Imaging evaluation of laryngeal pathology has been revolutionized with the development of multidetector CT. The thinner axial CT slices result in improved contrast resolution and the ability to perform multiplanar reformations without breathing or swallowing artifacts. This article reviews the use of multidetector CT in the evaluation of laryngeal trauma and in common and uncommon inflammatory laryngeal diseases. The imaging evaluation of hoarseness and recurrent laryngeal nerve paralysis is reviewed with emphasis on where MRI or positron emission tomography can offer additional diagnostic information.
The first article in this issue discusses the merits and pitfalls of CT and MRI. CT has long been favored by radiologists for laryngeal imaging because the rapidity of image acquisition minimizes breathing and swallowing artifacts that may make MRI images unreadable. Patients who are unable to remain still in the supine position because of concomitant chronic lung disease or excessive pharyngeal secretions also are more readily evaluated with CT. MRI has been reserved largely for problem-solving in laryngeal tumor cases, particularly with squamous cell carcinoma, because multiplanar imaging is possible, and MRI is a more sensitive tool for the evaluation of cartilaginous invasion. This preference may be changing with further evolution of multidetector CT (MDCT) scanners, which are able to obtain thinner axial slices more rapidly, affording better contrast and spatial resolution and allowing multiplanar evaluation of the neck. This article aims to demonstrate the utility of cross-sectional imaging for evaluation of non-neoplastic laryngeal pathology, with an emphasis on CT, because this is the study of choice for non-oncologic laryngeal imaging.
Laryngeal imaging: techniques and protocols
CT imaging techniques
Using 64-slice MDCT scanners, the laryngeal protocol at the University of California, San Francisco, consists of axial-plane 2.5-mm images from the skull base to the thoracic inlet during quiet respiration (not breath-hold). When a history of hoarseness or left recurrent laryngeal nerve paralysis is given, axial imaging continues to the level of the left pulmonary artery in the thorax. Intravenous iodinated contrast (100 cm 3 ) is administered routinely unless there is a known contrast allergy or the patient has poor renal function. As is true elsewhere in the neck, contrast is considered very important for the detection, delineation, and characterization of masses, the differentiation of nodes from vessels, and the determination of vascular patency. This 64-slice MDCT protocol takes approximately 8 to 10 seconds to perform after an initial postinjection delay of 40 to 60 seconds to allow contrast to reach the neck veins and for soft tissues to enhance. The author and colleagues routinely reconstruct coronal and sagittal images from this data at 1.5-mm intervals. The reformations through the neck may be helpful in verifying involvement of true vocal cords or subglottic tissues with supraglottic processes.
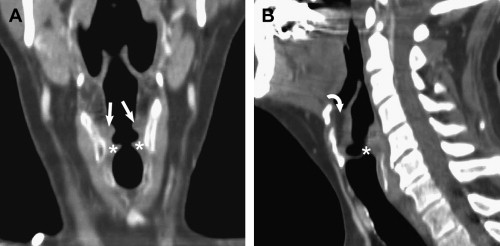
Rapid, thin-slice imaging with MDCT also allows the use of additional techniques, such as the modified Valhalla maneuver and phonation, to show laryngeal anatomic detail better. It also allows three-dimensional (3D) reconstruction formats such as volume and surface rendering and virtual laryngoscopy that may offer improved evaluation of the larynx. The modified Valhalla technique (exhalation against a closed glottis or blowing through a straw) or the phonation technique (the patient exhales with a constant “eeeeee” sound during image acquisition) may be used to expand the pyriform sinuses and distend the laryngeal ventricles, thus allowing better delineation of these structures . These techniques may be performed either at the time of whole-neck image acquisition or as an additional protocol through the larynx alone, after completion of a neck study. Some authors believe that these techniques have little additive value and that at times the images may add confusion . The author and colleagues also have had difficulty in imaging patients who are unable to sustain the 8 to 10 seconds of phonation or to follow the technician’s instructions adequately. They have, however, used the phonation technique with some success in demonstrating normal anatomy and delineating tumor extent ( Fig. 1 ).
To obtain 3D volume-rendered or virtual laryngoscopy images, one of these larynx-distending techniques must be used, and thinner slices must be obtained with a further increase in patient radiation . Such virtual laryngoscopy images can allow evaluation of the larynx without sedation and provide views below areas of obstruction; however, virtual laryngoscopy is not suggested as a replacement for direct laryngoscopy, nor is there evidence that it should be used for routine laryngeal CT imaging . The 3D volume-rendered and virtual laryngoscopy images can look quite spectacular, nonetheless ( Figs. 2 and 3 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


