle, TA tubal cartilage, WG soft palate
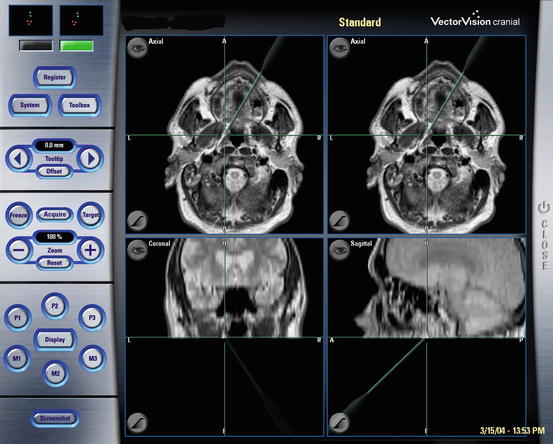
Fig. 3.4
Control of the position of the septal cartilage using 3D-MRI-navigation
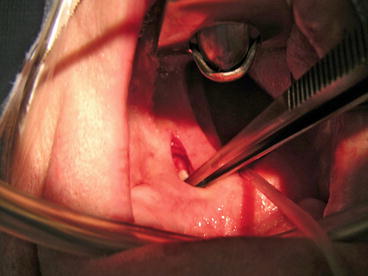
Fig. 3.5
Intraoperative situation: transpalatinal approach and velotraction for endoscopic control of the nasopharynx
There are a lot of advantages of this method:
Nasal septum cartilage is a stable material that is easy to harvest.
The direct transpalatinal implantation approach can be easily controlled by telescope.
The tensor veli palatini muscle is a safe landmark for placement of the cartilage.
The procedure is reversible.
Doherty and Slattery [31] could eliminate autophony and aural fullness successfully in two cases by cauterization and autologous fat graft plugging of the Eustachian tube at its nasopharyngeal orifice, in conjunction with myringotomy and ventilation tube placement.
The transtympanal obstruction of the Eustachian tube was demonstrated by Bluestone and Cantekin [13] and by Dyer and McElveen [37]. They inserted a soft catheter into the tympanal orifice and fixed it with bone wax. These patients also received tympanostomy tubes for ventilation. The advantage of this method is its reversibility. Unfortunately, exact numbers of patients successfully treated are unknown.
Another technical approach is to impair the opening force of the tensor veli palatini muscle, either by resection or by toxic inhibition [120, 187, 206]. Stroud et al. [187] cut off the tensor’s tendon in 10 patients with pET, with a reported success rate of 90 % (9 of 10 patients). Virtanen and Palva [206] extended the concept by the fracture or resection of the pterygoid hamulus. According to the authors, 9 of 13 patients remained without pET complaints up to 60 months. Despite the high success rates and the small rate of surgery-related complications, both procedures cannot be generally accepted in the therapy of the pET. Factures of the hamulus and surgical manipulations at the tensor veli palatini muscle are known as the substantial causes of chronic middle ear inflammations after cleft palate closure [14, 91, 158, 181]. The tensor not only opens the Eustachian tube, but it also is the physiological basis for active drainage of the middle ear [169]. A passive Eustachian tube without active muscular coordination should be absolutely avoided.
3.4.4 The “Dynamic Stabilization”
Despite the multitude of recommendations for the therapy of a pET, there still is no standard approach for these patients. All the studies published on the topic deal with a small number of patients. In addition, there is more than one pathophysiological mechanism responsible for the individual pET. Moreover, many of the components of the Eustachian tube playing a role in pET, such as the ingredients of the mucus, remain unknown. On the other hand, due to the differential specificity of the pathology, many cases of pET remain undetected. Many of the procedures described above are accompanied by their own Eustachian tube pathology. That is why it is justified to look for a completely non-invasive approach for correcting the pET. The aim of this approach should be to reduce the symptoms of the pET and to keep the intrinsic Eustachian tube function.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


