Open Tracheostomy
Eugene N. Myers
INTRODUCTION
Tracheostomy is one of the oldest surgical procedures recorded in human history and was born from the omnipresent condition of impending death from airway obstruction. The procedure described in predynastic Egyptian tablets that many interpret as the earliest images of tracheostomy dates from about 3600 BC. The Rig Veda, a Hindu text, gives a clear description of entering the anterior neck and trachea. In the fourth century BC, Alexander the Great was said to have performed a tracheotomy with the tip of his sword on a soldier who was choking. On the other hand, the most glaring omission in the history of our country was the lack of a tracheostomy in the case of George Washington when he had airway obstruction from epiglottitis. He was treated with bleeding rather than tracheostomy and died soon after.
Despite the evolving techniques for management of diseases and trauma, access to the tracheal lumen will remain an imperative to ensure adequate ventilation. The evolution of tracheotomy and intubation through the natural route is a remarkable chronicle of disease, survival, medical and surgical evolution, creative tool making, and scientific discovery. Tracheal cannulation will always be a crucial element in the management of a wide variety of conditions of the upper aerodigestive tract. This rich history should provide surgeons with valuable perspectives on their current strategies for management of the airway.
Tracheostomy may be one of the easiest or most difficult and frustrating of surgical procedures. When the procedure is elective, performed in the operating room on an adult with a slender neck and no airway obstruction, it is usually a simple straightforward procedure associated with few, if any, problems. In contrast, the same procedure on a patient with a short fat neck struggling because of air hunger may be one of the most difficult and frustrating of surgical procedures.
The highest priority before performing a tracheostomy is securing the airway. Endotracheal intubation is the most common way of securing the airway while a more permanent airway is achieved by performing a tracheostomy. The optimal conditions for performing a tracheostomy include having the patient in the operating room with a secure airway, adequate light, suction, proper instruments, and experienced assistants.
HISTORY
The indications for tracheostomy fall into three major categories including alleviation of upper airway obstruction, maintenance of pulmonary toilet, and long-term ventilatory support. The history of upper airway obstruction may be very brief such as in patients with trauma to the neck, foreign body aspiration, and acute infection.
The patient may be seen in the emergency room with airway problems, which require immediate tracheotomy in order to alleviate the obstruction. In the above-mentioned problems, endotracheal intubation may be impossible due to massive bleeding or marked distortion of the airway such as in cervical trauma. Some patients will present with air hunger, dyspnea, and, in the most dire cases, cyanosis. The history in such cases may need to be obtained from the individuals who accompany the patient, such as family or friends, and
occasionally after the fact. In some cases, particularly of trauma such as in an automobile or industrial accident, the patient may not be able to give a history or a history is available only by way of the paramedics who transported the patient from the field.
occasionally after the fact. In some cases, particularly of trauma such as in an automobile or industrial accident, the patient may not be able to give a history or a history is available only by way of the paramedics who transported the patient from the field.
The history of the patient who requires a tracheostomy for pulmonary toilet varies widely and may range from an individual who has a history of chronic aspiration due to cancer of the head and neck or its treatment to individuals who may have debilitating diseases such as emphysema, chronic obstructive pulmonary disease, acute or chronic pain, or progressive neurologic diseases such as myasthenia gravis and muscular dystrophy.
Perhaps the most frequent need for tracheostomy in modern times is to provide a secure airway in patients who require long-term ventilatory support, such as comatose patients, in patients with chronic lung disease, or in patients who have had more than 7 days of endotracheal intubation. Tracheostomy is performed in order to remove the endotracheal tube to prevent injury to the vocal cords and the subglottic region. Due to the patient’s serious condition and the presence of the endotracheal tube, the history of such patients may need to be provided by family or caregivers.
The history in other cases includes elective airway management in conjunction with the head and neck oncologic resection, acute infection such as epiglottitis, anaphylaxis, and patients who require long-term ventilatory support such as transplant patients with congestive heart failure and head trauma.
PHYSICAL EXAMINATION
The most important aspect in evaluating the patient with acute airway obstruction is to identify the etiology of the obstruction so that one can make a decision as to whether an immediate tracheostomy is necessary or endotracheal intubation can be carried out since a safe and successful tracheostomy is much easier to accomplish in a patient with a stable airway.
Evaluation of the patient’s acute airway obstruction may be hindered by air hunger, struggling or moving about, and bleeding into the upper airway. Examination of the upper airway should include an estimate of how much of the airway has been obstructed, whether there is a history of cancer of the upper airway, whether the patient is taking anticoagulants, or whether the patient aspirated a foreign body or may have been taking medication that resulted in acute allergic or anaphylactic reactions resulting in acute upper airway obstruction.
It is important to see if the patient with partial airway obstruction can be placed in the supine position for the tracheostomy without completely obstructing the airway. If not, then the tracheostomy should be carried out with the patient in the sitting position. Other important aspects in the physical examination includes the patient’s body habitus, for instance, very obese patients present a potential problem in carrying out tracheostomy. The patient with severe kyphosis, tumor involvement of the skin, and burns of the face, neck, and chest also presents a challenge for the surgeon.
Patients who will receive a tracheostomy for pulmonary toilet may already have an endotracheal tube for temporary pulmonary toilette. In these situations, the tracheostomy should be carried out with the endotracheal tube in place. If the patient is ambulatory, the tracheostomy can be carried out under a local anesthetic with intravenous sedation.
Whether to carry out the tracheostomy in the intensive care unit (ICU) setting or in the operating room is a controversial issue. However, we believe that the tracheostomy carried out in the operating room under ideal conditions will give better long-term results and fewer complications and is well worth the extra cost.
INDICATIONS FOR TRACHEOSTOMY
Airway obstruction such as compression outside the tracheal lumen due to a thyroid mass
Trauma to the neck causing severe injury to the laryngeal framework, great vessels, or hyoid bone
Edema of the airway due to trauma, burns, infection, or anaphylaxis
Abnormality within the tracheal lumen, for example, primary tracheal tumor or subglottic extension of primary cancer of the larynx
Abnormality within the tracheal wall such as tracheomalacia
Abnormality of the epiglottis or supraglottis, such as congenital anomalies, stenosis, infection, tumor, or bilateral vocal cord paralysis
Elective airway management in conjunction with extensive surgery for cancer of the head and neck
Severe obstructive sleep apnea
To provide access for adequate pulmonary toilet especially in patients with chronic aspiration, those who are unable to cough effectively due to pain such as with fractured ribs, individuals with generalized weakness, or those who have chronic neurologic problems such as myasthenia gravis, muscular dystrophy, or multiple sclerosis
Patients requiring long-term ventilatory support, both in the ICU setting and in the chronic care hospital setting
CONTRAINDICATIONS
Patient refusal
Patients with severe coagulation disorders
Recurrent cancer of the upper digestive tract with minimal life expectancy
PREOPERATIVE PLANNING
The highest priority before performing the tracheostomy is securing the airway. It is important to determine the site and type of airway obstruction. When the tracheostomy is performed electively in a patient without airway obstruction, such as with resection of cancer of the head and neck, this is not usually a problem. The procedure in such patients may be done under local or general anesthesia prior to the resection or after the procedure prior to closing the wound. Doing the tracheostomy prior to the resection has the marked benefit of having the endotracheal tube out of the airway to provide better exposure of the tumor.
The patient with air hunger from a compromised airway should have an endotracheal tube inserted to insure that the patient is well ventilated throughout the procedure. The patient who has a large obstructive cancer of the larynx, cervical trauma, or similar type of obstruction or bleeding will not be able to be intubated and will need to have tracheostomy carried out under local anesthesia.
In patients who have partial obstruction such as a foreign body, a radiographic study may be of great help if it does not jeopardize the remaining airway. It is important in preoperative planning to decide how the patient will be positioned and whether they can actually lie in the supine position. Patients who have severe air hunger and cannot tolerate the supine position will need to have a tracheostomy carried out in a sitting position.
As far as possible, tracheostomy should be carried out in the operating room under ideal circumstances requiring the following:
Securing the airway
Adequate illumination
Adequate suction
Experienced assistants
The tracheostomy may be very simple and straightforward procedure; however, in the absence of a secure airway, illumination, suction, and assistants, the tracheostomy may be one of the most difficult, frustrating, and dangerous of surgical procedures.
SURGICAL TECHNIQUE
The patient is placed on the operating table or other firm surface with a rolled towel or sheet under the shoulders to extend the neck (Fig. 33.1). This brings the trachea more anterior in the neck and exposes more of its length. A small pillow or rubber “doughnut” should be placed under the patient’s head to stabilize it during surgery. Some patients with obstruction of the airway cannot tolerate lying supine, and in these patients, the tracheostomy must be performed under local anesthesia with the patient in a sitting or semisitting position. In other patients, such as those with cervical osteoarthritis, questionable or documented fractures of the cervical spine, or severe kyphosis, the neck cannot be extended making the procedure even more difficult.
In adults, tracheostomy may be carried out under local or general anesthesia. In patients with a difficult airway, the use of a local anesthetic allows spontaneous respiration until the airway is secured. General anesthesia, if needed, can be induced once the tracheostomy has provided a secure airway. Many patients requiring tracheostomy are at high risk of respiratory distress either because of existing airway obstruction or because of associated medical or surgical problems. When possible, these patients should undergo oral or
nasal endotracheal intubation prior to tracheostomy to secure the airway and to prevent struggling during the procedure and to be certain that the patient is well oxygenated. Patients from the ICU who are being maintained by mechanical ventilation through an endotracheal tube should undergo a tracheostomy under local anesthesia. The oxygen level should be continuously monitored with a pulse oxygen monitor.
nasal endotracheal intubation prior to tracheostomy to secure the airway and to prevent struggling during the procedure and to be certain that the patient is well oxygenated. Patients from the ICU who are being maintained by mechanical ventilation through an endotracheal tube should undergo a tracheostomy under local anesthesia. The oxygen level should be continuously monitored with a pulse oxygen monitor.
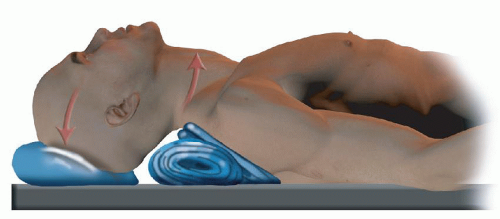 FIGURE 33.1 Positioning of patient for tracheostomy with a rolled blanket under the shoulder to extend the head. |
The line of incision should be marked on the skin prior to placing the patient in extension and before the local anesthesia is injected to avoid distortion of the anatomical landmarks. Whenever possible, the incision for the tracheostomy should be incorporated into any incision, which is planned on the neck. When using local anesthesia, Xylocaine 1% with 1:1,000,000 epinephrine should be injected into the skin and subcutaneous tissue where the incision for the tracheostomy has been outlined. Although the anesthetic effect occurs instantly after injection, it takes 5 to 10 minutes for the vasoconstrictive effect of the epinephrine to develop in order to prevent bleeding. In nonemergency situations, the local anesthetic is injected, and while the vasoconstriction is developing, the patient can be prepared and draped for surgery. In patients undergoing tracheostomy under general anesthesia, it is not necessary to inject local anesthesia since hemostasis can be secured with electrocautery. This however is the surgeon’s choice.
After the airway has been secured and the patient has been positioned correctly, the face, neck, chest, and shoulder should be sterilized with prep solution and the patient draped to allow easy access to the neck. During awake tracheostomy, I do not drape the face since this allows the surgeon to monitor the patient for pain or air hunger. Patients who have not been intubated may receive oxygen by nasal catheter. This catheter should also be prepared with antiseptic solution. The anesthetist must be notified to stop the flow of oxygen prior to the use of electrocautery in order to prevent an explosion or a fire.
A transverse incision is made in the skin approximately 1 cm above the suprasternal notch, in the triangle (Jackson triangle) bounded by the cricoid cartilage superiorly, and in the medial aspect of the sternocleidomastoid muscles laterally (Fig. 33.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


