CHAPTER 38 Non-penetrating surgery
Introduction
Trabeculectomy is the procedure of choice for glaucoma surgery thanks to its high success rate. Nevertheless, the procedure can be associated with major intraoperative and postoperative complications. In order to define a safer and more effective operation, during the last 20 years many alternatives to trabeculectomy have been proposed. Over the years, a growing body of evidence suggests that ‘non-penetrating glaucoma surgery’ (NPGS) is successful at lowering intraocular pressure and can be considered as a surgical option for glaucoma1,2. NPGS is represented by ‘deep sclerectomy’(DS) and by ‘Viscocanalostomy’(VC) (which was introduced by R. Stegmann in the early 1990); they are based on original studies by Krasnov (1972) and Zimmerman (1984) on ‘non-penetrating trabeculectomy’. Similarly, both procedures aim to lower intraocular pressure (IOP) by draining aqueous humor from the anterior chamber not through a patent scleral opening, but by slow percolation through the inner trabecular meshwork and/or Descemet’s membrane (the ‘sclerodescemetic membrane’) (Fig. 38.1). This avoids sudden IOP fall, hypotony, and a flat anterior chamber. The absence of anterior chamber opening and iridectomy limits inflammation and the risk of cataract and intraocular infection. Compared with deep sclerectomy, viscocanalostomy has significant advantages; it aims not only to be non-penetrating like deep sclerectomy, but also to restore the physiological outflow pathway, thus avoiding any external filtration. This would make the success of the procedure independent of conjunctival or episcleral scarring, a leading cause of failure in trabeculectomy, with fewer indications for wound healing modulation. Moreover, the absence of a filtering bleb avoids related ocular discomfort. In addition, the procedure can be carried out in any quadrant. A technical variation of viscocanalostomy, was recently introduced, named ‘canaloplasty’ (CP), aimed at a better and controlled dilation of Schlemm’s canal.
Deep sclerectomy
Fundamental principles
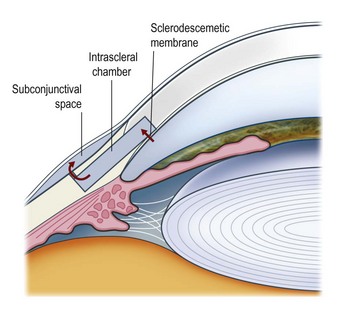
Deep sclerectomy (DS) aims to reduce intraocular pressure by external filtration of aqueous humor. Unlike trabeculectomy, aqueous exits the eye not through a patent hole, but by slow passage through the ‘sclerodescemetic membrane’ formed by the internal portion of the posterior and anterior trabecular meshwork and by the adjacent Descemet’s membrane. The membrane is created by removing the inner wall of Schlemm’s canal and juxtacanalicular trabeculum (sites of the increased outflow resistance in glaucoma) to expos the anterior trabecular meshwork and Descemet’s membrane. Percolating from the anterior chamber, aqueous fills an intrascleral ‘lake’ or ‘decompression chamber’, from where it drains into the subconjunctival space and/or is partially reabsorbed into the suprachoroidal space (Fig. 38.2).
Indications for surgery
Based on its high safety profile and on its mechanism of action, deep sclerectomy is indicated in primary open angle, pseudoexfoliative, and pigmentary glaucomas. Being non-penetrating, it can be useful particularly in aphakic eyes with vitreous in the anterior chamber, or in-patients where a sudden drop in IOP or long-lasting hypotony should be avoided, such as eyes with uncontrolled high pressure, eyes with high myopia, or even eyes with very advanced glaucoma. The procedure was also found to be effective in uveitic glaucoma3.
Operation technique
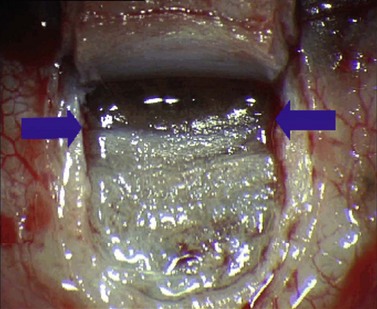
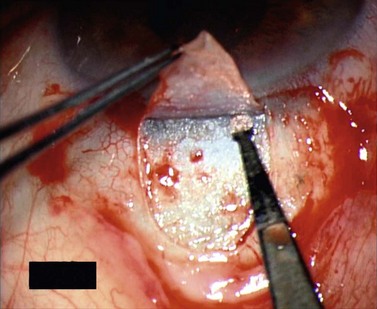
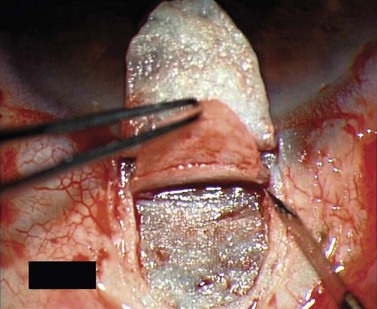
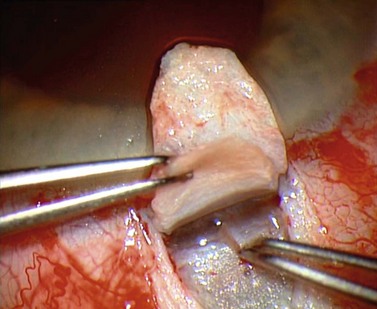
For good exposure of the surgical area, place a traction suture in the cornea or under the superior rectus. Raise a fornix-based conjunctival flap in the upper quadrant and lightly cauterize superficial blood vessels carefully, so as to preserve collector channels and to avoid scleral shrinkage and damage to Schlemm’s canal. Dissect a 5 × 5 mm superficial flap, approximately ⅓ scleral thickness, and advance anteriorly into clear cornea for about 1–1.5 mm (Fig. 38.3). To make the deep sclerokeratectomy, dissect a second 4 × 4 mm deep scleral flap. The dissection should be just deep enough to leave a thin layer of sclera (50–100 µm) over the choroid and the ciliary body with a dark reflex just visible below the scleral fibers. Start the deep sclerectomy posteriorly and carry it anteriorly until Schlemm’s canal is deroofed (Fig. 38.4). Advance the dissection into clear cornea to create the sclerodescemetic membrane, the site of aqueous filtration. Deepen the two lateral radial cuts and advance into clear cornea without touching the anterior trabeculum or Descemet’s membrane. By gently pulling the deep scleral flap with forceps and with counter traction on the bed of the canal using a triangular cellulose sponge, detach the anterior portion of the deep flap from the anterior trabecular meshwork and from Descemet’s membrane. Advance this 1–1.5 mm anteriorly. At this stage, there should be aqueous percolation through the membrane. To optimize outflow, peel the internal wall of Schlemm’s canal (the juxta-canalicular trabeculum and the canal endothelium) by grabbing it with thin forceps (‘external trabeculectomy’) (Fig. 38.5). This removes a homogeneous external trabecular membrane in one coherent plane and allows aqueous humor to egress through the remaining inner trabecular layers. Excise the deep flap by cutting it anteriorly.
To maintain the created space (‘intrascleral lake’ or ‘decompression chamber’) and to avoid postoperative scarring, different implants are used4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree