Fig. 11.1
Patient using bimatoprost only in the right eye. Periorbital skin changes and hypertrichosis are noted unilaterally (Courtesy of Drs. Tarek Shazly and Mark Latina)
Pupils
I review the notes made by the ophthalmic assistant regarding the pupils. I correlate any noted RAPD with visual field findings [30]. It is worth reviewing old photos, including those on a driver’s license, for a history of anisocoria (unilateral use of miotics or dilating agents, old trauma, Horner’s syndrome [31] (Fig. 11.2), Adie’s tonic pupil [32]) or other unusual pupil findings. Pupils that do not readily dilate with drops may have had long-term exposure to miotics, posterior synechiae, or previous surgery or trauma. An attack of acute angle-closure glaucoma with very high IOP may result in a nonmotile iris even after the attack is broken [33].


Fig. 11.2
Horner’s syndrome, right side. Note ptosis, miosis, and anhidrosis
Iris
I note the presence (or absence) and location of iridotomies (previously narrow angles or acute angle closure), heterochromia (Fig. 11.3) (Fuchs’ heterochromic iridocylcitis [34, 35] (Fig. 11.4), siderosis [36], congenital Horner’s syndrome [37], unilateral use of HLs), rubeosis [38] (Fig. 11.5a, b) (neovascularization of the iris: CRVO, proliferative diabetic retinopathy, ischemic syndrome), transillumination defects [39] (pigmentary dispersion syndrome or glaucoma) (Fig. 11.6), pseudoexfoliation (Fig. 11.7a, b) material at the pupil margin [40], moth-eaten appearance of the iris (iridocorneal–endothelial (ICE) syndrome [41] (Fig. 11.8) or related diseases), and nodules [42] (Koeppe nodules, inflammatory cell precipitates at the pupillary margin found in nongranulomatous as well and granulomatous uveitis; Busacca nodules on the iris surface, which are pathognomonic for granulomatous uveitides such as sarcoidosis). Iris bombe (Fig. 11.9), a forward bowing of the iris, occurs when the pupil margin is completely bound down to the lens with posterior synechia. The forward pressure of the fluid in the posterior chamber causes the bowed appearance. Portions of the iris may be touching the corneal endothelium. Peripheral laser iridotomies, often needed in several places around the iris, will relieve this forward pressure and allow the iris to flatten to its normal position. Iris bombe may occur in both phakic and pseudophakic eyes with untreated uveitis [43–45].
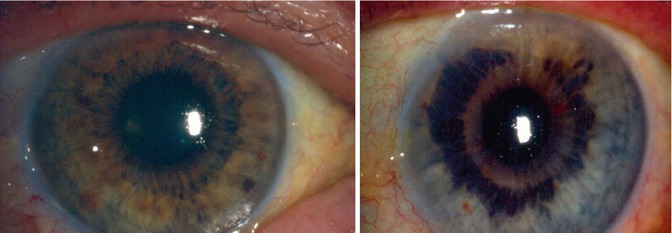
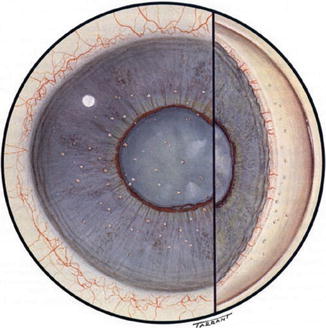
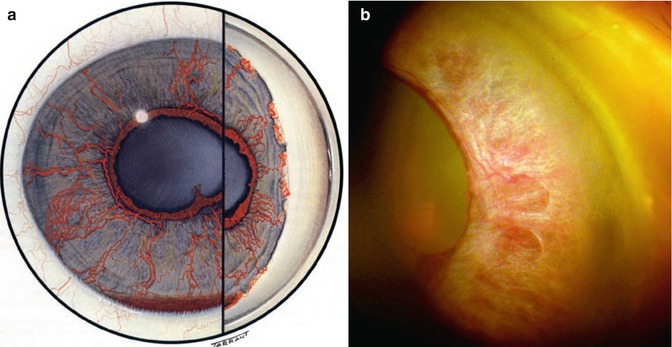
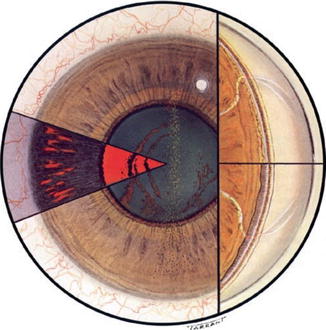
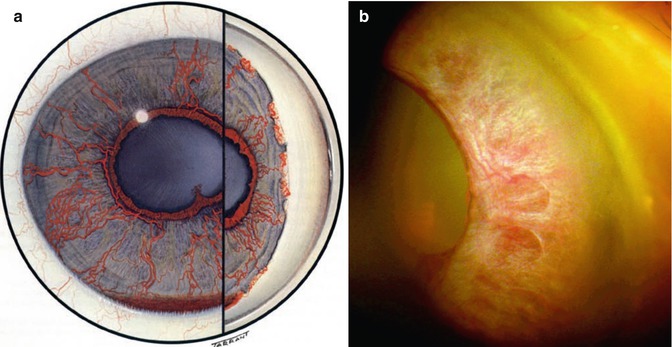
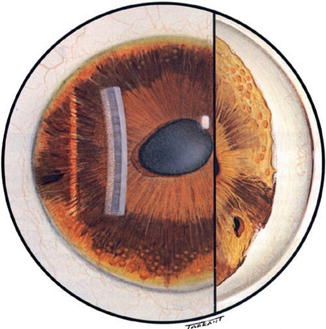
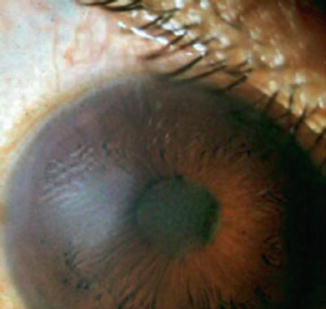
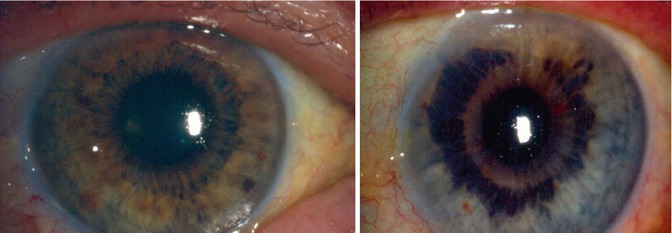
Fig. 11.3
Heterochromia of irides. The right eye is darker than the left eye (Image courtesy of http://www.medicalmediakits.com)
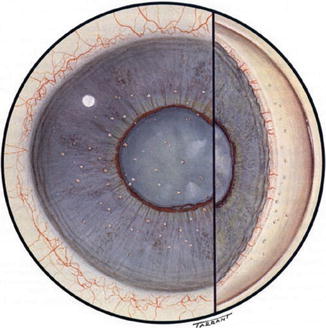
Fig. 11.4
Fuchs’ heterochromic iridocyclitis. Stellate keratic precipitates are noted (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
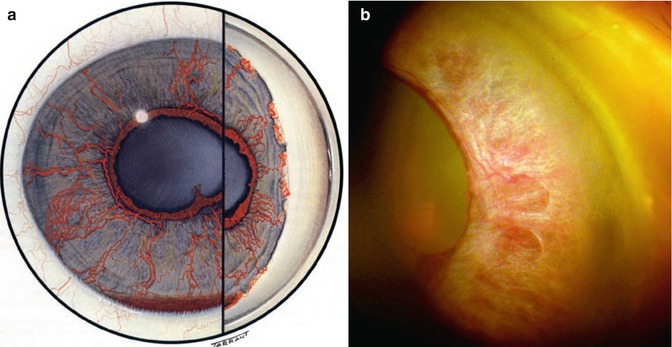
Fig. 11.5
(a) Rubeosis iridis. Fragile blood vessels occur in the iris and anterior chamber angle. (b) Rubeosis iridis, clinical photo. Neovascularization of the iris is a response to ischemia (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
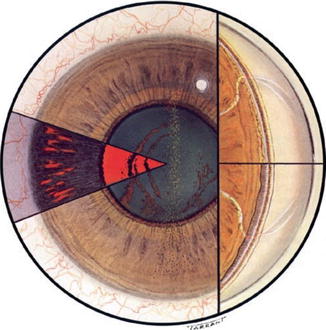
Fig. 11.6
Pigmentary dispersion syndrome and glaucoma. Transillumination defects of the iris and a Krukenberg pigment spindle are noted (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
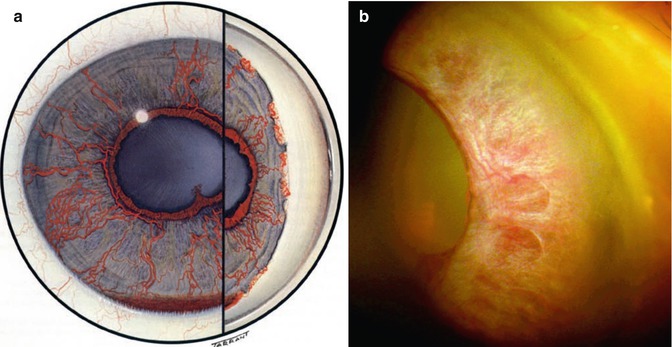
Fig. 11.7
(a) Exfoliation syndrome, clinical photo. “Dandruff-like” pseudoexfoliation material is seen on the anterior lens capsule and pupillary margin (Image courtesy of Michael P. Kelly, FOPS Duke University Eye Center). (b) Exfoliation syndrome. Sampaolesi’s line seen in the angle results from deposition of the exfoliative material anterior to Schwalbe’s line (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
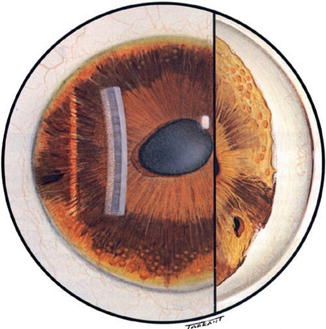
Fig. 11.8
ICE (iridocorneal–endothelial) syndrome. Corneal edema, moth-eaten appearance of the iris, and difficult to control glaucoma are common features (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
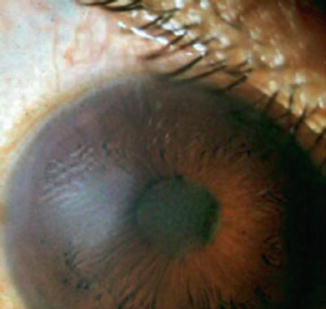
Fig. 11.9
Iris bombe. Posterior synechia completed seclude the iris causing a forward bowing with resultant angle-closure glaucoma. Laser iridotomies are curative
Conjunctiva
The patient is requested to look downward while I simultaneously lift their upper lid. I inspect the superior conjunctiva for the presence of a filtering bleb (Fig. 11.10), and if it is found, I note its location, size, shape, and quality (cystic, flat, overhanging the cornea, scarred, etc.) If glaucoma tube shunt surgery has occurred, I described the conjunctiva’s appearance and the presence of any scleral patch graft. I notice if there are any leaks from either kind of glaucoma surgery (Seidel’s test, using sterile fluorescein strips to “paint” the area of the bleb that appears to leak). I release their upper lid and ask them to look forward. I note any hyperemia, possible secondary to chronic use of glaucoma medications (and also ask about itching, burning, etc.). I look for the presence and location of any subconjunctival hemorrhages (Fig. 11.11) and review the patient’s use of aspirin, Plavix, Coumadin, etc. I ask them to look upward and inspect the lower portion of the bulbar conjunctiva. Upper and lower palpebral conjunctival areas are examined if there is significant lid margin disease or symptomatic complaints by the patient. If glaucoma surgery is being contemplated I search for areas of “virgin” conjunctiva to place new incisions.
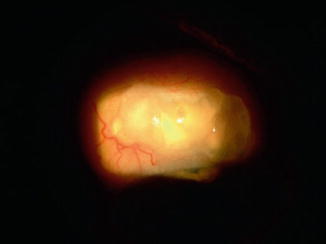

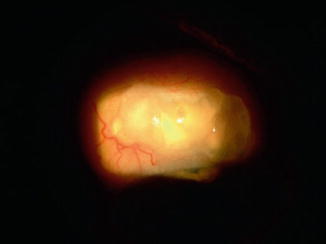
Fig. 11.10
Filtering bleb. This bleb is fairly thin and cystic as may occur with the use of antimetabolites such as mitomycin C (Courtesy of Drs. Tarek Shazly and Mark Latina)

Fig. 11.11
Subconjunctival hemorrhage. Painless accumulation of blood under the conjunctiva that usually results from rubbing, coughing, or Valsalva maneuver. Rarely related to blood dyscrasia. Frightening to patients who should be reassured that it is not sight threatening (Image courtesy of http://www.medicalmediakits.com)
Cornea
The epithelial surface, stroma, and endothelial layers of the cornea are examined using both broad and thin slit beams. I have found it increasingly helpful to take the 15 s of extra “chair time” required to do a tear breakup time (TBUT) [46, 47] test for each eye. Chronic exposure to glaucoma medications, which contain toxic benzalkonium chloride (BAK) [48] as well as the natural aging process, may lead to symptoms of ocular surface disease [49] and patient distress. Place a drop of fluorescein with anesthesia on the eye, have the patient blink, and observe the corneal surface through the slit lamp with the blue light engaged. Normal TBUTs are 10 s or longer in duration. Additionally, damaged epithelium may be detected using sterile lissamine green strips [50]. It stains devitalized corneal and conjunctival epithelium and is much gentler to the eye and patient friendly than rose bengal [51] solution.
We examine the endothelial surface for Krukenberg spindles [52] – an isosceles triangle-shaped deposition of melanin pigment found in the central posterior cornea (Fig. 11.12) associated with pigmentary dispersion syndrome (see Fig. 11.6) and glaucoma – and correlate this finding with possible radial slit-like iris transillumination defects. Transillumination defects may best be observed by making the slit-lamp beam bright and small and shining it directly through the pupil with the beam oriented directly in front of the eye, not obliquely. Pigmentary dispersion syndrome and pigmentary glaucoma are discussed in greater detail in Chap. 16.
Fig. 11.12
Krukenberg pigment spindle – “pine tree”-shaped deposition of pigment on corneal endothelium. Comes from pigment liberated from rear of iris as it scrapes lens zonules in predisposed individuals (Image courtesy of http://www.medicalmediakits.com)
Inflammatory keratic precipitates (KP) (Fig. 11.13) seen on the corneal endothelial surface are indicative of uveitis. These are collections of inflammatory cells. When the uveitis is active, they appear white. They may appear as pigmented residua from old, burned-out inflammatory disease. So-called “mutton-fat” KP are larger, have a greasy appearance, and are generally associated with granulomatous diseases (e.g., sarcoidosis). They contain both macrophages and epithelioid cells. KP may be present in all forms of nonspecific anterior uveitis. In Posner–Schlossman syndrome [53, 54] (Fig. 11.14), the KP may at first appear small and white, later taking on the appearance of pigmented rings with white centers. In Fuchs’ heterochromic iridocyclitis [55], the KP may be small and have a stellate appearance (Fig. 11.15). All forms of anterior segment inflammation may at first lead to increased intraocular pressure because of cellular debris and an inflamed trabecular meshwork, while later inflammation of the ciliary body may lead to a decreased production of aqueous humor and a fall in intraocular pressure [56].
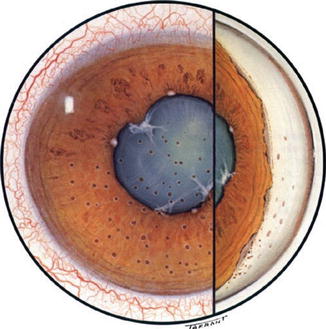
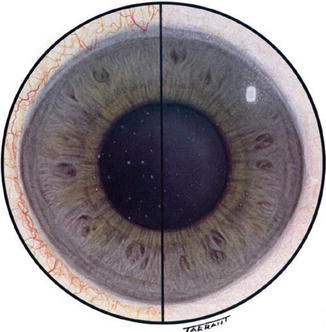
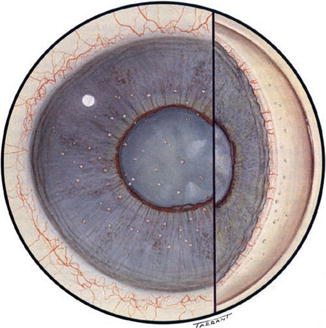
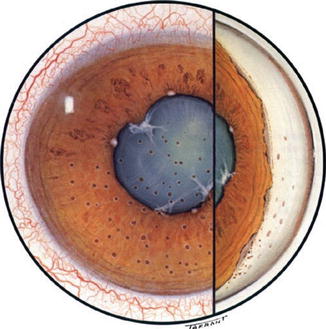
Fig. 11.13
Inflammation of the anterior segment of the eye. Keratic precipitates form on the endothelium (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
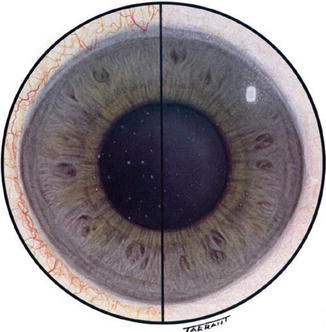
Fig. 11.14
Posner–Schlossman syndrome (glaucomatocyclitic crisis). The morphology of the KP may vary with the stage of the disease (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
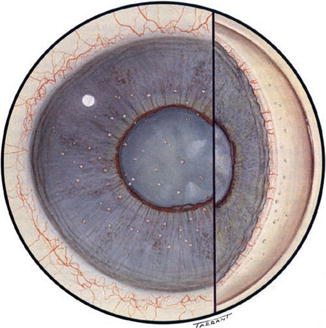
Fig. 11.15
Fuchs’ heterochromic iridocyclitis – fine white stellate KP may be present. The affected eye appears hypopigmented compared to the patient’s other eye (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
Aging changes of the corneal endothelium may appear as guttata, focal thickenings of Descemet’s membrane (Fig. 11.16). These may be indicative of early Fuchs’ endothelial dystrophy [57–59] (Fig. 11.17), a dominantly inherited, usually bilateral disease more common in women than men, usually presenting in patients older than 60 years of age. Patients with early or late Fuchs’ endothelial dystrophy may be more likely to suffer bullous keratopathy (corneal edema) after intraocular surgery (cataract or glaucoma filter). Younger, asymptomatic individuals may exhibit Hassall–Henle bodies [60], wartlike guttata at the peripheral regions of the corneal endothelium.


Fig. 11.16
Guttata are excrescences on the surface of the corneal endothelium, often a sign of aging. Found commonly in Fuchs’ endothelial dystrophy (Image courtesy of http://www.medicalmediakits.com)
Fig. 11.17
Fuchs’ endothelial dystrophy, clinical photo. Guttata are seen on the back of the corneal endothelium (Image courtesy of http://www.medicalmediakits.com)
If present, I comment on the appearance of an arcus senilis (Fig. 11.18), which represents lipid deposition in the peripheral corneal stroma. When opaque, an arcus may make it difficult to aim laser light through the cornea blocking the attempt to create a truly peripheral iridotomy for patients with narrow anterior chamber angles. Arcus may appear in some persons at a young age (often associated with familiar hyperlipidemia), but is more commonly found in the elderly (hence the name).
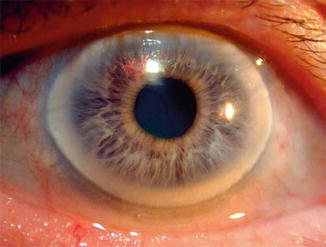
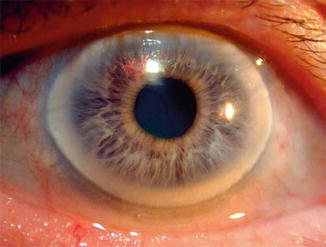
Fig. 11.18
Arcus senilis is a grayish-whitish arc or ring found in the periphery of the cornea. It causes no visual symptoms. It is more common in older individuals. If found in young patients it may be associated with hypercholesterolemia, hyperlipidemia, or hyperlipoproteinemia (Image courtesy of http://www.medicalmediakits.com)
Finally, I describe the condition (e.g., clear and compact, edematous, folds in Descemet’s membrane, neovascularized, opaque) of any penetrating keratoplasty (PKP, corneal transplant) that may be present. The presence or absence of sutures, and whether or not the knots are buried, is described in the chart notes.
Anterior Chamber
The anterior chamber (AC) is evaluated for its depth (normal, shallow centrally, or peripherally) and whether or not inflammation is present. The presence and degree of cells, flare (protein), hyphema (blood), or hypopyon (layered white cells) are noted. Cells and flare are evaluated by using a thin and narrow slit beam in a darkened room, to observe the Tyndall effect of light scattering off particles (cells) in a suspension. This is similar to the phenomenon of observing dust particles in the light beam of the projector in a darkened movie theater. Patients with uveitis are often light sensitive and are discomforted by light intensities that need be no stronger than that found in indoors with normal incandescent lighting levels. This patient symptom and complaint suggests uveitis and directs your examination to search for cell and flare. Uveitic glaucomas are more fully explored in Chap. 19.
Blood in the AC (hyphema) may be diffused or layered. Trauma is the most likely cause. Fragile abnormal blood vessels on the iris (rubeosis) or in the angle may bleed. This neovascularization may be due to proliferative diabetic retinopathy, following central retinal vessel occlusion, branch retinal vein occlusion, or ocular ischemic syndrome. Inquiries must be made about blood dyscrasias (including sickle cell anemia) and the use of anticoagulants. Blood cells can clog the trabecular meshwork and raise intraocular pressure [61]. If the IOP is raised high enough and long enough, blood staining of the cornea may occur [62].
Mechanical chaffing of the iris by an intraocular lens, usually an anterior chamber lens, can liberate blood and cause the so-called UGH syndrome (uveitis, glaucoma, and hyphema) [63, 64].
Ghost cells – pale tan remnants of blood in the vitreous – may be seen in slit beam or may layer inferiorly in the anterior chamber (Fig. 11.19). They may also clog the trabecular meshwork, usually transiently, and can cause a rise in intraocular pressure [65]. Chapter 21 elaborates on these phenomena.
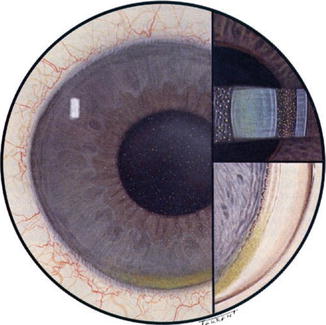
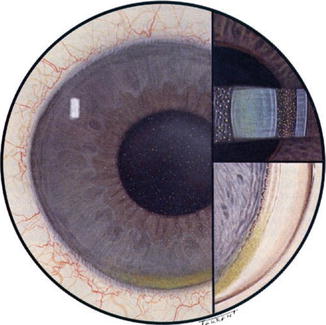
Fig. 11.19
Ghost cell glaucoma. Pale cell membranes of old blood may be seen in the vitreous or anterior chamber. They may clog the trabecular meshwork and raise intraocular pressure (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
Hypopyon – a layering of inflammatory cells inferiorly in the anterior chamber – may be sterile or infection related (Fig. 11.20). Hypopyon can result from infectious endophthalmitis, from neoplastic diseases such as leukemia or lymphoma and from inflammatory diseases of many etiologies [66–72]. IOP may increase with both inflammation of the TM and clogging caused by the cellular components.


Fig. 11.20
Hypopyon. Layered collections of white blood cells may be seen in the inferior portion of the anterior chamber in response to infection or severe inflammation (Image courtesy of http://www.medicalmediakits.com)
Gonioscopy
I perform gonioscopy, in a darkened room, at the initial examination of all glaucoma patients or suspects, without regard to how obviously open the angle appears to be on slit-lamp examination. The anterior chamber angle cannot be seen directly through the cornea, because light coming from structures in the angle undergoes total internal reflection. A goniolens replaces the cornea–air interface with a different interface having a refractive index greater than that of the cornea. Direct gonioscopy provides a direct view of the angle and indirect gonioscopy shows a reflected image from a mirror of a portion of the angle across the anterior chamber. Direct gonioscopy using Koeppe lenses is rarely performed outside of the academic environment.
I prefer to use the indirect Posner goniolens (Fig. 11.21a, b) or the similar Zeiss goniolens. These have four mirrors and thin metal handles. The indirect Sussman lens does not have a handle. While a bit more difficult to manipulate than the more traditional three-mirror Goldmann lens, the Posner and Zeiss devices have two advantages: (1) they may be used for indentation gonioscopy [73], especially helpful when evaluating narrow or slightly appositional angles, and (2) they use the patient’s tear film as an interface, requiring no gooey goniogel coupling agent [74]. Further observations of the eye are thus unimpeded by a corneal surface that is not coated with sticky methylcellulose. With the Posner/Zeiss goniolenses, this portion of the glaucoma examination is simpler for the physician and easier for the patient. Regardless of which goniolens is used, the patient’s eye must first be anesthetized with a topical agent such as proparacaine.


Fig. 11.21
(a) Posner style goniolens – in this view, the side facing the examiner is seen. This lens requires only the patient’s tears as a coupling agent. (b) The outside surface of the lens has been coated with opaque “nail polish” to help prevent scratching of the material used to provide the mirrored surface
Please note that the silvered outer surface of these prisms may be scratched easily. When I first take possession of a new Posner or Zeiss goniolens, I coat the outer surface with two layers of clear nail polish that seals the surface and prevents scratches.
I take note of the following anterior chamber angle structures (Fig. 11.22):
There is an art as well as a science to appropriately examining the anterior chamber angle by gonioscopy (see Chap. 10). Dr. Wallace Alward, of the University of Iowa, has created a superb website (http://www.gonioscopy.org/) dedicated to teaching gonioscopy skills through videography.
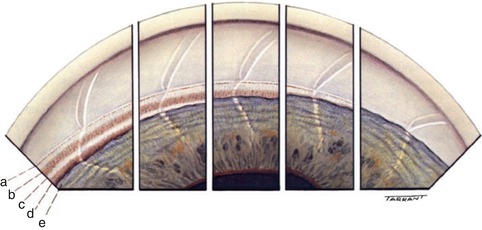
Ciliary Body Band (CBB): This is the most posterior structure in the angle. Normal color variations include pink, gray, and brownish tints. The CBB tends to be wider in myopic eyes and narrower in hyperopic eyes. Angle recession may be observed after blunt trauma. There may be a history of hyphema. Angle recession results from tears to the ciliary body along the longitudinal and meridional muscles. (Increased IOP secondary to angle recession may occur many years after the trauma – patients with angle recession should be made aware of this potential future problem and be examined every year [75].)
Scleral Spur (SS): This is the most anterior projection of the sclera. The longitudinal muscle of the ciliary body is attached to the scleral spur. On gonioscopy, SS is found just posterior to the trabecular meshwork. It appears as a narrow, whitish band.
Trabecular Meshwork (TM): The TM extends from the scleral spur to Schwalbe’s line. The posterior section starting at the SS is pigmented, with a grayish-blue translucent hue. The anterior section begins at Schwalbe’s line. It has a whitish color. Only the pigmented portion functions to pass aqueous from the eye. Increased pigmentation of the TM is observed often in patients with pigment dispersion syndrome [76] or pseudoexfoliation syndrome [77].
Schwalbe’s Line: This opaque line is the most forward structure of the anterior chamber angle. It arises from the anterior termination of the TM and the edge of the corneal Descemet’s membrane. I note the presence of peripheral anterior synechiae, iris processes, the quantity and quality of trabecular meshwork pigmentation, presence or absence of Sampaolesi’s line [78] (pigment deposited anterior to Schwalbe’s Line, often seen in pseudoexfoliation syndrome or pigment dispersion syndrome), abnormal appearance of angle vessels or neovascularization [79], and occasionally the presence of a foreign body or neoplasm in the anterior chamber angle. I estimate the degree of angle width using a modified simple Shaffer system [80] I–IV notation, from slit to narrow (I) to wide open (IV). I report the findings in Box 16 on page 2 of the consult form.
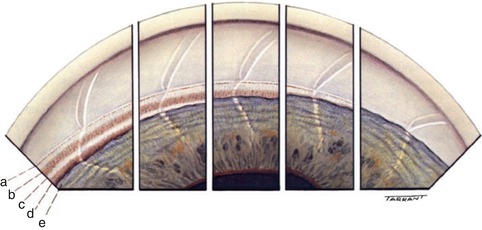
Fig. 11.22
The normal angle various widths of the normal angle seen in consecutive inserts. Note that the corneal optical wedge narrows as it approaches Schwalbe’s line and seems to end there in the situation of a narrow angle. (a) Schwalbe’s line. (b) Trabecular meshwork. (c) Scleral spur. (d) Ciliary body band. (e) Peripheral iris (Courtesy of Terry Tarrant and Alcon Labs, Fort Worth, Texas)
Gonioscopy is inexpensive, convenient, and a skill learned fairly easily. Academic medical centers may have access to anterior segment optical coherence tomography (AS-OCT) [81] and/or ultrasound biomicroscopy (UBM) [82, 83]. UBM can visualize anterior segment structures from the cornea to the ciliary body. Higher-frequency ultrasound gives better resolution but poorer penetration. UBM employs immersion techniques similar to B-scan ultrasonography. AS-OCT has higher resolution than UBM but poorer penetration. Newer AS-OCT machines have good sensitivity and specificity for diagnosing appositional angles [84].
These newer imaging modalities have been useful in examining anterior segment tumors [85, 86] as well as elucidating mechanisms behind pupillary block and plateau iris syndrome [87, 88].
Each machine has proponents advocating its use for determining the potential occludability of anterior chamber angles [89]. Devices under development may automate the process of determining the depth of the anterior chamber angle [90].
Our group has not had the luxury of using these various instruments in the community setting. Fortunately, laser peripheral iridotomy has a high benefit-to-risk ratio, so the occasional eye that is lasered because the angle appears occludable on gonioscopy but is not truly occludable seems a reasonable price to pay for those many eyes that will avoid acute angle closure.
Dilation
Dilating drops are placed in the new patient’s eyes after they have undergone the anterior segment slit-lamp exam (excluding the lens), gonioscopy, and visual field testing. The patient then sits in a waiting area for about 20 min to allow for maximum effect of the drops. Their chart is placed into a bin adjacent to one of the examining lanes being used by the physician.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


