Chapter 37
OPTIC NERVE AND VISUAL PATHWAY

Although injury of the optic nerves and afferent visual pathways may be associated with little evidence of head injury, often there is associated serious brain, facial, and orbital trauma (see Chapter 10). These cases can be especially challenging for the clinician as alterations in the state of consciousness make assessment of visual function difficult. If vision is found to be impaired, management depends upon localization of the site and mechanism of injury.
Trauma may affect any segment of the visual pathways; and accurate localization requires a complete neuroophthalmologic assessment.
• The optic radiations are generally not involved in closed head injury as they are well supported by deep white matter structures. Rarely, the occipital lobe may be injured by a blunt impact to the occiput. These patients exhibit highly congruous hemianopic visual field defects with no pupillary abnormality.
• Traumatic chiasmal injury, although rare, produces bitemporal hemianopic field defects, and may be associated with endocrine disorders due to hypothalamic involvement.1–3
PEARL… The optic nerves are by far the most common site of visual pathway trauma.4
For the purposes of management, TON can be classified into three types of injuries5:
1. optic nerve evulsion, where the optic nerve is partially or completely separated from the globe (Fig. 37–1);
2. direct injury caused by impact on the optic nerve or nerve sheath from a penetrating foreign body, a displaced bone fragment, or a retroorbital hematoma; and
3. indirect injury, in which forces are transmitted to the optic nerve within the optic canal.
This chapter focuses on the various forms of TON (additional details can be found in Chapter 38).
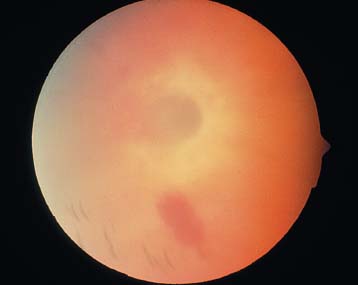
FIGURE 3 7–1 Typical appearance of an optic nerve evulsion with retinal hemorrhages and a nonrecognizable optic disk structure.
Incidence: TON occurs in approximately 1.6% of cases of head trauma and 2.5% of cases of midface and maxillofacial trauma.
Age: 1–89 years (mean: 29).
Sex: the male-female ratio is 4:1.
Place: home is most common, followed by highway and workplace environments (USEIR data; see Table 37–1).
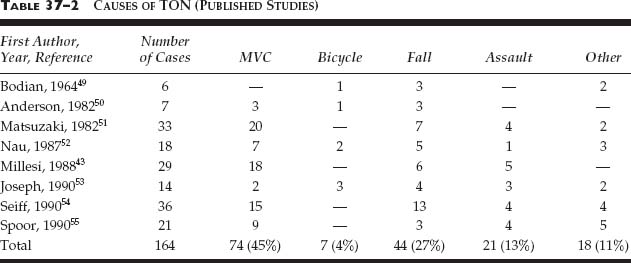
Cause: most often due to deceleration injury (see Table 37–2).
• MVCs and bicycle accidents are the most frequent cause (45% of the cases).
• Falls are the next most common cause (27%).
• Motorcycle crashes are a particularly high risk for TON (18% of the cases).
• In the USEIR, gunshot wounds are the most common source of injury (26%), followed by various blunt objects (see Table 37–3).
| Work/industrial | 11% |
| Farm | 2% |
| Home | 33% |
| School | 1% |
| Recreation/sport | 12% |
| Street/highway | 23% |
| Public building | 3% |
| Unknown | 12% |
| Other | 3% |
*Based on 427 cases.
Regardless of the type of TON, damage may occur via both primary and secondary mechanisms (see later in this chapter).6 Undoubtedly, several of these mechanisms are interdependent and occur simultaneously or consecutively.
PEARL… Indirect TON may occur after seemingly trivial injury to the head or superior orbital rim. Blunt impact to this region is transmitted along the orbital roof to the optic canal.
PATHOPHYSIOLOGYa
Primary Mechanisms
• Shearinga injury: the force generated by a blunt object’s impact to the head, most commonly the forehead, can be transmitted to the optic nerve through the walls of the bony orbit and cause a shearing injury to the optic nerve (Fig. 37–2).7 However, shearing of axons is no longer considered a common form of neurologic injury. Rather, trauma induces a focal disruption of axonal transport, which functionally separates the nerve leading to wallerian degeneration of the distal segment.8
| Hammer on metal | 2% |
| Sharp object | 5% |
| Nail | 2% |
| Blunt object | 24% |
| Fall | 3% |
| Gunshot | 26% |
| BB/pellet gun | 10% |
| MVC | 19% |
| Fireworks | 2% |
| Explosion | 2% |
| Lawn equipment | 1% |
| Unknown | 1% |
| Other | 3% |
* Based on 427 cases.

FIGURE 37–2 Transmission of lines of force from blunt frontal impact to the optic canal at the orbital apex.
• Laceration: either partial or complete laceration of the optic nerve or its sheath may occur due to a penetrating foreign body or a displaced bone fragment.
• Compression: penetrating foreign bodies or displaced bone fragments may compress the optic nerve as a primary mechanism of injury. Compression of the optic nerve may also occur as a secondary mechanism due to traumatic retroorbital or optic nerve sheath hematoma (see later in this Chapter).
Secondary Mechanisms
• Ischemia: interruption of the vascular supply may occur due to:
 compression or laceration in direct TON; or
compression or laceration in direct TON; or
 tearing of the microvasculature due to shearing forces in indirect TON.6 This is perhaps the most important secondary injury following trauma.
tearing of the microvasculature due to shearing forces in indirect TON.6 This is perhaps the most important secondary injury following trauma.
• Compression: retroorbital and optic nerve sheath hematoma may occur after direct9 or indirect TON10 and may further damage the optic nerve. In addition, orbital emphysema following fractures of the paranasal sinuses is a rare cause of optic nerve compression.12
• Reperfusion injury: with resolution of the primary insult, subsequent reperfusion can generate oxygen-free radicals, which cause further injury by lipid peroxidation of axonal membranes and their supporting glial tissue.13
• Edema: bradykinin and related substances are activated following traumatic and ischemic brain injury.6 Bradykinin initiates the release of arachidonic acid, producing a loss of vascular autoregulation and subsequent edema, which in the case of TON may produce a compartment syndrome within the optic canal that increases ischemic injury.14 Bradykinin antagonists may in the future have a role in the management of TON.15 Edema within the optic canal may elevate intracanalicular pressure and further exacerbate optic nerve injury.
• Intracellular calcium is increased after traumatic or ischemic damage to the nervous system and may lead to further cell death.14
• Inflammation is triggered by the release of inflammatory mediators due to the initial insult. First, polymorphonuclear cells arrive within 1–2 days of injury and release a broad array of toxic compounds.6 Within the first week, macrophages largely replace the polymorphonuclear cells and may promote reactive gliosis, which limits opportunities for axonal regeneration.6
PEARL… The detection of a compressive hematoma is critical because its evacuation may halt further visual decline and even improve vision.11
Pathophysiology Specific to the Type of TON
Optic Nerve Evulsion
It is the rarest form of TON. Evulsion may occur secondary to both open and closed globe trauma. However, closed trauma (i.e., contusion) is more common, and evulsion is most commonly seen with severe blunt trauma to the orbit.
• Total evulsion of the optic nerve occurs when the vitreous and retina separate from the optic disk, and the lamina cribrosa is ripped from its attachments to the choroid and sclera. The retinal vessels may be partially or totally disrupted.16
• Partial evulsion involves a localized segment of the optic disk with incomplete disruption of laminarscleral connections.
Three mechanisms have been postulated17.
1. Traumatic compression of the globe rapidly raises the IOP to the point that the optic nerve is pneumatically disinserted.
2. Orbital trauma associated with a sudden rise in the intraorbital pressure stretches the optic nerve until it is evulsed from its scleral insertion.
3. Extreme rotation and displacement of the globe within the orbit disrupt the laminar region of the optic disk. This mechanism is seen with finger jab injuries into the orbit and is associated with optic nerve evulsion with minimal ocular damage.b
Direct TON
Direct optic nerve injury may be caused by penetrating impact from:
• blunt (e.g., a BB pellet), or sharp (e.g., a knife) foreign objects; or from a
• displaced fracture or spicule of bone in the region of the optic canal.18
Less commonly, compression of the optic nerve may occur following trauma due to a retroorbital or optic nerve sheath hematoma.9 Orbital emphysema has rarely been associated with TON following orbital fractures and is due to air forced into the orbit through the fracture as a result of vomiting or nose blowing.12
Indirect TON
It is the most common form of TON.6
• The intracanalicular optic nerve is the most vulnerable to external blunt injury.1 This 6- to 12-mm segment of the optic nerve passes through the optic canal, which lies between the two bases of the lesser wing of the sphenoid.19
• Indirect intraorbital optic nerve injury rarely occurs because of the laxity of the optic nerve in this area and the fact that it is well cushioned by surrounding orbital fat.
SPECIAL CONSIDERATION
The optic canal contains the optic nerve, meninges, the ophthalmic arteries, and postganglionic sympathetic fibers. Within the canal, the optic nerve receives its blood supply from penetrating pial branches. It is immobilized by the dura in the canal, which is fixed to the surrounding periosteum and bone (see Fig. 37–3). About 4% of patients have no bone along the medial side of the optic canal; in such cases, the optic nerve is separated from the sphenoid sinus by only sinus mucosa and dura.19
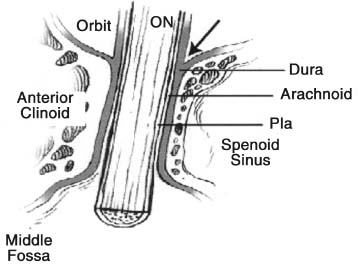
FIGURE 37–3 Anatomy of the optic nerve and canal illustrating the continuity of the orbital periosteum and dura surrounding the optic nerve (arrow).
Indirect injuries can be divided into anterior and posterior types.
• Anterior indirect TON denotes involvement of the optic disk and the segment of the retrobulbar optic nerve containing the central retinal artery.20 In these cases, ophthalmoscopic abnormalities are present:
 central retinal artery occlusion with an edematous retina, pale optic disk, threadlike arterioles, sludging of blood flow, and a cherry-red macular spot;
central retinal artery occlusion with an edematous retina, pale optic disk, threadlike arterioles, sludging of blood flow, and a cherry-red macular spot;
 retinal vasospasm (may occur without total occlusion)1;
retinal vasospasm (may occur without total occlusion)1;
 diffuse swelling of the optic disk21,c; and
diffuse swelling of the optic disk21,c; and
 tears of the optic disk margin.
tears of the optic disk margin.
• The diagnosis of posterior indirect TON requires:
 signs of optic nerve dysfunction following trauma;
signs of optic nerve dysfunction following trauma;
 no ophthalmoscopic abnormalities; and
no ophthalmoscopic abnormalities; and
 no evidence of chiasmal dysfunction.
no evidence of chiasmal dysfunction.
PEARL… Optic disk margin tears are usually associated with hemorrhage of the optic disk of less than 120 degrees. Over a period of 1 to 4 weeks, these hemorrhages resolve, leaving a heavily pigmented scar at the disk margin and optic disk pallor. The visual field defects typically correlate well with the location of the optic disk injury.
Over 4 to 8 weeks, disk pallor develops. The site of injury in these cases may occur anywhere between the chiasm and the entry of the ophthalmic artery into the optic nerve. This is the most common type of indirect optic nerve injury.18
EVALUATION
Optic Nerve Evulsion
The visual acuity may be reduced to a variable degree in partial evulsion; in total evulsion, the eye’s vision is NLP.
The fundus picture changes with time.
• Immediately after the injury, the disk is often obscured by overlying vitreous hemorrhage.
• Over time, as the view gradually improves, the disrupted disk contour becomes visible and in cases of total evulsion, the scleral canal is seen devoid of the optic disk.
• This defect is gradually filled with glial tissue, which may extend into the vitreous.17
• The differential diagnosis of this fundus appearance includes staphyloma, optic pit, optic disk coloboma, and morning-glory syndrome.d
• In cases in which the disk is obscured by vitreous hemorrhage, orbital imaging with ultrasound or CT scanning may be useful in confirming the presence of optic nerve evulsion.23
• Associated ocular findings commonly include subconjunctival hemorrhage, limitation of extraocular movement, proptosis, and a dilated and amaurotic pupil.
Indirect TON
Examination of the visual system after head trauma may be difficult and measurement of the visual acuity may be impossible. However, every effort should be made to assess the visual function.
• In the alert verbal patient, a visual acuity measurement may be obtained at the bedside. Visual loss may range from a minimal decline to NLP. Absence of light perception should be carefully confirmed with the IBO by illuminating all four quadrants (see Chapter 9).
• Pupillary responses are of critical importance and provide an objective sign of optic nerve injury.24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


