CHAPTER 41 New advances in glaucoma surgery
Introduction
Trabeculectomy, since its introduction in 1968 by Cairns1, has been the most widely performed glaucoma incisional procedure and continues today to be considered by many the gold standard by which all other surgical glaucoma procedures are measured. Because of the low attainable intraocular pressure (IOP) levels, and the relative simplicity of performing the actual procedure, trabeculectomy rapidly gained acceptance. However, despite its advantages, a large number of potentially visually devastating complications may result, in both the short and long term. These have been well documented in the literature and include, but are not limited to, infections (blebitis, endophthalmitis), bleb-related complications (encapsulation, fibrosis, leakage, dysesthesia, overhang, corneal dellen), hypotony and its associated complications (shallow/flat anterior chamber, maculopathy, overfiltration), as well as others such as aqueous misdirection syndrome, accelerated cataract formation, and endothelial cell loss2.
Another procedure which has continued to gain acceptance, especially in complex eyes with previous surgical failure and increasingly also as a primary procedure, are the glaucoma drainage devices (GDDs). The first such device was introduced by Molteno in the 1960s3. Other similar models followed including the Ahmed valve4, the Krupin eye disc5, and the Baerveldt drainage device6. These long tube shunt devices were designed to carry aqueous from the anterior chamber to a reservoir 10–12 millimeters (mm) posterior to the limbus, taking advantage of the larger posterior potential subconjunctival space, as well as theoretically avoiding the less metabolically active limbal zone where it may be more likely for a bleb to fibrose and fail. However, like trabeculectomy, these procedures too have an extensive complication profile. Most significantly, the risk of hypotony and suprachoroidal hemorrhage have led to the design or performance of modern day GDD surgery to emphasize flow control with either a valved plate mechanism such as the Ahmed, or partial and sometimes complete ligature of the tube with suture material. Despite these measures, hypotony and its associated complications remain a risk for the patient undergoing tube shunt surgery. In addition to these risks, GDD surgery has its own unique set of postoperative risks, including tube or plate exposure, tube occlusion, tube-related corneal endothelial cell loss even with properly positioned tubes, ptosis, and diplopia.
The Ex-PRESS shunt
The Ex-PRESS mini glaucoma shunt, like trabeculectomy, is designed to provide aqueous humor with an outlet into the subconjunctival space resulting in a bleb. The stainless steel device has a rounded tip in the anterior chamber to drain aqueous humor through the shaft trans-sclerally to end in a footplate which rests under a scleral flap and prevents migration of the shunt anteriorly. A spur on the anterior chamber side of the device prevents device extrusion. Several designs of the device offer slight modifications of the footplate or tip. While initially the device was implanted subconjunctivally without a scleral flap, complication rates were unacceptably high, with hypotony, shunt migration, and conjunctival erosion7. Later, the shunt was placed under a trabeculectomy-style scleral flap, which improved the safety profile of the device.
Technique
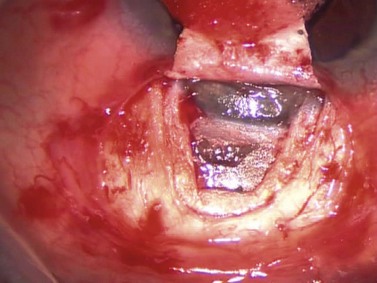
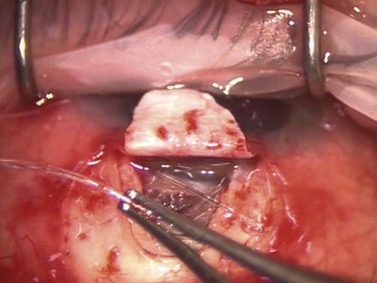
As in standard trabeculectomy, a conjunctival peritomy is followed by a scleral flap dissected forward so as to provide a clear view of the scleral spur. The dimensions of this flap should be slightly larger than that in standard trabeculectomy so as to cover fully the footplate of the device. Once the glistening white fibers of the scleral spur are visible, the anterior chamber should be pressurized with an ophthalmic viscosurgical device (OVD) via a paracentesis incision, or a cataract incision, if part of a combined procedure. An entry is made into the anterior chamber at the level of the scleral spur using either a sapphire blade, manufactured by Optonol, or a 25-gauge hypodermic needle (Fig. 41.1). The angle of entry into the anterior chamber must be parallel to the iris plane. An entry angled perpendicular to the spur will result in an excessively posterior shunt impinging on iris, perhaps with tip occlusion, corectopia, and photophobia. An entry angled excessively anteriorly will rest the tip near the corneal endothelium. The ideal position for the shunt is to be parallel to the iris surface (Fig. 41.2). Once the shunt is in a satisfactory position, the OVD may be aspirated with a dry technique and the anterior chamber pressurized with balanced saline solution (BSS). The scleral flap is sutured at its corners similar to a standard trabeculectomy; flow can be assessed with a surgical sponge. With suture tension adjusted to attain satisfactory flow, the conjunctiva is closed in a watertight fashion.
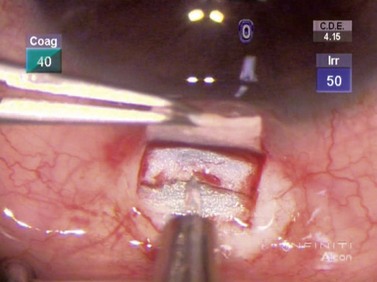
Fig. 41.1 A sapphire blade is shown about to enter the anterior chamber at the level of the scleral spur.
Discussion
Several studies have demonstrated effective IOP lowering and decreased medication usage with the Ex-PRESS shunt8,9 and more recently, prospective and retrospective studies have found the device to be comparable with conventional trabeculectomy10,11. In traditional trabeculectomy surgery, aqueous egress from the anterior chamber is regulated by the size of the ostium and of the scleral flap as well as suture tension. Although the Ex-PRESS shunt depends also on subconjunctival flow to lower IOP, it provides a consistent and reproducible ostium size, which may be challenging with a standard trabeculectomy punch. As well, without a large ostium, the Ex-PRESS shunt is inserted through a small entry into the anterior chamber improving anterior chamber stability during entry, as well as obviating the need for a surgical iridectomy. While in trabeculectomy, a surgical iridectomy may also be avoided, the creation of the large punch opening, combined with a shallowing of the anterior chamber, commonly results in iris presenting at the trabeculectomy site requiring a surgical iridectomy. This is notable in patients with narrow angles or shallow anterior chambers where enhanced anterior chamber stability may be more important. In our experience the Ex-PRESS shunt is well suited for narrow angle patients who require filtration surgery.
Non-penetrating Schlemm’s canaloplasty
Technique
The dissection is continued forward into peripheral clear cornea for approximately 2 mm exposing the trabeculo-Descemet window (TDW) (Fig. 41.3). Extreme care must be taken with the TDW as it easily ruptures, even with a wet surgical sponge. Once the TDW has been exposed, the deep flap is excised. The microcatheter is introduced into one of the cut ends of the canal and under fiberoptic illumination guidance is advanced carefully around the entire circumference until the tip emerges from the opposite cut end (Fig. 41.4). Once this has been achieved a suture, typically 10-0 Prolene, which the authors prefer, is tied to the distal end with two loose ends tied to the loop. The microcatheter is retracted 360° in the opposite direction, while an assistant injects a metered dose of OVD into the canal. Once fully retracted, the suture is cut from the microcatheter and the result is two loose suture ends emerging from each cut end of Schlemm’s canal. These ends are carefully corresponded and tied down in a slipknot fashion over the TDW. As the suture is tensioned, an inward dimpling of the TDW should be visualized, occasionally accompanied by an increase in aqueous humor percolation seen to emerge through the TDW (Fig. 41.5). The second suture is then tied down in a similar fashion. The superficial scleral flap is replaced and sutured down in a watertight fashion with typically five interrupted sutures, and finally followed by watertight conjunctival closure.
Discussion
The goal of canaloplasty is to restore or augment the outflow of aqueous via the conventional pathway by suture mediated distension of Schlemm’s canal. The tensioned suture attempts to reverse the process of canal collapse in glaucomatous eyes and thus to lower IOP. In the longest follow-up studies to date, at 2 years postoperatively, the mean IOP in patients undergoing canaloplasty alone was reduced from 23.3 mmHg to 16.3 mmHg and the mean number of medications used was reduced from 2.0 to 0.6. In patients undergoing combined cataract surgery with canaloplasty, the mean IOP was reduced from 23.1 mmHg to 13.4 mmHg and medication numbers decreased from 1.7 to 0.212. Suture tension has been shown in studies to be critical to obtain IOP lowering, with greater distension correlating with greater lowering of IOP13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 scleral thickness. A deep scleral flap is created, approximately 1 mm within the borders of the superficial flap and the depth such that approximately 100 µm of sclera remain in the bed of the dissection. As this dissection is carried forward, the glistening white fibers of the scleral spur should appear in the bed of the dissection and, immediately anterior to this, the canal of Schlemm is seen to split open. The dissection must be carried forward at a consistent depth: dissecting excessively deeply will penetrate the eye; conversely superficial dissection will pass over the canal without accessing it.
scleral thickness. A deep scleral flap is created, approximately 1 mm within the borders of the superficial flap and the depth such that approximately 100 µm of sclera remain in the bed of the dissection. As this dissection is carried forward, the glistening white fibers of the scleral spur should appear in the bed of the dissection and, immediately anterior to this, the canal of Schlemm is seen to split open. The dissection must be carried forward at a consistent depth: dissecting excessively deeply will penetrate the eye; conversely superficial dissection will pass over the canal without accessing it.