Chapter 33
OCULAR MANIFESTATIONS OF NONOPHTHALMIC CONDITIONS

Nonmechanical globe injuries may be caused by:
• chemicals (see Chapters 11 and 32);
• temperature;
• radiation (see Chapter 34); or
• mechanical impact elsewhere in the body.
Traumatic events not directly related to the eye rarely lead to ocular lesions; if they do, these are via:
• changes in rheologic conditions;
• hypoxia; or
• a sudden increase of the intravascular pressure.
CONTROVERSY
Because of the great variability of retinal findings and a still incompletely understood response of the retina to distant trauma, the pathomechanism remains under debate.
Three mechanisms have been proposed to explain the resulting fundus findings:
• retinal vascular endothelial cell damage by increased intraluminal pressure;
• damage by emboli (e.g., air, blood products, fat); and
• mechanical forces acting at the vitreoretinal interface.
PURTSCHER’S RETINOPATHY
This is a retinopathy resulting from various etiologies and consisting of:
• marked macular and generalized retinal edema;
• multiple patches of peripapillary superficial retinal whitening;
• intraretinal hemorrhages around the optic disk; and
• disk edema (see Fig. 33–1).
The first case was described in 1868;1 however, no epidemiological data are available.
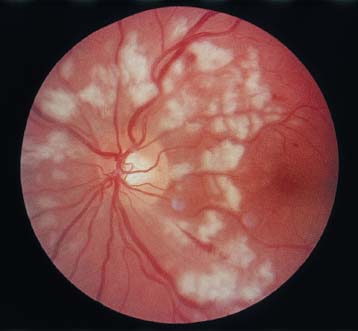
FIGURE 33–1 Purtscher’s retinopathy (see the text for details).
The most typical causes2–6 follow:
• severe head trauma;
• fracture of (long) bones; or
• chest compression (typically in an MVC);
the condition has also been described, however, after:
• concussions of the liver;
• blow to the orbit;
• carotid surgery/angiography; and
• thoracic/renal surgery.
Pathophysiology
Various suggestions have been made with regard to the pathophysiology, such as:
• extravasation from retinal vessels during a sudden increase in the intracranial pressure2;
• reflux venous shock waves produced from intra-thoracic chest compression7;
• fat emboli in retinal arterioles8,9; and
The underlying systemic condition generates various intravascular microparticles that occlude small peripapillary arterioles,5,11–14 with the following mechanisms/materials contributing:
• fat embolization from long bone fractures or acute pancreatitis (due to enzymatic digestion of omental fat)15;
• air emboli from compressive chest injuries15;
• retinal venous wall trauma from venous reflux with endothelial cell swelling and capillary engorgement in the upper body7;
• angiospastic response following a sudden increase in venous pressure6,7;
• local retinal vascular coagulopathy or complement-induced granulocyte aggregation leading to multiple arteriolar occlusions16; and
• fibrin clots, aggregates of platelets and leukocytes.15
A Purtscher-like fundus picture may also occur in lupus erythematosus and at childbirth.11,17
Evaluation
The symptomsa are usually bilateral, although rarely symmetrical, and develop within 4 days.
• Unilateral cases have also been reported.15,18
• Patients complain of decreased vision, often from 20/200 to counting fingers.
• IBO (the peripheral retina is commonly spared):
 numerous white retinal patches or confluent cotton-wool spots around the disk;
numerous white retinal patches or confluent cotton-wool spots around the disk;
 superficial retinal hemorrhages;
superficial retinal hemorrhages;
 serous macular detachments, dilated and tortuous vasculature, and
serous macular detachments, dilated and tortuous vasculature, and
 disk edema.
disk edema.
• FA:
 focal areas of arteriolar obstruction;
focal areas of arteriolar obstruction;
 patchy capillary nonperfusion;
patchy capillary nonperfusion;
 disk edema;
disk edema;
 dye leakage from retinal arterioles, capillaries, and venules;15
dye leakage from retinal arterioles, capillaries, and venules;15
 the choroidal filling may be normal in the acute stages with some blockage of background choroidal fluorescence;
the choroidal filling may be normal in the acute stages with some blockage of background choroidal fluorescence;
 late perivenous staining and/or partial vein obstruction; and
late perivenous staining and/or partial vein obstruction; and
 optic disk edema.
optic disk edema.
Management
Management is by observation.
Complications
Lesions similar to those in Purtscher’s retinopathy have been produced experimentally,b resulting in the clinical picture of Purtscher’s retinopathy. It is thus obvious that the condition may be complicated by vascular occlusions in the retina and on the optic disk, leading to permanent functional impairment.
Prognosis and Outcome
The retinal lesions typically resolve in a few weeks to months. After resolution, the fundus may appear normal, but pigment migration and optic atrophy can occur.4
PEARL… Both the visual acuity and the visual fieldc return to normal in most cases, although if optic atrophy occurs, the vision may be permanently reduced.4
Fundus features in Purtscher-type retinopathy are similar and may appear in many other conditions. History, associated systemic disease, and the interval between injury and onset of visual signs/symptoms may help in the differential diagnosis. Common etiologies include the following.
Fat embolism20 is clinically recognized in up to 5% of patients with long bone fractures,21,22 affects multiple organ systems,23 and may be fatal in 20% of the severe cases.24 Retinal lesions are present in 50–60% of patients, but they are more peripheral.4,7
Acute pancreatitis occurs when digestive enzymes released from the inflamed pancreas degrade omental fat, liberating into the general circulation free fat emboli that may eventually lodge in the retinal circulation.15 A complement cascade may be activated by the release of pancreatic proteases, leading to leukoembolic retinal arteriolar occlusion.16
Compression cyanosis (or traumatic asphyxia) is accompanied by bluish discoloration of the chest, neck, face, and upper extremities.
Air embolization is a rare complication of chest/ jugular vein surgery/injury. Distinguishing fundus features include a uniformly gray appearance of the fundus, a pale optic nerve, and intra-arterial air.d
Hydrostatic pressure syndrome occurs when a person is ejected from an aircraft traveling at very high speed. The high decelerating forces drive blood toward the head and create mental confusion, temporary loss of vision, periocular edema, ecchymosis of the lids, and subconjunctival and retinal hemorrhage.7
The nonophthalmologist should be aware of sight-threatening complications even in the absence of direct ocular involvement.
PEARL… If the victim is unconscious or complains about visual loss during the first 4 days after severe trauma, an ophthalmologist should be called for consultation. The findings should be precisely documented and photographed because the patient may later seek compensation for the injury (see Chapter 7).
WHIPLASH SYNDROME
An energy transfer to the neck and head occurs via acceleration/deceleration; it is most common in rear-end collision MVCs25 and may lead to a variety of clinical manifestations (whiplash-associated disorders). The predominant symptom is pain and discomfort, frequently in the absence of pathology on inspection or radiological investigation. There may be concussional injury to the brain.
Epidemiology and Prevention
In one study,25 the driver-specific incidence rate was 96 per 100,000 licensed drivers per year. It varies with population density.e
Pathophysiology
A violent flexion is immediately followed by an extension of the neck, which may cause a mechanical injury to the sympathetic nerves.
PEARL… The visual disturbance in whiplash syndrome may be caused by direct injury to the cervical/carotid artery or by an accompanying Purtscher type of injury; a true retinal excavation26 may also exist, and the whiplash maculopathy may be related to vitreomacular traction.
Evaluation
The patients may have a wide range of complaints.
• The most common presenting symptoms are neck pain (≤100%) and headache (54–66%).25
• Horner’s syndromef may be the most common ocular manifestation.4
• Visual complaints are reported in 8 to 26%.25,27
 The reduction in visual acuity is rather acute but usually not worse than 20/30. The symptoms are bilateral and resolve over a period of a few days.
The reduction in visual acuity is rather acute but usually not worse than 20/30. The symptoms are bilateral and resolve over a period of a few days.
• On biomicroscopic examination, there is a gray swelling of the fovea. A crater-like depression less than 100 µm in diameter with slight RPE disturbance may remain unchanged even when the symptoms resolve.26
• FA may be normal or may show a tiny focal area of hyperfluorescence.26
Management
There is no known treatment.
Complications
An accompanying concussional injury to the brain may cause temporary palsy of the cranial nerves with diplopia.4
Prognosis and Outcome
The visual acuity usually, although not always, returns to normal. A similar clinical appearance and course may be seen after contusion and solar retinopathy (see Chapter 34).11
The nonophthalmologist should be aware of sight-threatening complications even in the absence of direct ocular involvement. If the victim complains about visual loss after a whiplash injury, an ophthalmologist should be called for consultation. Accurate documentation is important.
SHAKEN BABYg SYNDROME
The 15% mortality rate underscores the importance of recognizing this form of child abuse.29
Epidemiology and Prevention
In central Europe, 3.5% of the parents confessed to having used so much violence on their children that it might have resulted in severe injury; 10% of traumatized children admitted to a hospital show evidence of physical violence.30
In a single year, 1120 instances of child abuse were registered by the police in western Germanyh; the estimated number of cases was between 20,000 and 400,000.30
• Two thirds of the abused children are babies.
• The typical victim is a male infant, younger than 6 months of age, who is alone with the perpetrator at the time of the injury.31
• The incidence is unrelated to race, gender, socioeconomic status, or education.31
• The presenting sign is eye related in 4 to 6% of the cases.
• Whereas after accidental head injuries nearly all babiesi have normal funduscopic examinations, most babies with nonaccidental head injuries show varying degrees of retinal hemorrhages.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


