Chapter 23 Partial Stapedectomy
HISTORY
In 1958, Shea1 advocated total stapes footplate removal when using the polyethylene strut prosthesis and a vein graft to seal the oval window. Shortly thereafter, Schuknecht2 advocated the use of a wire and fat prosthesis, and House and Greenfield3 later advocated the use of a wire with absorbable gelatin sponge (Gelfoam) prosthesis. The use of the wire/Gelfoam or wire/fat prosthesis necessitated total removal of the footplate for the wire prosthesis to function satisfactorily. Other methods that could be considered a partial stapedectomy technique included the shattered footplate procedure with the use of a polyethylene strut, and the subluxated footplate procedure, both of which necessitated removal of the superstructure of the stapes.4 These two techniques were quickly rejected because of the associated sensorineural hearing loss resulting from either surgical trauma or a perilymphatic fistula.
In 1961, the piston concept was introduced, in which a cup/piston prosthesis was used with a connective tissue graft of vein to seal the oval window.5 The introduction of the piston prosthesis no longer required a total removal of the stapes footplate. The concept evolved of “removing only that part of the footplate which comes out easily.”6 This newly introduced surgical technique consequently produced more successful hearing results and fewer inner ear complications. The same technique could be used for the thin blue footplate with minimal otosclerotic involvement, or for the obliterative footplate, in which only a stapedotomy opening (“drill-out”) could be created. Measurement of the distance between the long process of the incus and stapes footplate was eliminated because a 4-mm prosthesis would protrude into the vestibule 0.2 to 0.3 mm in virtually every case. This slight protrusion would create its self-centering effect. By interposing a vein graft between the prosthesis and vestibule, there was rarely a regrowth of otosclerotic bone, including the obliterative type. Also, because of this protrusion, migration of the piston in subsequent years was virtually unknown.
The 4 mm length is used in virtually every stapedectomy case whether it is a drill-out stapedotomy, a partial footplate removal, or a total footplate removal. Any connective tissue can be used with this prosthesis, but I prefer a vein graft that outlines the oval window opening and ensures a complete immediate seal of the oval window. Moon7 advocates the cup/piston prosthesis with areolar tissue. The cup/piston prosthesis is radiopaque and easy to localize and identify on routine mastoid radiographic views. Comparison of impedance studies of various stapes prostheses has shown the stainless steel cup/piston to be the closest in compliance to that of a normal mobile stapes.8 Hearing results reported by otologic surgeons who have used this technique have consistently confirmed a 96% air-bone gap closure to within 10 dB.9–11 Similarly, the complete closure (and overclosure) rate has been repeatedly confirmed at 80%, which the wire/tissue prosthesis and wire pistons have yet to attain.
Because the stapes does not increase in size with age, the 4 mm cup/piston prosthesis has been used in children 5 years old, adults, and elderly individuals. All patients who show an air-bone gap and normal results on otologic examination are candidates for stapedectomy surgery if stapedial fixation is found at the time of the middle ear exploration. Approximately 22% of patients with otosclerosis have a diminished cochlear reserve with a Shambaugh preoperative bone conduction classification of D or E. These patients have very severe mixed hearing losses, and in many, only a partial footplate removal can be obtained. These patients also most frequently show complete closure and overclosure of the air-bone gap. For these patients, the extra 10 dB of hearing gain is crucial because of their mixed hearing loss. Approximately 74% of the patients undergoing surgery have partial or total footplate removal that does not necessitate drilling. The remaining 26% require drilling to create a fenestra 0.8 mm in diameter or larger to accept the vein graft and cup/piston prosthesis.6
In 1980, Austin12 compared the results of total stapedectomy and partial stapedectomy, tissue seal and no tissue seal, and the small fenestra of Smyth. His statistical analysis, using chi-square tables for success or failure, sensorineural hearing loss, fistula, and complete air-bone gap closure, was computed. He concluded that a tissue seal provides a better success rate, a significantly lower risk of fistula, and a better hearing result in terms of complete closure or overclosure of the air-bone gap. Austin noted that in addition to the increased risk of sensorineural complications and fistulas, the small-diameter pistons used in stapedotomies did not provide as good a hearing result.
SURGICAL TECHNIQUE
Stapedectomy footplate surgery follows a very basic principle—be as atraumatic as possible in removing the footplate of the stapes. This principle is contingent on removal of “only that part of the footplate which comes out easily.”6
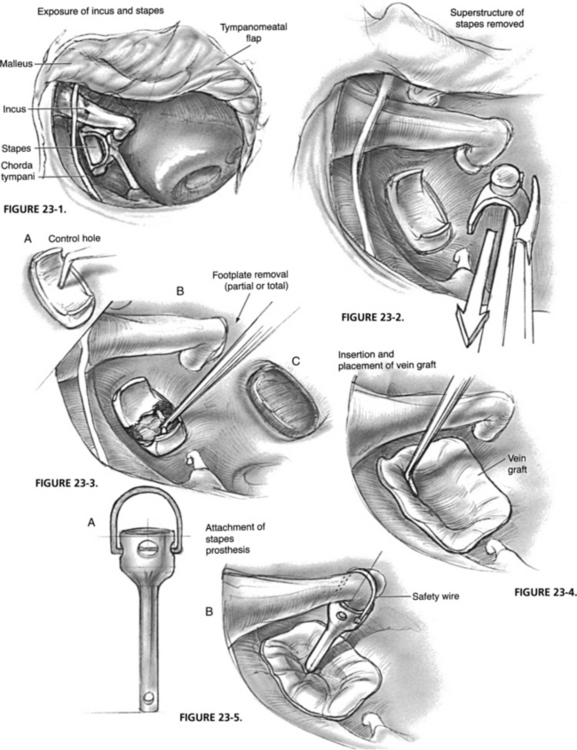
Routine stapedectomy is divided into three stages: (1) exposure of the middle ear, incus, stapes, and footplate area; (2) removal of the stapes superstructure; and (3) removal of the stapes footplate. If the opening is 0.8 mm or larger, the piston can function satisfactorily. The new fenestra must be sealed with a tissue graft; a self-centering 4 mm cup/piston bridges the gap from the oval window membrane to the incus (Figs. 23-1 to 23-5).
Footplate surgery can be classified as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree