Office Examination of the Ear
Joseph B. Nadol, Jr.
Harold F. Schuknecht
Although examination of the ear is relatively free of discomfort and is less demanding of time than most medical examinations, special equipment is needed and a meticulous routine should be followed. The wide array of ear diseases that are seen by the otologist may range from a patient with impacted cerumen to a patient in coma from otogenic meningitis. The following discussion relates to the nonemergent visit to the otologist’s office.
The office of a practicing otologist needs at least two rooms equipped for standard examination of the ear, nose, and throat. In addition, there should be a room known informally as the “scope room,” where examinations and minor procedures can be performed using a binocular microscope and an ear irrigating station. Conventional audiometry, tympanometry, brainstem evoked response (BSER), and electronystagmography (ENG) should also be incorporated into the office practice or be conveniently available.
Any medical practice benefits from the immediate availability of support facilities, such as an emergency unit, clinical laboratory, radiology, and medical consultation.
MEDICAL HISTORY
In no other specialty than otology is it more true that the right questions need to be asked to aid in the process of diagnosis. For simple problems (e.g., wax impaction), there is no diagnostic challenge, but for more complicated problems, the time of onset, rate of progression, associated symptoms, magnitude of discomfort and disability, precipitating events, previous therapy, family history, and effect on quality of life must be considered. The medical history, including review of systems and current use of medications, may reveal pertinent information.
When confronted by a patient with an ear disorder, the otologist should not make a hasty decision regarding the validity or seriousness of the complaints. Allow the patient time to present the case as he or she sees it and then proceed with questions necessary to elicit further information.
INSPECTION AND OTOSCOPY
Gross inspection and digital palpation may reveal the presence of congenital malformations, inflammatory conditions, and neoplastic disorders of the auricle, external meatus, and periauricular area.
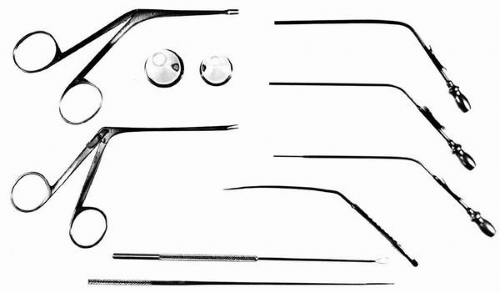
Examination of the external canal and tympanic membrane may begin with a handheld otologic speculum and illumination with a head mirror or head light. A handheld otoscope with a magnification of 2.5X and its own light source is an adequate screening tool to determine normalcy or pathology of the tympanic membrane. If a pathologic condition is detected or suspected, a binocular microscope with a magnification of 6X to 40X is essential. This can be wall mounted for examination with the patient in a sitting position or floor mounted for examination with the patient in a recumbent position (Fig. 1.1). Other handheld equipment essential for the otologic examination include no. 5 and no. 20 French suction tips, forceps (Hartmann and alligator), and wax curettes (Fig. 1.2).
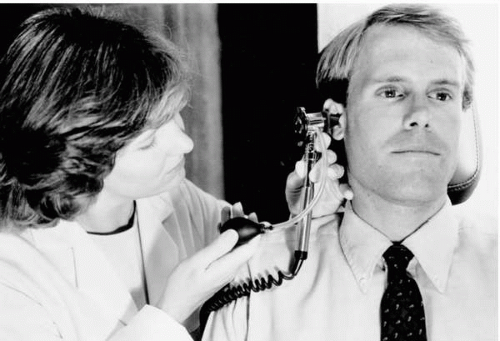
Depending on the symptoms and initial otologic findings, further examination may include pressure otoscopy (Fig. 1.3), instrumental manipulation of the manubrium and tympanic membrane, and occasionally incisions done under local anesthesia to determine the status of middle ear pathology.
Examining and recording the findings of otoscopy should be a systematic endeavor. The appropriate size of the speculum will be determined by the age of the patient, the tortuosity of both the fibrocartilaginous and bony parts of the ear canal, and the obstruction to view by hair in the meatus of male patients’ ears. It is advantageous to use the largest possible speculum. Any manipulations, such as removal of wax,
keratin, dried exudate, or other debris, and fluid discharge are best accomplished with 6X or higher magnification to prevent trauma and pain. It is essential that this be accomplished because epithelial debris, cerumen, and hardened exudate often obscure an underlying pathologic process.
keratin, dried exudate, or other debris, and fluid discharge are best accomplished with 6X or higher magnification to prevent trauma and pain. It is essential that this be accomplished because epithelial debris, cerumen, and hardened exudate often obscure an underlying pathologic process.
The external auditory canals are inspected for congenital anomalies, ulceration, granulation, stenosis, bony osteoma, or exostoses. The quality of the epidermis should be noted. The firmness of smooth outgrowths may be tested by instrumental palpation but with gentleness to prevent lacerations or hematomas. If surgery is contemplated, the extent of convexity of the anterior canal wall is recorded.
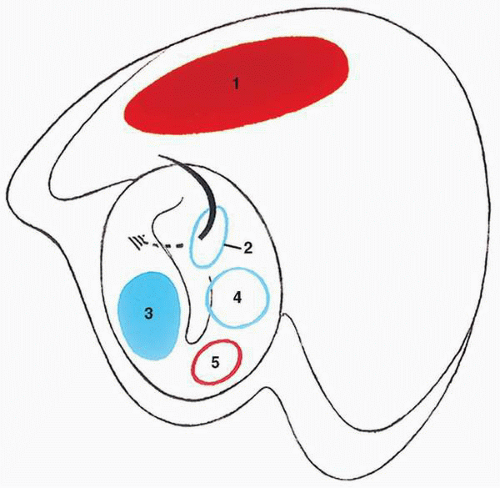
Examination of the tympanic membrane and middle ear involves the assessment of two principal anatomic areas: (i) the pars tensa and middle ear and (ii) the pars flaccida and epitympanum. Positive findings should be recorded in narrative form accompanied by a sketch. A convention for diagrammatic representation of pathology of the tympanic membrane should be adopted. For example, in our office a retraction pocket or replacement membrane is outlined in blue, a perforation outlined in red, and granulation represented as a red area (Fig. 1.4).
A patulous eustachian tube is an often overlooked disorder. The history is often adequate to make the diagnosis and consists of autophony, which disappears in the recumbent position. Examination will reveal respiratory movements of the tympanic membrane. These movements can be accentuated by having the patient block one nostril by digital pressure on the nose and breathe forcefully through the open nostril.
An intact pars tensa is not necessarily an indication of a healthy middle ear. Variations in texture and color and response to pressure otoscopy will convey to the experienced otoscopist the presence of middle ear disease such as serous effusion, acute otitis, neoplastic disease, fibrocystic sclerosis of the middle ear, and vascular anomalies (e.g., aberrant carotid, high jugular bulb). Diffuse or focal areas of retraction of the pars tensa should be identified and recorded, and if a conductive hearing loss is present, malleus mobility should be evaluated by pressure otoscopy. If the tympanic membrane shows areas of dimeric membrane (thin replacement membrane), these should be noted; retractions attached to the incus (myringoincudopexy) or stapes (myringostapediopexy) should also be identified and recorded.
Perforations of the pars tensa are characterized in terms of size and location, as well as in the appearance of their margins. Thickened margins are usually associated with fibrous thickening of the pars tensa and indicate previous chronic or recurring inflammatory disease. Keratin accumulation at the margins of the perforation is suggestive that the squamous epithelium has extended onto the medial surface of the tympanic membrane. The mucosa of the middle ear can be inspected
through the perforation and evaluated for evidence of acute or chronic pathologic change such as inflammatory or fibrous thickening, polypoid hypertrophy, ulceration, granulations, and epidermization. Exuberant tissue may be suggestive of neoplastic disease and require biopsy, but the surgeon should keep in mind the possibility of an aberrant carotid, high jugular bulb, or aberrant facial nerve. Also, biopsies and removal of polyps, which may be an essential part of a thorough evaluation of the ear, should be done without disturbing the ossicles, particularly the stapes.
through the perforation and evaluated for evidence of acute or chronic pathologic change such as inflammatory or fibrous thickening, polypoid hypertrophy, ulceration, granulations, and epidermization. Exuberant tissue may be suggestive of neoplastic disease and require biopsy, but the surgeon should keep in mind the possibility of an aberrant carotid, high jugular bulb, or aberrant facial nerve. Also, biopsies and removal of polyps, which may be an essential part of a thorough evaluation of the ear, should be done without disturbing the ossicles, particularly the stapes.
Ossicular pathology can often be identified by inspection, particularly if there is a large perforation or a retracted dimeric membrane in the posterosuperior quadrant of the pars tensa. Common areas of resorptive osteitis are the long process of the incus, the crural arch, and the manubrium. Gentle instrumental manipulations may be helpful in differentiating ossicular mobility or fixation. With large perforations of the pars tensa, the unopposed pull of the tensor tympani muscle often results in medial displacement of the inferior end of the manubrium and occasionally fibrous adhesion to the promontory.
Cholesteatoma of the middle ear may occur alone or in association with cholesteatoma of the epitympanum or mastoid. Cholesteatoma implies the retention of keratin and often mandates surgical correction. It must be differentiated from epidermization, which is also an epidermis-lined region of the middle ear but without retention of keratin and therefore not progressive and in itself not an indication for surgery. Cholesteatoma is often associated with erosion of ossicles, as well as the posterior bony tympanic annulus and the scutum (lateral wall of the epitympanum). Occasionally an attic cholesteatoma may cause erosion of the scutum, resulting in an “autoatticotomy.” Rarely, after invading the mastoid, cholesteatoma will cause resorption of the posterior wall of the external auditory canal, thus exteriorizing itself in what is known as “nature’s radical.”
Attic retraction pockets are retractions of the pars flaccida (Shrapnel’s membrane) into the lateral epitympanic compartment and are caused by chronic or recurring negative pressure in the middle ear. The retraction may consist of a slight medial bowing of the membrane or a deep pocket extending onto the lateral surfaces of the body of incus and head of malleus with varying degrees of resorption of the scutum. If the pocket is clean and dry, it is usually nonprogressive and of no clinical significance. Deeper retractions that collect keratin are so-called symptomatic retraction pockets. Particularly if granulations or suppuration occur, such retractions are often progressive, causing erosion of ossicles and extension into the medial epitympanic compartment, antrum, and mastoid. This condition mandates surgical correction. It is usually not difficult to differentiate a benign nonprogressive retraction pocket from an attic cholesteatoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree