Objective
To analyze overlaps between pregnancy and orbital inflammation (OI).
Design
Retrospective observational case series.
Methods
Eight new cases from 1997 to 2015 and 2 previously published cases were identified for inclusion in this investigation to provide the fullest clinical picture. Medical records, imaging studies, and the results of biopsies were reviewed.
Results
Three categories of association were discovered: (1) OI arising for the first time during pregnancy (5 cases); (2) OI arising within 3 months of delivery (2 cases); and (3) previously diagnosed OI reactivated or exacerbated by pregnancy (3 cases). One patient had a preexistent systemic autoimmune disease and another’s was later diagnosed. One patient had attacks during sequential pregnancies. Findings included eyelid swelling and erythema, conjunctival chemosis, pain on eye movement, minimal diplopia, the usual absence of proptosis, and general preservation of visual acuity. Imaging studies disclosed extraocular muscle swelling (8 cases), most frequently of a single lateral rectus muscle. There were 2 cases of dacryoadenitis; 1 of these and an additional case displayed inflammation of the retrobulbar fat. Corticosteroids effected resolution of most symptoms. Singleton births were normal with the exceptions of an intrauterine fetal demise owing to acrania and a molar pregnancy.
Conclusion
OI usually affects a single rectus muscle (typically the lateral) and, less often, the lacrimal gland and is often mild when it arises during or after pregnancy. Independent systemic autoimmune disease is an uncommon feature. Corticosteroids were efficacious except in 1 case with severe orbital scarring. No definitive causal relationships between pregnancy and OI could be established based on the clinical data.
Idiopathic, noninfectious orbital inflammations are by definition localized disorders. A significant number of orbital inflammations, however, may be associated with some underlying systemic condition or remote organ dysfunction. Examples of this phenomenon are granulomatosis with polyangiitis (previously known as Wegener granulomatosis), polyarteritis nodosa, multifocal fibrosclerosis (now sometimes categorized as IgG4-related disease), systemic lupus erythematosus, celiac disease, regional enteritis (Crohn disease), and ulcerative colitis. Despite its obvious frequency and accompanying pancorporeal metabolic, hormonal, and immunologic perturbations, pregnancy is not known to most ophthalmologists as being linked to episodes of orbital inflammation (OI). We summarize the findings in 8 new cases of this phenomenon and compare them with 2 others that have been previously published.
Methods
This retrospective, observational study was conducted in compliance with the rules of the Institutional Review Board at Massachusetts Eye and Ear. The office clinical records and eye pathology files were reviewed for cases of pregnant women diagnosed with orbital pseudotumor, idiopathic orbital inflammation, orbital inflammation, and nonspecific orbital inflammation at 4 tertiary care centers. Inquiries were also made of a group of 8 experienced orbital surgeons and no additional cases were identified. A total of 8 cases were assembled from the period 1997–2015 from the practices of the coauthors of this paper. The new cases were included in this series if the attacks occurred either during pregnancy or within 3 months of delivery.
The medical records were summarized ( Table ) and clinical photographs and imaging studies (computed tomography and magnetic resonance imaging scans, ultrasonograms) were reviewed. Four cases ( Table , Cases 5, 7, 8, 9) are included that were part of a report of 16 cases of orbital myositis in which the patients were mentioned in passing as having been pregnant, but no information about the pregnancies or the ocular examinations was provided. The records and microscopic slides of the patients were retrieved and reevaluated for the purposes of the current study. Also listed in the Table are the data extracted from 2 detailed earlier reports in the literature (Cases 3 and 6). Microscopic sections of 3 biopsies were available for reevaluation. A fourth biopsied case did not have microscopic slides or a pathology report available for review, except for a notation in the medical chart regarding the salient findings. No change was made in the original diagnoses among the reviewed cases. One biopsy was submitted for immunohistochemical analysis of the subtypes of the infiltrating lymphoid cells.
| Case Number | Age | Presenting Complaint/Severity | Orbital Site Initially Involved (Confirmed by Imaging) | Orbital Inflammation Initially During Pregnancy | Orbital Inflammation Initially After Pregnancy | Orbital Inflammatory Recurrences During or After Subsequent Pregnancies | Orbital Inflammatory Recurrences Not Associated With Pregnancy | Systemic Disease | Biopsy and Results | Follow-up | Treatment and Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| I. New onset during pregnancy | |||||||||||
| Case 1 | 40 | Left superolateral upper eyelid pain and swelling increasing over 3 weeks; normal vision, pupils, and motility; no proptosis | Bilateral dacryoadenitis (CT) | 28 weeks’ gestation; intrauterine fetal demise owing to acraina, anencephaly, and a complex heart malformation | Not applicable | Not applicable | Not applicable | Diabetes mellitus type 2 | Light lymphoplasmacytic infiltrate and early fibrosis of lacrimal gland | 9 months | Complete resolution of pain and swelling with oral corticosteroids (60 mg/d with 6-wk taper) |
| Case 2 | 29 | 24 hours of right eye redness; pain worse with horizontal eye movement; VA 20/30; motility full; pain with adduction; no proptosis; mild upper eyelid edema; mild segmental conjunctival chemosis medially | Right medial rectus myositis without tendon involvement (CT) | 28 weeks pregnant | Not applicable | Not applicable | Not applicable | None | Not done | 16 years | Complete resolution without treatment in 1 week (occasional acetaminophen) |
| Case 3 | 30 | Painful diplopia for 3 days; VA 20/20; 30 prism diopters of left esodeviation; abduction deficit; normal pupils; otherwise unremarkable examination | Left lateral rectus myositis without tendon involvement (MRI) | 38 weeks pregnant | Not applicable | Not applicable | Not applicable | None | Not done | 6 months | Complete resolution of pain and abduction deficit with oral corticosteroids (1.0 mg/kg/d with taper over 6 wk) |
| Case 4 | 36 | Acute erythema and edema of eyelids progressing over 3 weeks; painful horizontal diplopia; limitation of elevation and abduction; 3 mm ptosis; conjunctival injection and chemosis; 6 mm proptosis; VA 20/20 OU, normal pupils; intraocular pressure mildly elevated | Right retrobulbar tissues (ultrasound, MRI) | 16 weeks pregnant | Not applicable | Not applicable | Not applicable | Thrombotic thrombocytopenic purpura; lichen sclerosis | Moderate nonfibrotic lymphocytic infiltrate of fat | 4 months | Improvement in symptoms with 30 mg prednisone + 2-month taper and injection of 40 mg prednisone into inferolateral fat pad; residual ptosis with reduced proptosis |
| Case 5 | 27 | Subacute onset of orbital pain; eyelid swelling; diplopia; moderately limited adduction OD; normal vision; progression after pregnancy | Left lateral, medial, superior, inferior recti; right medial rectus myositis without tendon involvement (CT) | Unknown gestational date | Bilateral worsening immediately after first delivery; severe pain and motility restriction OU; mild right orbital recurrence during second pregnancy | 4 recurrences (OD > OS) | None | Not done | 5 years | Treated with NSAIDs, corticosteroids (60–80 mg/d) and radiation therapy (2000 rad); residual mild limitation of elevation OD and elevation/adduction OS | |
| II. New onset after pregnancy (within 3 months) | |||||||||||
| Case 6 | 26 | Acute upper eyelid edema and painful diplopia of 5 days’ duration; moderate adduction/abduction deficits; normal pupils | Right lateral rectus myositis without tendon involvement (MRI) | Not applicable | Symptoms began 8 days after normal delivery | Not applicable | Not applicable | None | Not done | Not available | Complete resolution after 3 days of corticosteroid treatment (dose not specified) |
| Case 7 | 33 | Acute onset of right orbital pain with eyelid swelling with diplopia; severe limitation in adduction OD and normal vision | Right lateral rectus myositis including tendon (CT) | Not applicable | Symptoms began 3 months after molar pregnancy | Not applicable | Not applicable | Developed ankylosing spondylitis 3 years after pregnancy | Not done | 18 years | Improvement with corticosteroids (60–80 mg/d); remaining mildly limited adduction OD |
| III. Recurrence of existing orbital disease during or after pregnancy | |||||||||||
| Case 8 | 24 | Acute onset of orbital pain and eyelid swelling; painful and limited adduction OS; normal vision; milder symptoms during pregnancy attack | Left medial rectus myositis including tendon (CT) | Not applicable | Not applicable | Mild recurrence during pregnancy; orbital pain and pain with eye movement; normal motility and no treatment | Left medial rectus myositis (2 episodes total prior to pregnancy) | None | Pathology report and slides unavailable for review | 3 years | Complete resolution with NSAID therapy (ibuprofen 1200–2400 mg/d for 2 wk with 6-wk taper) |
| Case 9 | 25 | Acute onset of orbital pain and eyelid swelling; painful adduction and severely limited abduction OD; normal vision | Right lateral rectus myositis including tendon (CT) | Not applicable | Not applicable | Recurrence at 3 months’ gestation; left myositis with limited abduction; left orbital recurrence at end of pregnancy; right orbital recurrence 4 months postpartum | 3 recurrences (right medial rectus; left lateral rectus x2; 4 episodes prior to pregnancy) | None | Not done | 12 years | Complete resolution with corticosteroids (multiple courses, 60–80 mg/d); also received radiation therapy (2000 rad) |
| Case 10 | 25 | Acute onset of orbital pain and eyelid swelling; VA 20/20 OU; moderately limited abduction, elevation, and depression; 7 mm proptosis OD | Lateral orbital mass including right lateral rectus myositis; dacryoadenitis; superior orbital fissure involvement (CT) | Not applicable | Not applicable | Steroid-dependent orbital disease; recurrence of existing disease at 3 months’ gestation; 20/32 vision; optic neuropathy | 3 more recurrences after pregnancy | None | Progressive fibrosis with diminishing lymphocytic infiltrate | 15 years | Steroid-dependent for many years (20–30 mg/d) with courses of 60–80 mg/d; underwent radiation and surgical debulking; no light perception; limited abduction/elevation/depression |
Results
In the overall series ( Table ), 3 categories emerged: (1) initial development of orbital inflammation, usually during the third trimester of pregnancy (5 cases); (2) orbital inflammation initially appearing after pregnancy from 5 days to 3 months (2 cases); and (3) orbital inflammation already established before pregnancy but reactivated or exacerbated during or within 3 months after pregnancy (3 cases).
The 10 patients ranged in age from 24 to 40 years (mean of 29.5 years and median of 28 years). Graves orbitopathy was ruled out by appropriate serologic testing and orbital cellulitis by radiologic demonstration of clear sinuses. Only 1 patient (#5, Table ) had 2 separate attacks of OI during sequential pregnancies. Typical complaints that developed acutely or subacutely (usually over several days) were eyelid erythema and fullness (with an accentuated lateral swelling and an S-shaped eyelid if the lacrimal gland was affected), conjunctival injection with exaggeration over the tendinous insertion of the involved muscle, pain with eye movement, diplopia in extremes of gaze, and low-grade or no proptosis (only 2 patients had 6 and 7 mm of proptosis) ( Figure 1 , Bottom left and Bottom right, and Figure 2 , Top left and Top right). Case 10 with 7 mm of proptosis, had several recurrences leading to profound visual loss. Three patients had bilateral disease: 1 with dacryoadenitis (Case 1) and the other 2 with myositis (Cases 5 and 9). One patient (Case 4, Figure 1 , Bottom left) had an already diagnosed systemic autoimmune disease before the orbital episode, while another later developed one (ankylosing spondylitis, Case 7) that emerged after subsidence of the OI. Four of the 5 patients presenting with orbital inflammation during pregnancy had mild disease (mild spontaneous orbital pain/gaze-evoked orbital pain/minor eyelid swelling/proptosis <2 mm/limited eye movement only in extreme fields of gaze); 1 initially had moderately severe disease (moderately severe spontaneous orbital pain/moderate eyelid swelling/proptosis <3 mm/moderately limited eye movement), which progressed after delivery (Case 5). The 2 patients developing orbital inflammation after pregnancy also had myositis. Severe disease (severe orbital pain/severe soft tissue swelling/severe restriction of eye movement/proptosis >3 mm/optic neuropathy) mostly characterized the group of 3 patients who already had OI before their pregnancy, which aggravated or reactivated the disease. A disastrous outcome was seen in only 1 patient in this group (Case 10, Figure 2 , Top left), who had involvement of the orbital fat involving the orbital apex and became steroid dependent, requiring radiotherapy and surgical debulking that did not avert loss of light perception.
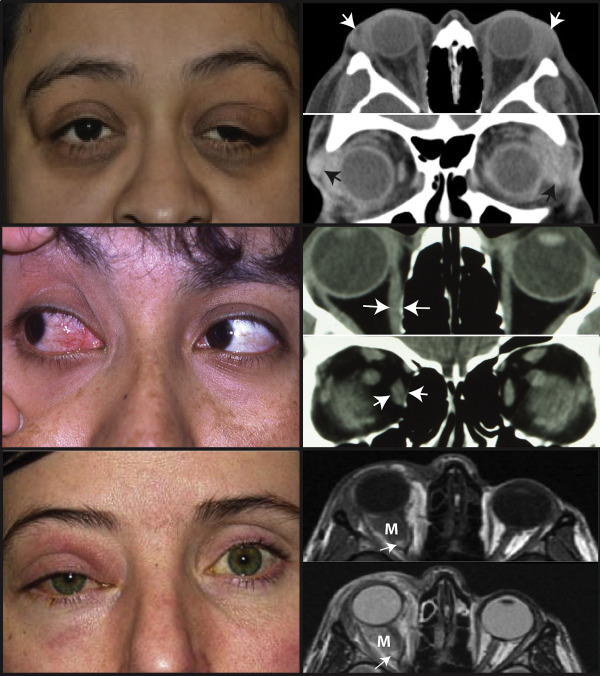
The lateral rectus was the most commonly involved single muscle, followed far behind by the medial rectus. The orbital fat was found by imaging studies to be significantly infiltrated ( Figure 1 , Bottom right, and Figure 2 , Top right) in the 2 cases with significant proptosis (Cases 4 and 10). Myositis and dacryoadenitis cases did not display this finding. Therapy for mild disease was successful with short-term courses of systemic corticosteroids or nonsteroidal anti-inflammatory drugs. Triamcinolone 40 mg was directly injected into an inflammatory mass (Case 4) with some beneficial effects. For more severe disease, longer courses and reintroduction of steroids were required, and occasionally low-dose radiotherapy (15–20 Gy) was employed. Surgical debulking was performed in the most severe case (Case 10).
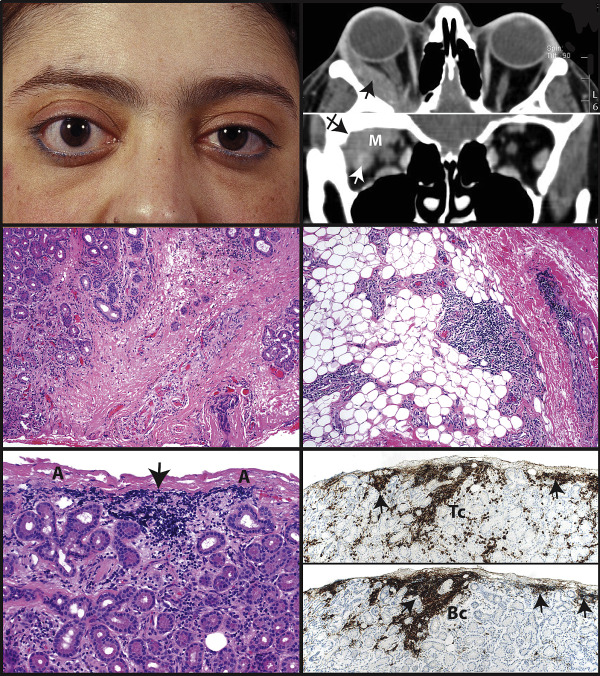
Biopsies were obtained in only 4 cases (not deemed necessary in instances of distinctive myositis). Three biopsies were available for review and revealed differences depending on the sites and stages of the biopsies. In Case 1 with bilateral lacrimal gland swellings, only the more prominent left gland was biopsied and disclosed a light periductular and interacinar lymphocytic infiltrate that also focally formed small aggregates at the peripheries of the lobules. Interstitial fibrosis was minimal and concentrated in the vicinity of the ductules ( Figure 2 , Middle left). There was disappearance of the zymogen-bearing acinar cells with survival of scattered ductules in zones where fibrosis radiated out toward the acini.
Fibroadipose tissue adjacent to the gland displayed a more pronounced perivascular lymphocytic infiltrate that extended from the fibrous septa into the fat lobules between the individual adipocytes ( Figure 2 , Middle right). In a certain sense the process resembled a periglandular (periadventital) inflammation, which made the lacrimal glands themselves appear more enlarged on computed tomography scanning than they actually were. Small lymphocytic collections were located at the peripheries of the lobules ( Figure 2 , Bottom left) and periductally. Immunohistochemical studies demonstrated, in the focal lymphoid aggregates and diffusely, a mild excess of CD3+ T lymphocytes ( Figure 2 , Bottom right, top panel) over CD20+ B lymphocytes ( Figure 2 , Bottom right, bottom panel) with interspersed CD68+ histiocytes ( Figure 3 , Top left). These findings are consistent with the normal polytypic immunoarchitecture of the gland and characteristic of its nonneoplastic, standing interacinar lymphocytic population.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


