Ocular Trauma
Blunt Trauma
Andrew Mick
THE DISEASE
Pathophysiology
Trauma to the eye from a blunt object results in a concussive shock wave throughout the orbit and globe. The mechanical forces exerted on the globe have the potential to produce damage in all orbital structures.
Common causes include fist fights, airbags, golf balls, baseballs, racquet balls, and bungee cords. Rocks and snowballs are common causes of blunt trauma in children. Greater damage often occurs with smaller objects because the force is more concentrated into the orbital structures. Smaller objects are also able to fit within the protective orbital rim. Larger objects dissipate a large amount of their force into the bones of the face and orbital rim.
The Patient Significant History
Recent eye trauma
Clinical Symptoms
Pain
Sharp and sectoral: Corneal abrasion, laceration of the conjunctiva or lid
Dull aching: Orbital blowout, retrobulbar hemorrhage
Photophobia: Traumatic iritis
Watery discharge
Double vision
Entrapment of extraocular muscles (EOMs)
Damage to controlling cranial nerve
Retrobulbar hemorrhage
Decreased vision
Damage to cornea, lens, retina, or optic nerve
Intraocular bleeding: Hyphema or vitreous hemorrhage
Clinical Signs
Reduced visual acuity
EOM abnormalities
EOM restriction: muscle entrapment secondary to an orbital fracture, damage to controlling cranial nerve, retrobulbar hemorrhage
Lid involvement
Ecchymosis and swelling
Lid lacerations: Injury from a sharp or penetrating object
Crepitus or subcutaneous emphysema: Introduction of air into periocular tissues suggesting orbital blowout fracture
Globe involvement
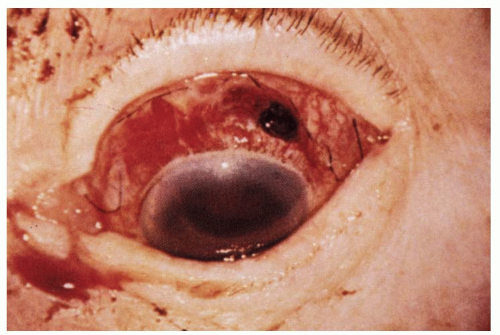
Globe rupture: More likely with trauma from smaller, sharp, high speed objects (Fig. 12-1)
Conjunctival laceration
Subconjunctival hemorrhage
Intraocular pressure (IOP) abnormality
Low IOP: Ruptured globe, retinal detachment, or iritis
High IOP: Intraocular hemorrhage, inflammation, lens subluxation into the anterior chamber, retinal detachment, or angle recession
Corneal involvement
Abrasion: Superficial epithelial layer involved
Laceration: Deeper structures involved without full-thickness wound
Perforation: Full-thickness wound
Anterior chamber involvement
Anterior chamber cell/flare
Hyphema
Abnormal anatomical position of tissues
Grading anterior uveitis
Subclinical: No cells or flare
Trace: Any cells or barely noticeable flare
Grade 1: 5 to 10 cells per highpower field
Grade 2: 11 to 20 cells per highpower field
Grade 3: 21 to 50 cells per highpower field
Grade 4: Cells too numerous to count, fibrinous/plasmoid aqueous
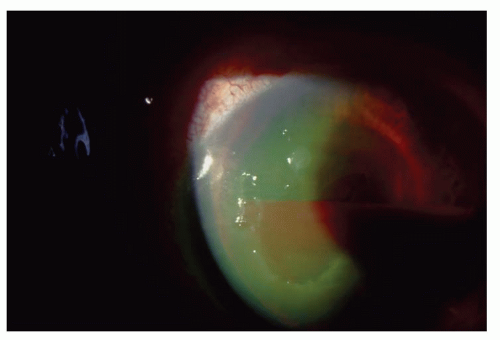
Hyphema (Fig. 12-2)
Microhyphema
No layering of red blood cells in the inferior angle
Visible red blood cells suspended throughout the anterior chamber
General hyphema
Grade I: less than 1/3 of the anterior chamber
Grade II: 1/3 to 1/2 of the anterior chamber
Grade III: greater than 1/2, but less than total
Grade IV: Total (100%) hyphema (a.k.a. 8-ball hyphema)
Iris involvement
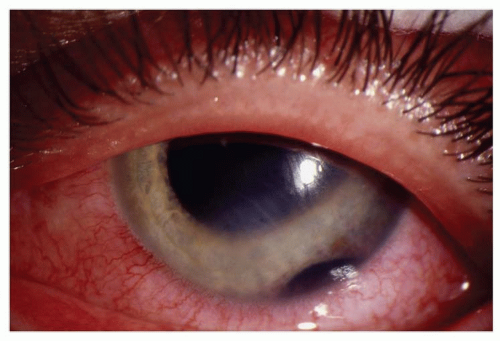
Iridodialysis: Iris disinsertion at scleral spur (Fig. 12-3)
Sphincter or dilator muscle tears
Transillumination defects: Possible site of intraorbital foreign body entrance
Lens involvement
Subluxation
Anterior segment displacement
Opacification: Secondary to blunt trauma or penetrating foreign body
Vitreous involvement
Posterior vitreous detachment
Vitreous hemorrhage: Increases likelihood of associated retinal detachment/tear
Retinal involvement
Retinal breaks or detachments: Increased risk with preexisting retinal breaks
Retinal dialysis: Disinsertion of the sensory retina at the ora serrata
Traumatic macular hole: Tangential traction at the fovea caused by trauma induced initial equatorial expansion and forward displacement of the posterior pole followed by a rebound to its normal anatomical position
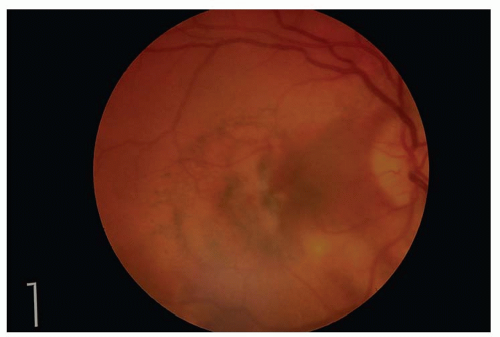
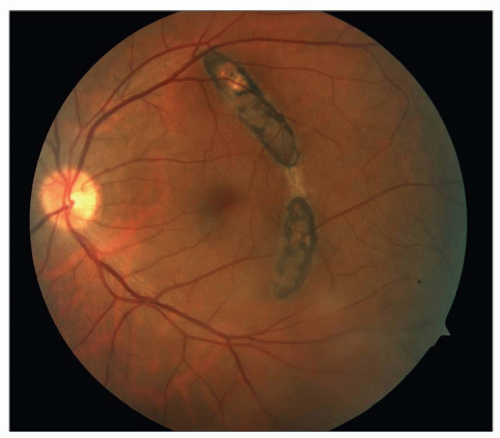
Commotio retinae: Retinal whitening clinically appearing like edema, representing fragmentation of the photoreceptor outer segments (Fig. 12-4)
Choroidal involvement
Choroidal rupture: Breaks of the inner choroid and overlying RPE, often curvilinear and concentric to optic nerve, may be associated with subretinal hemorrhage or serous detachment of the retina, short- and long-term risk of choroidal neovascular membranes (Fig. 12-5)
Chorioretinitis sclopetaria: Choroidal rupture caused by shock waves from high velocity, grazing object passing adjacent to the globe
Optic nerve involvement
Traumatic optic neuropathy: Most common injury site is at orbital apex, afferent pupillary deficit (APD), sluggish or absent pupillary responses, decreased vision, color vision abnormality, visual field defects, acutely may be normal but progressive atrophy develops over several weeks, damage can be direct or indirect
Direct optic nerve damage: Penetrating objects or bone fractures.
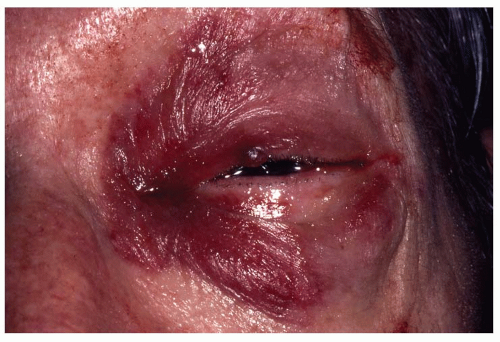
Indirect optic nerve damage: Mechanical shearing, nerve sheath hemorrhage, orbital/retrobulbar hemorrhage, orbital emphysema, ischemia from damaged blood vessels, secondary inflammation (Fig. 12-6)
Optic nerve avulsion: Globe rotated and pulled forward resulting in tearing of the lamina cribrosa and nerve fibers at the disc margin, acute partial ring of hemorrhage surrounding the optic nerve, late fibrous proliferation fills area surrounding avulsion site
Demographics
Blunt trauma is more common in men than women and has a higher prevalence in the younger age groups. Work environments and recreational activities that put eyes at risk of trauma also increase the prevalence of injuries.
Ancillary Tests
Binocular indirect ophthalmoscopy: Evaluate the vitreous, retina, choroid, and optic nerve, scleral indentation contraindicated when hyphema and globe rupture are present
Tonometry: Elevated IOP (intraocular hemorrhage, inflammation, lens subluxation into the anterior chamber, retinal detachment), decreases IOP (globe rupture or retinal detachment)
Gonioscopy: Rule out angle recession or anterior synechiae formation, contraindicated when hyphema and globe rupture are present
Sickle cell screening: Black patients with hyphema
Seidel’s test: Suspicion of penetrating injury to the globe
Forced duction tests: Differentiate between mechanical and paretic EOM deficits
Infraorbital nerve testing: Localized anesthesia signals possible orbital fracture
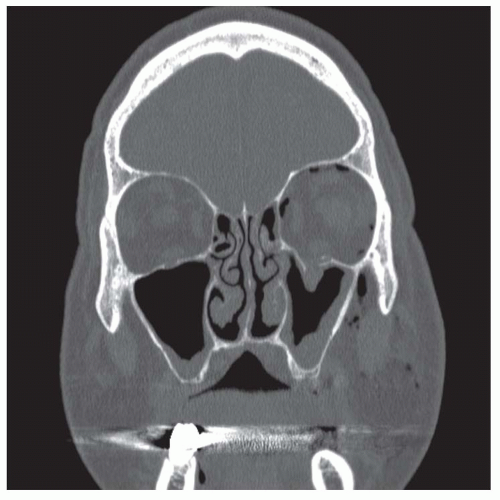
Computed tomography (CT): Detecting subtle orbital fractures or ruptures of the globe, metallic foreign bodies (Fig. 12-7)
Magnetic resonance imaging (MRI): Details soft-tissue damage, must rule out the presence of metallic foreign bodies prior to MRI scanning
Orbital ultrasonography (B-scan): Detecting a ruptured globe or retinal detachment through hazy media or cataract
Fluorescein angiography: Rule out choroidal rupture
The Treatment
Corneal abrasion
Antibiotic coverage
Noncontact lens wearer: Polymyxin B/trimethoprim solution four times a day
Contact lens wearer needs antipseudomonal coverage: besifloxacin 0.6% (Besivance: Bausch and Lomb, Madison, NJ): moxifloxacin 0.5% (Vigamox: Alcon, Ft Worth, TX), gatifloxacin 0.3% (Zymar: Allergan, Irvine, CA), ofloxacin, ciprofloxacin, tobramycin four times a day
Cycloplegia
Cyclopentolate 1% three times a day
Scopolamine 0.25% two times a day
Bandage contact lens
Débridement of loose epithelium
Orbital fracture
Broad-spectrum oral antibiotic therapy
Amoxicillin/clavulanate 500/125 mg two times a day
Cephalexin 250 to 500 mg four times a day
Azithromycin 250 mg twice daily for 1 day and then once daily for 4 days
Cool compresses/ice packs
Appropriate analgesics
Mild pain: Acetaminophen 500 mg every 4 to 6 hours, ibuprofen 400 to 600 mg every 4 to 6 hours, naproxen 250 to 500 mg twice daily
Moderate pain: Acetaminophen with codeine (30 mg codeine) every 6 hours
Severe pain: Acetaminophen (500 mg) with hydrocodone (5 mg) every 4 to 6 hours, ibuprofen (200 mg) with hydrocodone (7.5 mg) every 4 to 6 hours, acetaminophen (325 mg) with oxycodone (10 mg) every 4 to 6 hours
Refer for surgical evaluation immediately
Oculocardiac reflex present: Bradycardia, heart block, nausea, vomiting
Orbital floor fracture with muscle/soft tissue entrapment: High risk of secondary ischemia, especially in children
Early/severe enophthalmos present or severe facial asymmetry
Cerebral spinal fluid rhinorrhea
Large fractures: greater than 1/2 floor or any involving the roof or orbital apex
Refer for surgical evaluation within 1 month
Forced duction testing is positive, or the patient experiences persistent diplopia
There is at greater than 3 mm of persistent enophthalmos present
Observe
Diplopia only in extreme gazes
Minimal cosmetic change
Hyphema
General and microhyphema management guidelines
Bed rest with only bathroom privileges
Elevate head to at least 30 degrees at all times, asleep and awake
No nonsteroidal anti-inflammatory drugs (NSAIDs) or any aspirin-containing medications
Protective eye shield with holes to allow for detection of decreased acuity
Topical steroids: Prednisolone acetate 1% four times a day
Cycloplegic: Scopolamine 0.25% twice daily or atropine 1% daily
Lab tests for sickle cell in black patients
Monitor and treat elevated IOP over 24 mm Hg: IOP may be elevated by red blood cell in the trabecular meshwork, inflammatory debris, peripheral synechiae, or pupillary block from central clot. Elevated IOP can result in damage to the optic nerve and blood staining of the cornea. β-Blockers should be the first line of therapy in the absence of contraindications. Prostaglandin analogs should not be used to avoid adding to the inflammatory response. Miotics increase vascular permeability and increase the risk of posterior synechiae. Carbonic anhydrase inhibitors are contraindicated in sickle cell disease due to acidification of anterior chamber
Daily ocular evaluation: Patient should return immediately if there is a decrease in vision or change in symptoms
Severe hyphema or a noncompliant patient may require hospitalization:
Activity can be more closely monitored, antifibrinolytic agents (aminocaproic acid 50 mg/kg every 4 hours) may be administered. Patients in whom hospitalization should be considered include the following:
Patients with large hyphema: greater than 1/3 anterior chamber
Uncooperative patients
Children: Amblyopia risk with persistent hyphema
Patients who have rebleeding
Patient utilizing anticoagulant therapy
Sickle cell anemia patients
Patients with medically uncontrolled IOP
Reasons to refer hyphema patient for consideration of surgical removal of blood
IOP extremely elevated and not responsive to topical therapy
Grade III or IV hyphema lasting 6 days: Risk of corneal blood staining
Children with persistent hyphema: Amblyopia risk
Traumatic uveitis
Treatment guidelines:
Subclinical: Cycloplegic such as cyclopentolate 1% four times a day
Grade 1: Cycloplegic such as homatropine 5% three times a day, topical steroids such as prednisolone acetate 1% three times a day
Grade 2: Cycloplegic such as homatropine 5% four times a day or scopolamine 0.25% twice a day, topical steroids such as prednisolone acetate 1% four times a day
Grades 3 and 4: Cycloplegic such as atropine 1% once daily or scopolamine 0.25% twice daily, topical steroids such as prednisolone acetate 1% four times a day, consider longer acting steroid-containing ointment nightly such as sulfacetamide/prednisolone (Vasociden: Novartis, Switzerland) gentamicin/prednisolone (Pred-G: Allergan, Irvine, CA) tobramycin/dexamethasone (Tobradex: Alcon, Ft Worth, TX)
Presence of elevated IOP associated with iritis: β-blockers are first line of therapy without contraindications, consider a-agonists and topical carbonic anhydrase inhibitors, avoid prostaglandin analogs as they promote inflammation, no miotics as they increase vascular permeability and risk of posterior synechiae formation
Lens subluxation
Subluxation of the lens into the anterior chamber can cause marked increase in IOP secondary to pupil block. Prior to referral for repositioning or removal of the lens, the following should be done to decrease IOP:
Cyloplegia with appropriate agent
Treat elevated IOP with β-blocker, α-agonist, topical or oral carbonic anhydrase inhibitor (acetazolamide 250 four times a day, 500 mg sequel twice a day, methazolamide 25 mg twice a day), or oral hyperosmotic agent (isosorbide 1 to 3 gm/kg, not metabolized to glucose)
Ruptured globe
Advise patient to not touch or squeeze eyes, position eye shield, advise the patient to not consume any food or water, immediately refer patient to ophthalmic surgeon for surgical repair
Commotio retinae
There is no specific treatment for this condition
Prognosis with uncomplicated commotio retinae is excellent, vision often returns to normal, more extensive damage to the photoreceptors manifests in RPE mottling and atrophy that may result in functional deficits
Retinal tears and detachments
B-scan ultrasonography: When retina cannot be visualized because of media opacity, an APD may be an early indicator of possible detachment, referral for retinopexy or vitreal-retinal surgery as the extent of damage warrants.
Choroidal rupture
There is no specific treatment for this condition
Periodic examination for the development of a choroidal neovascular membrane at the site of RPE disruption that can occur months after the injury or years later, immediate referral to a retinal specialist if choroidal neovascular membrane detected
Optic nerve trauma
There is no specific treatment for this condition
High-dose intravenous steroids administered in the first hours after trauma or surgical decompression of the optic canal have been advocated; treatment therefore will vary with different treating physicians
Corneal Abrasion
Andrew Mick
THE DISEASE
Pathophysiology
The cornea is composed of five distinct layers, including the epithelium, Bowman’s membrane, stroma, Descemet’s membrane, and the endothelium. A defect in the most superficial layer, the epithelium, is classified as a corneal abrasion. Any object that strikes the cornea can produce a superficial abrasion. Common causes are fingernails, tree branches, mascara brushes, and paper cuts.
The Patient Significant History
Trauma from vegetative matter: Increased risk of fungal infection
Contact lens wear: Increased risk of bacterial infection, especially Pseudomonas
Paper cuts or fingernail injuries: Increased risk of recurrent erosion after resolution
High-speed foreign body or associated blunt trauma: Increased risk of penetrating injury
Clinical Symptoms
Pain/foreign body sensation
Lacrimation
Light sensitivity
Clinical Signs
Positive fluorescein staining of defect
Negative Seidel’s test
Mild anterior chamber reaction
Swollen eyelid
The Treatment
Cycloplegia: Cyclopentolate 1% four times a day or homatropine 5% three times a day, or scopolamine 0.25% twice daily
Noncontact lens wearers:
Polymyxin B/trimethoprim solution four times a day
Polymyxin B/bacitracin ointment nightly
Contact lens wearers require anti-Pseudomonas coverage:
Besifloxacin 0.6% (Besivance: Bausch and Lomb, Madison, NJ), moxifloxacin 0.5% (Vigamox: Alcon, Ft Worth, TX), gatifloxacin 0.3% (Zymar: Allergan,
Irvine, CA), ofloxacin, ciprofloxacin, tobramycin four times a day
Ciprofloxacin, tobramycin ointment nightly
Consider tight-fitting low-powered soft bandage contact lens: Decreases lid-cornea interaction and facilitate epithelial healing of large or extremely painful abrasions
Consider topical NSAID to decrease pain: Ketorolac or diclofenac solution
Appropriate analgesics for pain:
Mild pain: Acetaminophen 500 mg every 4 to 6 hours, ibuprofen 400 to 600 mg every 4 to 6 hours, naproxen 250 to 500 mg twice a day
Moderate pain: Acetaminophen with codeine (30 mg codeine) every 6 hours
Severe pain: Acetaminophen (500 mg) with hydrocodone (5 mg) every 4 to 6 hours, ibuprofen (200 mg) with hydrocodone (7.5 mg) every 4 to 6 hours, acetaminophen (325 mg) with oxycodone (10 mg) every 4 to 6 hours
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree