Purpose
To describe the clinical features and management of ocular surface squamous neoplasia (OSSN) after corneal graft.
Design
Retrospective case series of 4 patients.
Methods
Four eyes of 4 patients treated for OSSN after corneal graft in an institutional setting were included. All 4 patients were treated with topical chemotherapy and additionally 1 patient each was treated with excisional biopsy and photodynamic therapy. The main outcome measure was the recurrence of OSSN and the clarity of corneal graft after treatment.
Results
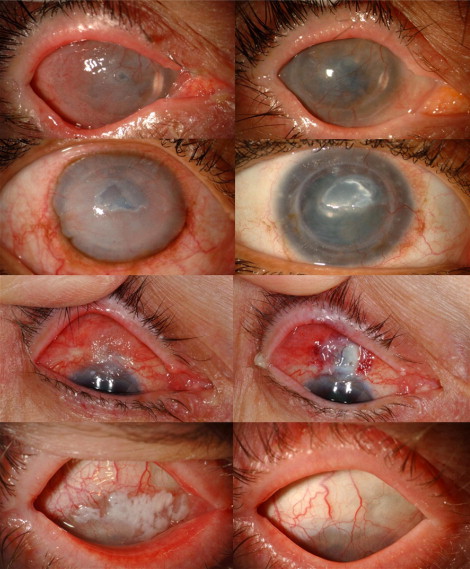
The mean time interval between corneal graft and diagnosis of OSSN was 36 months (range, 2 to 73 months). All 4 eyes were on chronic treatment with topical steroids for a minimum duration of 2 months and 2 eyes had previous herpes keratitis. Misdiagnosis of graft rejection was found in 2 cases. The mean tumor basal diameter was 18 mm (range, 14- to 25-mm) and the tumor involved a mean of 76% of the corneal surface (range, 15% to 90%). Management was successful in all cases using topical mitomycin C (n = 1), topical interferon alpha2b (n = 4), and photodynamic therapy (n = 1). At mean follow-up of 20 months, tumor control was achieved in all cases and all 4 eyes showed chronic graft opacification with vascularization but no intraocular tumor.
Conclusion
Corneal OSSN should be considered in patients using chronic topical steroids for corneal graft. Nonsurgical management with topical chemotherapy or photodynamic therapy can achieve tumor control.
Ocular surface squamous neoplasia (OSSN) has an incidence of 0.03 per 100 000 persons in the United States. OSSN is a spectrum of malignancy ranging from intraepithelial dysplasia to invasive squamous cell carcinoma (SCC). Corneal OSSN is usually an extension of conjunctival squamous neoplasia but, rarely, isolated involvement of the corneal epithelium has been reported. A literature search did not reveal any accounts of corneal OSSN after corneal graft. In this article, we describe the clinical presentation and management of 4 cases of corneal OSSN after corneal graft ( Table , Figure ).
| Features | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Age/gender/race | 61/F/W | 36/F/AA | 74/F/W | 48/M/W |
| History | ||||
| Smoking | No | Yes | No | Yes |
| Systemic immunosuppression | No | No a | No | No |
| Past ocular history | ||||
| History of herpes keratitis | Yes | No | No | Yes |
| Use of chronic topical steroids | Yes | Yes | Yes | Yes |
| Corneal graft | ||||
| Indication for corneal graft | Herpetic scar | Welding burn | Surgical thinning | Herpetic scar |
| Number of grafts | 1 | 2 | 2 | 1 |
| Interval between graft and OSSN (months) | 54 | 15 | 2 | 72 |
| Referring diagnosis | Graft failure | Graft failure | SCC | SCC |
| Treatment summary | INF α2b | Excisional biopsy + INF α2b | INF α2b + PDT | MMC + INF α2b |
| Recurrence | No | No | No | Yes b |
a Patient had known drug abuse.
b Recurrence completely responded to topical interferon alpha2b.
Case Reports
Case 1
A 61-year-old White woman developed blurred vision 5 years after corneal transplantation for postherpetic corneal neovascularization. She was on prednisolone acetate 1% (Omnipred; Alcon Laboratories, Fort Worth, Texas, USA) twice daily for 2 months for presumed graft failure prior to referral. On examination there was a gelatinous vascularized mass covering the entire corneal surface with 360 degrees of limbal involvement and extensive perilimbal conjunctival involvement, measuring 25 mm in diameter. A diagnosis of OSSN was made and the patient was treated with topical interferon alpha2b 1 million international units (IU) 4 times a day (qid). By 8-month follow-up, complete resolution of the OSSN was documented and residual vascularization of the graft was observed. A maintenance dose of interferon alpha2b for 6 additional months was prescribed.
Case 2
A 36-year-old African-American woman with known drug abuse underwent corneal transplantation twice for a welding burn. Seven years later, she developed progressive opacification of the graft and was referred as graft failure. She was on prednisolone acetate drops qid for 12 months. Examination revealed a vascularized opacified graft with squamous neoplasia on the entire corneal surface and a perilimbal rim of conjunctival involvement, measuring 14 mm in diameter. Alcohol corneal epitheliectomy was performed to remove the malignancy, but tight adherence and fibrosis to the underlying cornea led to residual epicorneal tumor. Histopathology confirmed the diagnosis of invasive SCC and the patient was postoperatively treated with topical interferon alpha2b 1 million IU/mL. Five months later, the SCC was completely resolved and residual corneal stromal opacification and vascularization was noted.
Case 3
A 74-year-old White woman was treated elsewhere with deep scleral resection for conjunctival papilloma that resulted in perforation, requiring a tectonic corneal patch graft. Five months after grafting, the patient developed OSSN recurrence over the entire graft. On examination, the superior limbal region of the right eye revealed gelatinous conjunctival tumor on the graft and overlapping the peripheral cornea (2 clock hours), measuring 12 mm in diameter. Topical interferon alpha2b 1 million IU/mL qid was applied for 1 month, showing slow minimal response. Because of the history of the previous scleral perforation, topical mitomycin C (MMC) and further surgery were avoided, so the patient was treated with photodynamic therapy (PDT) using standard dose of 6 mg/m 2 body surface area of verteporfin administered intravenously and with laser irradiation (690 nm) for 83 seconds using a light dose of 50 J/cm 2 . After PDT, the tumor completely resolved and patient underwent repeat tectonic patch graft for corneoscleral thinning.
Case 4
A 48-year-old White man with history of corneal transplant for herpetic keratitis developed blurred vision. Examination revealed a vascularized graft with an extensive 4-mm thick leukoplakic conjunctival tumor involving 360 degrees of limbal tissue and extending to the superior bulbar and tarsal conjunctiva, measuring 20 mm in diameter. The patient was treated with 2 cycles of MMC 0.04% qid for 1 week each with complete resolution. Four years later, he manifested OSSN recurrence and was retreated with 4 cycles of MMC (1 week each), with good response. Small areas of recurrence were evident 3 months after cessation of MMC and the patient was maintained on topical interferon alpha2b qid for 12 months, with complete tumor resolution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


