CHAPTER 68 Open-globe injuries
Introduction
In 1996, Kuhn and associates developed a classification system intended to standardize and simplify the assessment and reporting of ocular trauma and they defined commonly used eye trauma terms1. They defined ‘rupture’ as a full-thickness wound of the eyewall (sclera and/or cornea) caused by a blunt object that results in a momentary increase in the intraocular pressure and an inside-out injury mechanism. They also clarified ‘laceration’ as a full-thickness wound of the eyewall caused by a sharp object with an outside-in mechanism. Penetrating injuries are those which are caused by a single laceration, and a perforating injury involves two full-thickness lacerations (entrance and exit) of the eyewall1.
In 1997, the Ocular Trauma Classification Group further refined this classification system for ocular trauma by providing a method of categorization during the initial examination or at the time of the primary surgical intervention (Table 68.1)2. The system classifies open-globe injuries according to the type of injury (based upon the mechanism), the grade of injury (defined by visual acuity in the injured eye at initial examination), the status of the pupil (defined as the presence or absence of a relative afferent pupillary defect in the injured eye), and the zone of the injury (based upon the anteroposterior extent of the injury). This chapter will address open-globe injuries in general, which are defined as any full-thickness wound in the cornea and/or sclera.
Table 68.1 Open-globe injury classification
| Type |
| Grade |
| Visual acuity |
| Pupil |
| Zone |
From Pieramici DJ, Sternberg P Jr., Aaberg TM Sr., et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. American Journal of Ophthalmology 1997;123(6):820–31.
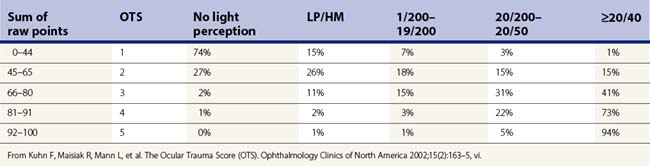
In 2002, Kuhn and associates established the ocular trauma score (OTS) in order to more accurately predict the functional outcome 6 months after a serious eye injury3. After analysis of over 2500 eye injuries, they established six variables with assigned raw points that can be summed and subsequently categorized into one of five groups (Tables 68.2 and 68.3).
Table 68.2 Calculation of the raw points for the Ocular Trauma Score
| Variable | Raw points |
|---|---|
| Initial vision | |
| NLP | 60 |
| LP/HM | 70 |
| 1/200–19/200 | 80 |
| 20/200–20/50 | 90 |
| ≥20/40 | 100 |
| Rupture | –23 |
| Endophthalmitis | –17 |
| Perforating injury | –14 |
| Retinal detachment | –11 |
| Afferent pupillary defect | –10 |
From Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmology Clinics of North America 2002;15(2):163–5, vi.
Preoperative evaluation
Initial diagnosis
The diagnosis of open-globe injury should be considered in every patient who has sustained trauma to the eye or orbit. A complete history regarding the details leading up to and following the injury is crucial in the initial assessment. Injuries sustained while hammering metal on metal should be suspected to involve an intraocular foreign body until proven otherwise. Similarly, 6% of ocular paintball injuries were found to have a ruptured globe in a study that pooled the data from multiple case series4. Systemic, life-threatening conditions may occur in conjunction with an open-globe injury and should be addressed prior to any further evaluation.
Initial diagnostic examination
Signs that suggest open-globe injury
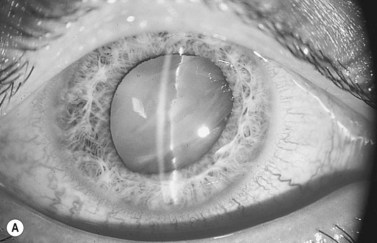
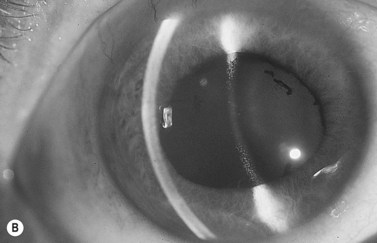
A complete ocular examination, including dilated fundus examination, should be performed when possible. Findings which suggest scleral rupture include a visual acuity of 20/400 or worse, marked chemosis, hyphema, an abnormally deep or shallow anterior chamber (Fig. 68.1), low intraocular pressure (IOP) or an IOP less than the non-traumatized eye, and a relative afferent pupillary defect5–7. The Seidel test may reveal an occult penetrating ocular injury. Finally, vitreous hemorrhage may obscure a retained intraocular foreign body.
Most frequent sites of rupture
In eyes which have not undergone prior surgery, the most frequent sites of rupture are at the limbus and parallel to the equator, and between the rectus muscle insertions and the equator8. Radially oriented ruptures under the rectus muscles are less common6. Eyes which have undergone previous surgery tend to rupture at the site of the prior surgical incision. A recent retrospective study of post-penetrating keratoplasty ruptured globes revealed that the average extent of wound dehiscence at the graft–host junction was 2.1 quadrants and involved the inferior quadrant more commonly than elsewhere9. Less frequent sites are in the cornea and at the posterior pole. Posterior ruptures, lying parallel to the equator, are usually found superiorly, in either the nasal or the temporal quadrant6.
Imaging studies
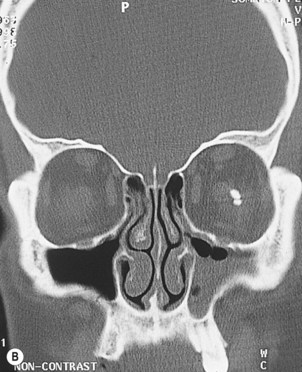
Computed tomography (CT) is the imaging technique of choice for initial assessment after ocular trauma, especially if a retained intraocular foreign body (IOFB) is suspected10,11. CT scan should be performed even if an IOFB can be visualized, since CT imaging may reveal additional IOFBs12. Thin-section axial and coronal CT images at 1.5 mm intervals are recommended for detecting IOFBs, fractures, and other soft-tissue injuries11 (Fig. 68.2). The disadvantage of CT is that non-metallic foreign bodies made of wood or plastic may be missed because they appear hypodense and may be confused with air13. Joseph et al. evaluated the use of CT scan alone for the diagnosis of open-globe injuries and found it had a sensitivity of 75% and specificity of 93%. They concluded that CT scan is not sensitive enough to be solely relied upon for diagnosis of open-globe injuries14.
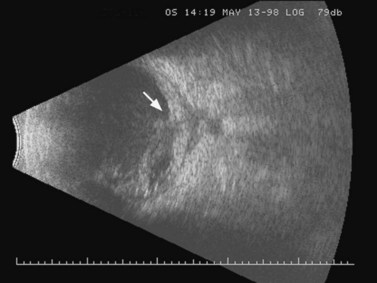
Contact B-scan ultrasonography (US) is also a useful test after ocular trauma because it can diagnose vitreous hemorrhage, retinal detachment, choroidal detachment, IOFB, and ruptured globe when clinical examination is inconclusive or the ocular media are opaque15–17 (Fig. 68.3). However, in one study, US detected less than 25% of open-globe injuries confirmed by exploration6. While CT is superior for detecting most foreign bodies, US can detect intraocular and intraorbital wooden foreign bodies13,18, is more useful for localizing foreign bodies relative to the ocular coats19, and is superior to CT in demonstrating ocular damage associated with an IOFB16.
Ultrasound biomicroscopy is a useful adjunct in evaluating eyes after trauma, especially in patients with media opacities, multiple traumatic injuries, or abnormal anatomy20. This high frequency ultrasound (50 MHz) reveals the appearance of a foreign body and surrounding tissues better than conventional low frequency ultrasound (10 Mhz)21. Like US, localization of foreign bodies near, or in, the eyewall is possible with ultrasound biomicroscopy.
Non-metallic objects that are difficult to visualize on CT or US can be visualized with magnetic resonance imaging (MRI)22. However, among the drawbacks of MRI is the potential for movement of ferromagnetic foreign bodies with deleterious effects23. Therefore, an initial CT is necessary to exclude the presence of an ocular metallic foreign body before performing an MRI24. Additionally, MRI is more expensive, not always readily available, and more sensitive to motion artifact than other forms of imaging. MRI is usually recommended if CT and US are negative, but suspicion of a retained foreign body remains high22.