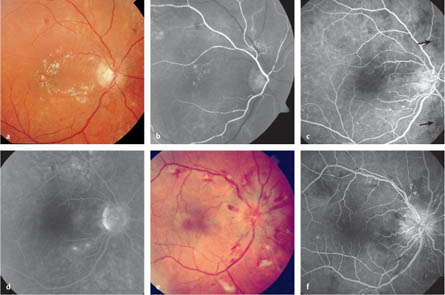
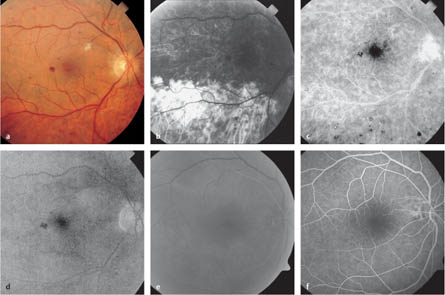
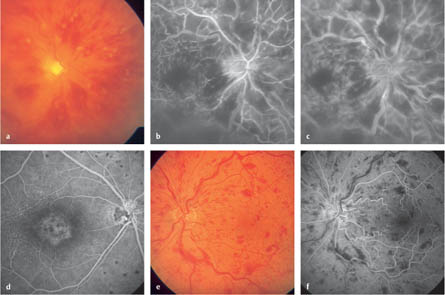
7.1 Hypertensive Retinopathy Duncan BB, Wong TY, Tyroler HA, Davis CE, Fuchs FD. Hypertensive retinopathy and incident coronary heart disease in high risk men. Br J Ophthalmol 2002;86:1002–6. Hayreh SS. Classification of hypertensive fundus changes and their order of appearance. Ophthalmologica 1989;198:247–60. Klein R, Klein BE, Moss SE. The relation of systemic hypertension to changes in the retinal vasculature: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc 1997;95:329–50. Lafaut BA, De Vriese AS, Stulting AA. Fundus fluorescein angiography of patients with severe hypertensive nephropathy. Graefes Arch Clin Exp Ophthalmol 1997;235:749–54. Pache M, Kube T, Wolf S, Kutschbach P. Do angiographic data support a detailed classification of hypertensive fundus changes? J Hum Hypertens 2002;16:405–10. Fig. 7.1a–f Hypertensive retinopathy a Color photograph. Star-shaped hard exudates are seen in the macula, as well as stenotic retinal arteries with thickened vessel walls, signs of arteriovenous crossing and collateral vessels, particularly below and above the optic nerve head. b Arterial phase. Choroidal filling is delayed and segmented. The retinal arterioles show wall irregularities and are clearly constricted. Collateral vessels are visible above the optic nerve head. The hard exudates are sometimes not visible on fluorescence angiography and are only discernible as weak areas of hypofluorescence in the early phase. They cease to be visible during the course of the angiography. c Arteriovenous phase. Collateral vessels can be seen above the optic nerve head, as abnormally directed vessel channels with only minimal leakage. Areas of hypofluorescence secondary to capillary occlusion (arrows) can be seen distal to the collateral vessels. Mild hypofluorescence due to the central retinal edema is visible in the fovea. The choroid still shows segmental, incomplete filling. d Late phase. Two small vessel proliferations in the temporal lower vessel arcade can be identified due to preretinal leakage. The vascular anomalies close to the optic nerve head do not present a similar leakage phenomena in the late phase. Low-grade hyper-fluorescence of the optic nerve head is visible. e Color photograph. Hypertensive retinopathy, with narrowing of the retinal arteries, increased wall reflexes, arteriovenous crossing signs, cotton-wool spots, striped hemorrhage, and optic disc swelling. f Arteriovenous phase. The cotton-wool spots are recognizable as discrete areas of hypofluorescence. Marked congestion and collateral hyperfluorescences can be seen on the optic disc. Speckled and delayed choroidal filling, capillary dropout and adjacent formation of collateral vessels above and below the optic disc, as well as in the temporal vessel arcade area, can be seen. The hemorrhage continues to be visible as constant, clear, and limited areas of hypofluorescence during the course of the angiography. Biousse V. Carotid disease and the eye. Curr Opin Ophthalmol 1997;8:16–26. Brown GC, Magargal LE. The ocular ischemic syndrome: clinical, fluorescein angiographic and carotid angiographic features. Int Ophthalmol 1988;11:239–51. Dugan JD Jr, Green WR. Ophthalmologic manifestations of carotid occlusive disease. Eye 1991;5:226–38. Mizener JB, Podhajsky P, Hayreh SS. Ocular ischemic syndrome. Ophthalmology 1997;104:859–64. Fig. 7.2a–f Ocular ischemic syndrome a Color photograph. Ocular ischemic syndrome in a patient with advanced carotid artery occlusion. The 58-year-old patient presented with a rubeosis of unclear etiology; his visual acuity had fallen to 0.5. Doppler ultrasonography demonstrated a high-grade ipsilateral occlusion in the carotid artery. Ophthalmoscopy shows disseminated, nonconfluent areas of hemorrhage, with microaneurysms and a cotton-wool spot. The veins are distended, with no evidence of venous beading. The arteries are narrowed. b Early phase. After 15 s, there is clearly delayed, inhomogeneous choroidal filling. The retinal vessels are also filling with a definite delay. c Arteriovenous phase. The time between the first appearance of the dye in the arteries and complete filling of the veins was over 20 s in this patient (normally up to 11 s). Dot-shaped hyper-fluorescence in the region of the microaneurysms can be seen at the entire posterior pole, along with hyperfluorescence over the optic nerve head. d Late phase. Mild macular edema and persistent blockage is visible due to the areas of hemorrhage. e Arterial phase (in a different patient). Hypoperfusion in high-grade stenosis of the carotid arteries; the patient did not report any reduction in visual acuity. Very weak appearance of the dye in the retinal vessels can be seen only after 20 s. f Arteriovenous phase. Again, more than 20 s pass before complete filling of the retinal veins. No areas of hemorrhage or microaneurysms are evident yet. Fig. 7.3a–f Central retinal vein occlusion a Color photograph. Ischemic central retinal vein occlusion, with massive retinal edema, cotton-wool spots, distended veins and increased tortuosity of the vessels, and disseminated retinal hemorrhages in all quadrants. b Arteriovenous phase. There are areas of hypofluorescence due to hemorrhage (blockage) and extended capillary dropout (hypoperfusion), and areas of hyperfluorescence due to leakage from the distended vessels and accumulation in the vessel walls. There is a clearly extended arteriovenous passage time. c Late arteriovenous phase. Increasing preretinal leakage is evident from the diffuse fluorescein leakage from the damaged vessels. Fluorescein staining is seen in the congested vein walls. d Arteriovenous phase (in a different patient) 1 year after ischemic central retinal vein occlusion. Pigment epithelial changes in the central macula (with clearly demarcated areas of hyperfluorescence and hypofluorescence), capillary dropout and expansion of the parafoveal capillary network, and extended cilioretinal shunt vessels on the optic nerve head, are recognizable as sequelae of the central retinal vein occlusion. Scarred laser coagulation spots are visible above and below (a hypofluorescent center with a hyperfluorescent rim). e Color photograph. Nonischemic central retinal vein occlusion with relatively few areas of streaky retinal hemorrhage, moderately extended veins with increased tortuosity, no cotton-wool spots, mild retinal edema, and low-grade macular edema. f Arteriovenous phase. There is moderate distension and increased filling of the retinal veins, a moderately extended arteriovenous passage time, no capillary dropout, mild congestion with extended capillaries in the optic nerve head region, no leakage, and hypofluorescence due to hemorrhage (blockage). Cooney MJ, Fekrat S, Finkelstein D. Current concepts in the management of central retinal vein occlusion. Curr Opin Ophthalmol 1998;9:47–50. Hayreh SS. Management of central retinal vein occlusion. Ophthalmologica 2003;217:167–88. Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders Prog Retin Eye Res 2005;24:493–519. Hayreh SS, Zimmerman MB, Podhajsky P. Hematologic abnormalities associated with various types of retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 2002;240:180–96.
Epidemiology, Pathophysiology, and Clinical Presentation
 Diseases of the cardiovascular system are the most frequent causes of morbidity and mortality in the industrialized nations, and hypertension is the most important treatable risk factor for cardiovascular disease. In the USA, 38% of the population between 45–64 and 71% of the population of 65 years and over are affected.
Diseases of the cardiovascular system are the most frequent causes of morbidity and mortality in the industrialized nations, and hypertension is the most important treatable risk factor for cardiovascular disease. In the USA, 38% of the population between 45–64 and 71% of the population of 65 years and over are affected.
 Hypertensive retinopathy can be observed with acute or chronic increases in blood pressure. It is an independent risk factor for increased cardiovascular mortality.
Hypertensive retinopathy can be observed with acute or chronic increases in blood pressure. It is an independent risk factor for increased cardiovascular mortality.
 In patients with chronic hypertension, focal narrowing of the arterioles, capillary hypoperfusion, and cotton-wool spots are seen. Damage to the blood–retina barrier, leading to intraretinal hemorrhage and exudates, can also be noted. Long-term changes in the vascular architecture lead to endothelial-cell hyperplasia, hyalinization of the intima, and hypertrophy of the media, which are visible ophthalmoscopically in the form of copper-wire arteries and can lead to signs of arteriovenous crossing. In extreme cases, the disease progresses to proliferative retinopathy and edema of the optic nerve head.
In patients with chronic hypertension, focal narrowing of the arterioles, capillary hypoperfusion, and cotton-wool spots are seen. Damage to the blood–retina barrier, leading to intraretinal hemorrhage and exudates, can also be noted. Long-term changes in the vascular architecture lead to endothelial-cell hyperplasia, hyalinization of the intima, and hypertrophy of the media, which are visible ophthalmoscopically in the form of copper-wire arteries and can lead to signs of arteriovenous crossing. In extreme cases, the disease progresses to proliferative retinopathy and edema of the optic nerve head.
 When there are acute and massive increases in blood pressure, hypertensive choroidopathy may be observed. As a result of fibrinoid necrosis of the choroidal vessels, focal damage to the outer blood–retina barrier at the pigment epithelium takes place, with localized retinal detachment. Focal hyperpigmentation of the retinal pigment epithelium with a surrounding halo (Elschnig spots) can be seen in the healing phase.
When there are acute and massive increases in blood pressure, hypertensive choroidopathy may be observed. As a result of fibrinoid necrosis of the choroidal vessels, focal damage to the outer blood–retina barrier at the pigment epithelium takes place, with localized retinal detachment. Focal hyperpigmentation of the retinal pigment epithelium with a surrounding halo (Elschnig spots) can be seen in the healing phase.
 Patients with hypertensive retinopathy have an increased risk of developing retinal macroaneurysms (see section 7.7), retinal vein occlusions (see sections 7.3, 7.4), and anterior ischemic optic neuropathy (see section 10.1).
Patients with hypertensive retinopathy have an increased risk of developing retinal macroaneurysms (see section 7.7), retinal vein occlusions (see sections 7.3, 7.4), and anterior ischemic optic neuropathy (see section 10.1).
 Pregnancy-induced hypertension in preeclamptic patients induces retinal and choroidal ischemia that is usually diagnosed ophthalmoscopically.
Pregnancy-induced hypertension in preeclamptic patients induces retinal and choroidal ischemia that is usually diagnosed ophthalmoscopically.
Fluorescein Angiography
 The basic signs of hypertensive retinopathy can be diagnosed ophthalmoscopically, without angiography; however, advanced vessel changes can be visualized better using angiography.
The basic signs of hypertensive retinopathy can be diagnosed ophthalmoscopically, without angiography; however, advanced vessel changes can be visualized better using angiography.
 In advanced cases, retinal capillary occlusion (areas of hypofluorescence due to hypoperfusion), changes to the capillary architecture (particularly perifoveal, peripapillary, temporal to the fovea, and along the arterioles), microaneurysms (dot-like areas of increasing hyperfluorescence with moderate leakage), increased vessel tortuosity (particularly in the arterioles), arteriovenous anastomoses (new vessel lumina with low leakage) and leakage over the optic nerve head, in conjunction with optic disc swelling, can all be observed using fluorescein angiography.
In advanced cases, retinal capillary occlusion (areas of hypofluorescence due to hypoperfusion), changes to the capillary architecture (particularly perifoveal, peripapillary, temporal to the fovea, and along the arterioles), microaneurysms (dot-like areas of increasing hyperfluorescence with moderate leakage), increased vessel tortuosity (particularly in the arterioles), arteriovenous anastomoses (new vessel lumina with low leakage) and leakage over the optic nerve head, in conjunction with optic disc swelling, can all be observed using fluorescein angiography.
 Choroidal filling is often delayed and irregular, and is sometimes only recognizable after filling of the retinal vessels has taken place.
Choroidal filling is often delayed and irregular, and is sometimes only recognizable after filling of the retinal vessels has taken place.
 Focal leakages arise over pigment epithelial defects in hypertensive choroidopathy.
Focal leakages arise over pigment epithelial defects in hypertensive choroidopathy.
Diagnosis and Treatment
 Medical treatment for arterial hypertension is the initial measure. Visual acuity is often still surprisingly good in patients with hypertensive retinopathy, even in those with advanced disease.
Medical treatment for arterial hypertension is the initial measure. Visual acuity is often still surprisingly good in patients with hypertensive retinopathy, even in those with advanced disease.
 Ophthalmological diagnosis is clinically important when there is acute blood pressure deterioration (in patients with previously unknown hypertension), for identifying chronic retinal vessel changes in newly diagnosed hypertension, and in patients with advanced retinopathy. Ophthalmological treatment using laser coagulation is generally necessary if proliferative retinopathy develops.
Ophthalmological diagnosis is clinically important when there is acute blood pressure deterioration (in patients with previously unknown hypertension), for identifying chronic retinal vessel changes in newly diagnosed hypertension, and in patients with advanced retinopathy. Ophthalmological treatment using laser coagulation is generally necessary if proliferative retinopathy develops.
References
7.2 Ocular Ischemic Syndrome
Epidemiology, Pathophysiology, and Clinical Presentation
 In the ocular ischemic syndrome, retinal hypoperfusion takes place as a result of narrowing of the ipsilateral carotid artery (with narrowing of the lumen by more than 80%), mostly secondary to arteriosclerosis.
In the ocular ischemic syndrome, retinal hypoperfusion takes place as a result of narrowing of the ipsilateral carotid artery (with narrowing of the lumen by more than 80%), mostly secondary to arteriosclerosis.
 Patients often report amaurosis fugax, or slow or sudden reductions in visual acuity; however, the disease can also become symptomatic without visual disturbances—for example, due to a secondary glaucoma. Ocular or periorbital pain is a relatively typical symptom (and is also independent of the appearance of a secondary glaucoma). The patients are usually over 60, with men being affected more often than women.
Patients often report amaurosis fugax, or slow or sudden reductions in visual acuity; however, the disease can also become symptomatic without visual disturbances—for example, due to a secondary glaucoma. Ocular or periorbital pain is a relatively typical symptom (and is also independent of the appearance of a secondary glaucoma). The patients are usually over 60, with men being affected more often than women.
 The estimated incidence is between one in 10 000 and one in 100 000. The disease pattern is probably under-diagnosed and is frequently confused with other retinal vessel diseases. Bilateral disease is observed in approximately 20% of the patients.
The estimated incidence is between one in 10 000 and one in 100 000. The disease pattern is probably under-diagnosed and is frequently confused with other retinal vessel diseases. Bilateral disease is observed in approximately 20% of the patients.
 Neovascularization of the anterior segment occurs in 60–80% of the affected patients. Additional characteristics include a pale optic disc, constriction of the retinal arteries, distension of the veins, and fundus hemorrhages. Retinal neovascularization occurs in up to 13% of the patients.
Neovascularization of the anterior segment occurs in 60–80% of the affected patients. Additional characteristics include a pale optic disc, constriction of the retinal arteries, distension of the veins, and fundus hemorrhages. Retinal neovascularization occurs in up to 13% of the patients.
 The syndrome is associated with diabetes mellitus (56%), hypertension (50%), coronary sclerosis (38%), and symptomatic cerebral hypoperfusion (31%). Patients with ocular ischemic syndrome have a markedly increased risk of other arterial occlusive diseases, such as cerebral and cardiac ischemia.
The syndrome is associated with diabetes mellitus (56%), hypertension (50%), coronary sclerosis (38%), and symptomatic cerebral hypoperfusion (31%). Patients with ocular ischemic syndrome have a markedly increased risk of other arterial occlusive diseases, such as cerebral and cardiac ischemia.
Fluorescein Angiography
 Typical findings are a delay in the appearance of fluorescein in the retinal/choroidal circulation system (with prolongation of the arm–retina time, which is normally 10–12 s) and an extended arteriovenous passage time.
Typical findings are a delay in the appearance of fluorescein in the retinal/choroidal circulation system (with prolongation of the arm–retina time, which is normally 10–12 s) and an extended arteriovenous passage time.
 Irregular filling of the vascular system is also noticeable in addition to the delay during choroidal filling.
Irregular filling of the vascular system is also noticeable in addition to the delay during choroidal filling.
 The arteries are generally constricted and the veins distended, but venous beading is not usually seen.
The arteries are generally constricted and the veins distended, but venous beading is not usually seen.
 Dot hemorrhages (hypofluorescence due to blockages) and microaneurysms (increasing dot-shaped areas of hyperfluorescence) in the middle and distant periphery (and occasionally also at the posterior pole) can be distinguished angiographically. The hemorrhages are rarely confluent—a characteristic that distinguishes them from venous occlusions.
Dot hemorrhages (hypofluorescence due to blockages) and microaneurysms (increasing dot-shaped areas of hyperfluorescence) in the middle and distant periphery (and occasionally also at the posterior pole) can be distinguished angiographically. The hemorrhages are rarely confluent—a characteristic that distinguishes them from venous occlusions.
 Persistent fluorescence of the vessel walls of the retinal arteries in the late phase of angiography can be observed—in contrast to retinal arterial occlusion (in which there is no late fluorescence) or vein occlusion (which is particularly evident in the retinal veins).
Persistent fluorescence of the vessel walls of the retinal arteries in the late phase of angiography can be observed—in contrast to retinal arterial occlusion (in which there is no late fluorescence) or vein occlusion (which is particularly evident in the retinal veins).
 In a small proportion of affected patients, macular edema may be observed (with a late accumulation of hyperfluorescence in the macula without associated neovascularization).
In a small proportion of affected patients, macular edema may be observed (with a late accumulation of hyperfluorescence in the macula without associated neovascularization).
 Angiographically, cotton-wool spots show moderate hypofluorescence due to localized hypoperfusion and blockage phenomena.
Angiographically, cotton-wool spots show moderate hypofluorescence due to localized hypoperfusion and blockage phenomena.
Diagnosis and Treatment
 Medical and neurological work-up, including an examination of the carotid arteries, should be carried out if ocular ischemic syndrome is suspected clinically.
Medical and neurological work-up, including an examination of the carotid arteries, should be carried out if ocular ischemic syndrome is suspected clinically.
 Retinal perfusion can be improved and a reduction in the reported ocular symptoms can be achieved in a number of patients by lumen extension or bypass surgery.
Retinal perfusion can be improved and a reduction in the reported ocular symptoms can be achieved in a number of patients by lumen extension or bypass surgery.
 Panretinal laser coagulation can lead to regression of the proliferative disease in areas of neovascularization.
Panretinal laser coagulation can lead to regression of the proliferative disease in areas of neovascularization.
 Generally, however, the prognosis with regard to the preservation of good visual acuity or a good peripheral field of vision is poor in clinically symptomatic patients.
Generally, however, the prognosis with regard to the preservation of good visual acuity or a good peripheral field of vision is poor in clinically symptomatic patients.
References
7.3 Central Retinal Vein Occlusion
Epidemiology, Pathophysiology, and Clinical Presentation
 Central retinal vein occlusion (CRVO) occurs as a result of thrombosis of the central retinal vein at the level of, and posterior to, the lamina cribrosa. Secondary to the occlusion, there is an increase in hydrostatic pressure, with extrusion of blood components from the retinal vessels and a clear deceleration of the retinal bloodstream. Risk factors include arterial hypertension, ocular hypertension, glaucoma, damage to the vascular wall (e. g., in diabetes mellitus and inflammatory conditions), and an increase in blood viscosity.
Central retinal vein occlusion (CRVO) occurs as a result of thrombosis of the central retinal vein at the level of, and posterior to, the lamina cribrosa. Secondary to the occlusion, there is an increase in hydrostatic pressure, with extrusion of blood components from the retinal vessels and a clear deceleration of the retinal bloodstream. Risk factors include arterial hypertension, ocular hypertension, glaucoma, damage to the vascular wall (e. g., in diabetes mellitus and inflammatory conditions), and an increase in blood viscosity.
 Ophthalmoscopically, intraretinal and subretinal hemorrhages can be identified in all four quadrants, along with retinal edema with loss of retinal transparency, cotton-wool spots, extended and increased tortuosity of retinal veins, optic nerve head edema, and macular edema. The changes can appear with different grades of severity and with a wide range of interindividual variation.
Ophthalmoscopically, intraretinal and subretinal hemorrhages can be identified in all four quadrants, along with retinal edema with loss of retinal transparency, cotton-wool spots, extended and increased tortuosity of retinal veins, optic nerve head edema, and macular edema. The changes can appear with different grades of severity and with a wide range of interindividual variation.
 CRVO is usually classified as ischemic or nonischemic, but it should be borne in mind that definitions vary from study to study. Some 30% of CRVOs are assigned to the ischemic form.
CRVO is usually classified as ischemic or nonischemic, but it should be borne in mind that definitions vary from study to study. Some 30% of CRVOs are assigned to the ischemic form.
 Apart from the angiographic criteria, ischemic CRVO—in contrast to nonischemic CRVO—usually presents with a large number of fundus hemorrhages and cotton-wool spots, visual acuity of < 0.1, loss of peripheral visual fields, relative afferent pupillary deficit, and reduced amplitudes and delayed timing in the full-field electroretinogram.
Apart from the angiographic criteria, ischemic CRVO—in contrast to nonischemic CRVO—usually presents with a large number of fundus hemorrhages and cotton-wool spots, visual acuity of < 0.1, loss of peripheral visual fields, relative afferent pupillary deficit, and reduced amplitudes and delayed timing in the full-field electroretinogram.
 Major complications include a permanent reduction in visual acuity resulting from macular damage and the development of a neovascular glaucoma, which usually occurs within 7–8 months of the onset of the disease with ischemic CRVO.
Major complications include a permanent reduction in visual acuity resulting from macular damage and the development of a neovascular glaucoma, which usually occurs within 7–8 months of the onset of the disease with ischemic CRVO.
 During the course of the disease, stages ranging from complete blindness to full recovery of visual acuity are possible. A permanent reduction in visual acuity occurs as a result of persistent macular edema, damage to either the perifoveal capillary network or the retinal pigment epithelium, prolonged retinal ischemia, or optic disc damage due to secondary glaucoma.
During the course of the disease, stages ranging from complete blindness to full recovery of visual acuity are possible. A permanent reduction in visual acuity occurs as a result of persistent macular edema, damage to either the perifoveal capillary network or the retinal pigment epithelium, prolonged retinal ischemia, or optic disc damage due to secondary glaucoma.
 The prevalence is 0.1%, a rate that is approximately five times less than that of branch retinal vein occlusion. The risk of neovascular glaucoma developing is 30–50% for ischemic CRVO and less than 10% for nonischemic CRVO. The risk of contracting central retinal vein occlusion in the fellow eye is < 10%.
The prevalence is 0.1%, a rate that is approximately five times less than that of branch retinal vein occlusion. The risk of neovascular glaucoma developing is 30–50% for ischemic CRVO and less than 10% for nonischemic CRVO. The risk of contracting central retinal vein occlusion in the fellow eye is < 10%.
Fluorescein Angiography
 The retinal veins appear broadened snake-like and have delayed filling in the venous phase of angiography. The arteriovenous time is usually prolonged. In severe cases, there is prolonged fluorescence of the vein walls.
The retinal veins appear broadened snake-like and have delayed filling in the venous phase of angiography. The arteriovenous time is usually prolonged. In severe cases, there is prolonged fluorescence of the vein walls.
 In the area of the occlusion, fleck-shaped and sometimes confluent intraretinal and preretinal hemorrhages (hypofluorescence due to blockage), retinal edema (hypofluorescence due to blockage), capillary occlusions or retinal ischemia (hypofluorescence due to hypoperfusion), intraretinal hard exudates, and cotton-wool spots can all be observed.
In the area of the occlusion, fleck-shaped and sometimes confluent intraretinal and preretinal hemorrhages (hypofluorescence due to blockage), retinal edema (hypofluorescence due to blockage), capillary occlusions or retinal ischemia (hypofluorescence due to hypoperfusion), intraretinal hard exudates, and cotton-wool spots can all be observed.
 In the late phase, areas of hyperfluorescence over the blocked veins due to dysfunction of the blood–retina barrier can be seen.
In the late phase, areas of hyperfluorescence over the blocked veins due to dysfunction of the blood–retina barrier can be seen.
 Some of the natural papillary vein drainage takes place via cilioretinal vessels. In CRVO, these are visible in angiography as collaterals with increased filling, usually without significant leakage.
Some of the natural papillary vein drainage takes place via cilioretinal vessels. In CRVO, these are visible in angiography as collaterals with increased filling, usually without significant leakage.
 Capillary occlusion in more than 10 disc diameters of the retinal surface (approximately 50% of the retina in 30° exposures) can be used as a fluorescein-angio-graphic characteristic to distinguish between ischemic and nonischemic CRVO. However, this criterion is not appropriate as a single distinctive sign for distinguishing between the two disease groups, particularly since it can often not be assessed in the first few weeks of the disease (for example, in cases of extensive hemorrhage).
Capillary occlusion in more than 10 disc diameters of the retinal surface (approximately 50% of the retina in 30° exposures) can be used as a fluorescein-angio-graphic characteristic to distinguish between ischemic and nonischemic CRVO. However, this criterion is not appropriate as a single distinctive sign for distinguishing between the two disease groups, particularly since it can often not be assessed in the first few weeks of the disease (for example, in cases of extensive hemorrhage).
 Vascular anastomoses and anomalies (better visualized with fluorescein angiography, which usually shows no leakage or only slight leakage), telangiectases (irregular vessels with moderate hyperfluorescence), and vessel proliferations (hyperfluorescence from newly formed vessels, displaying clear leakage), along with secondary glaucoma and vitreous hemorrhage, can all develop in the course of the disease.
Vascular anastomoses and anomalies (better visualized with fluorescein angiography, which usually shows no leakage or only slight leakage), telangiectases (irregular vessels with moderate hyperfluorescence), and vessel proliferations (hyperfluorescence from newly formed vessels, displaying clear leakage), along with secondary glaucoma and vitreous hemorrhage, can all develop in the course of the disease.
Diagnosis and Treatment
 More than 50% of patients with nonischemic CRVO maintain or recover visual acuity of 0.5 or more during the natural course of the disease.
More than 50% of patients with nonischemic CRVO maintain or recover visual acuity of 0.5 or more during the natural course of the disease.
 The current treatment approaches (hemodilution, anticoagulant drug treatment, radial optic neurotomy, induction of retinochoroidal anastomoses by laser coagulation, and intravitreal corticosteroid injections) are controversial, and the results have not been confirmed in prospective multicenter studies.
The current treatment approaches (hemodilution, anticoagulant drug treatment, radial optic neurotomy, induction of retinochoroidal anastomoses by laser coagulation, and intravitreal corticosteroid injections) are controversial, and the results have not been confirmed in prospective multicenter studies.
 In macular edema, the amount of leakage visible in the angiogram can be reduced using central laser coagulation, but this does not lead to improved visual acuity.
In macular edema, the amount of leakage visible in the angiogram can be reduced using central laser coagulation, but this does not lead to improved visual acuity.
 In ischemic CRVO, panretinal coagulation is recommended when areas of neovascularization appear in retina or in the iridocorneal angle. This is advocated as a preventive measure in ischemic CRVO by several groups, but it is highly controversial, since only just under half of the patients develop neovascular glaucoma and coagulation causes a reduction in the visual field.
In ischemic CRVO, panretinal coagulation is recommended when areas of neovascularization appear in retina or in the iridocorneal angle. This is advocated as a preventive measure in ischemic CRVO by several groups, but it is highly controversial, since only just under half of the patients develop neovascular glaucoma and coagulation causes a reduction in the visual field.
References
7.4 Branch Retinal Vein Occlusion
Epidemiology, Pathophysiology, and Clinical Presentation
 After diabetic retinopathy, branch retinal vein occlusion (BRVO) is the second most common retinal vascular disease, with a prevalence of 0.6%. The risk of the fellow eye developing a vein occlusion is 10%.
After diabetic retinopathy, branch retinal vein occlusion (BRVO) is the second most common retinal vascular disease, with a prevalence of 0.6%. The risk of the fellow eye developing a vein occlusion is 10%.
 BRVO typically affects patients between 50 and 70 years of age and has no gender predilection. Arterial hypertension is a major risk factor.
BRVO typically affects patients between 50 and 70 years of age and has no gender predilection. Arterial hypertension is a major risk factor.
 The pathophysiological mechanism is still unclear. Vessel wall damage and changes to the flow profile within the retinal vein probably play a decisive role.
The pathophysiological mechanism is still unclear. Vessel wall damage and changes to the flow profile within the retinal vein probably play a decisive role.
 The occlusion develops distal to any crossing of arteries and veins, and the temporal quadrants are more regularly affected. An occlusion at the level of the optic nerve head leads to occlusion of half of the retina.
The occlusion develops distal to any crossing of arteries and veins, and the temporal quadrants are more regularly affected. An occlusion at the level of the optic nerve head leads to occlusion of half of the retina.
 There is a 40% risk of proliferative disease in the affected eye in an ischemic branch retinal vein occlusion (capillary nonperfusion over more than five disc diameters).
There is a 40% risk of proliferative disease in the affected eye in an ischemic branch retinal vein occlusion (capillary nonperfusion over more than five disc diameters).
 BRVOs are generally symptomatic (with a sudden decrease in visual acuity or loss of visual fields). The reduced visual acuity is caused by macular edema, macular ischemia, or macular hemorrhage.
BRVOs are generally symptomatic (with a sudden decrease in visual acuity or loss of visual fields). The reduced visual acuity is caused by macular edema, macular ischemia, or macular hemorrhage.
Fluorescein Angiography
 The affected venous branch is distended and shows delayed filling in the venous phase.
The affected venous branch is distended and shows delayed filling in the venous phase.
 Fleck-shaped, partly confluent areas of intraretinal and preretinal hemorrhage (hypofluorescence due to blockage), retinal edema (hypofluorescence due to blockage), capillary dropout with ischemia (hypofluorescence due to hypoperfusion), intraretinal hard exudates, and cotton-wool spots can all be observed in the area of the occlusion.
Fleck-shaped, partly confluent areas of intraretinal and preretinal hemorrhage (hypofluorescence due to blockage), retinal edema (hypofluorescence due to blockage), capillary dropout with ischemia (hypofluorescence due to hypoperfusion), intraretinal hard exudates, and cotton-wool spots can all be observed in the area of the occlusion.
 In the late phase, hyperfluorescences are noticeable over the occluded vein and are typically also visible locally over the occlusion area.
In the late phase, hyperfluorescences are noticeable over the occluded vein and are typically also visible locally over the occlusion area.
 An important aspect for establishing the indication for laser coagulation is whether hyperfluorescence is visible in the late phase in the presence of macular edema, or whether the macular edema is ischemic (with extensive capillary dropout).
An important aspect for establishing the indication for laser coagulation is whether hyperfluorescence is visible in the late phase in the presence of macular edema, or whether the macular edema is ischemic (with extensive capillary dropout).
 In the course of the disease, vessel anastomoses develop and vessel anomalies occur (these are more visible with fluorescein angiography). Telangiectases (irregular vessels with moderate hyperfluorescence), microaneurysms, and vessel proliferations (hyperfluorescence caused by newly formed vessels), with secondary glaucoma and vitreous hemorrhages, can also occur.
In the course of the disease, vessel anastomoses develop and vessel anomalies occur (these are more visible with fluorescein angiography). Telangiectases (irregular vessels with moderate hyperfluorescence), microaneurysms, and vessel proliferations (hyperfluorescence caused by newly formed vessels), with secondary glaucoma and vitreous hemorrhages, can also occur.
 In contrast to neovascularization, vessel collaterals do not show any fluorescein leakage.
In contrast to neovascularization, vessel collaterals do not show any fluorescein leakage.
Diagnosis and Treatment
 The diagnosis is generally reached from the typical clinical findings. Fluorescein angiography is indicated when there is a need to identify ischemic areas and leakage in patients with macular edema (rarely in the acute stage).
The diagnosis is generally reached from the typical clinical findings. Fluorescein angiography is indicated when there is a need to identify ischemic areas and leakage in patients with macular edema (rarely in the acute stage).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree