1 My favorite definition of tinnitus is from McFadden (1982). Tinnitus • Is a perception of sound (it must be heard) • Is involuntary (not produced intentionally) • Originates in the head (not hearing or overly sensitive to an external sound) I would add that the patient’s reaction should be considered. It is helpful to distinguish • Tinnitus that is problematic from that which is not (Coles, 1987) • How often the tinnitus occurs and how long an episode is (e.g., whether it occurs once a month for 10 seconds or is present daily) Tinnitus has been classified in several ways, such as its presumed site of generation and whether it is audible to someone other than the patient (objective tinnitus) or the patient alone (subjective tinnitus). An objective tinnitus, heard by the examiner, may be of middle ear origin or a spontaneous otoacoustic emission arising from the sensorineural system. Therefore, the terms subjective and objective are not helpful in understanding or treating tinnitus. Therefore, tinnitus can be classified in a manner analogous to hearing loss according to site of injury or generation (Tyler and Babin, 1986); that is, whether it is middle ear, sensorineural, or central tinnitus. The treatments described in this book are applicable to all classes of tinnitus. A thorough physical examination and treatment of identified ailments, when possible, are important first steps in treating a patient with tinnitus. The overall impact of tinnitus on a patient is influenced by the characteristics of tinnitus and of that particular patient (Dauman and Tyler, 1992). For example, I believe that tinnitus is more likely to be annoying if it is louder or has a screeching quality. Some authors have incorrectly suggested that psychoacoustic factors are unimportant or unrelated to tinnitus annoyance. Psychoacoustic factors are indeed relevant, although they are only one thing to consider in understanding the effect tinnitus has on a patient. An absence of high correlation between loudness and annoyance does not mean that loudness is not important. Stouffer and Tyler (1990) concluded that patients with soft tinnitus are not under as much stress as those who report a loud tinnitus. Also, patients who are under stress or have not had adequate sleep find the tinnitus more annoying. Tinnitus is not a personality disorder, but psychological factors are involved in the development and maintenance of this problem (see, e.g., Fowler and Fowler, 1955). Although patients with severe tinnitus can have clinical depression, in my experience serious psychological problems are rare among most tinnitus patients. Very few of us, after all, would not be bothered at all if we constantly heard an unwanted sound that we had no control over. Neurophysiological models can be considered from many different aspects. In the normal auditory system, increases in spontaneous activity evoked by acoustic stimuli are thought to be the basis for sound perception. Therefore, neurophysiological models have logically nominated an increase in spontaneous activity in the absence of acoustic stimulation as the mechanism of tinnitus. Wherever the site of origin, most probably this must be transmitted to and result in an increased spontaneous rate in the auditory cortex. Table 1–1 reviews a few of the neurophysiological models that have been proposed over the years (for reviews, see Cacace, 2003; Eggermont, 2000; Eggermont and Roberts, 2004; Jastreboff, 1990; Salvi, Lockwood, and Burkard, 2000; Vernon and Moeller, 1995). Some of these are specific to precise anatomic or physiological sites; others are more general models referring to processing principles.
Neurophysiological Models, Psychological Models, and Treatments for Tinnitus
What Is Tinnitus?
Neurophysiological Models of Tinnitus
| Kiang, Moxon, and Levine (1970) | Edge between normal and absent hair cells and subsequent neural activity |
| Tonndorf (1981) | Decoupling of stereocilia between the hair cells and tectorial membrane |
| Moeller (1984) Eggermont (1984) | Cross-talk (interneural synchrony) between nerve fibers |
| Hazell (1987) | Tinnitus a result of automatic gain control system of central nervous system (e.g., normally increasing the sensitivity in quiet), linked to outer hair cells |
| Penner and Bilger (1989) | Spontaneous otoacoustic emissions |
| Jastreboff (1990) | Discordant inner and outer hair cell damage (damaged outer hair cells with reasonably intact inner hair cells) |
| Salvi et al (1996, 2000) | Increase in central neurons tuned to similar frequencies following reorganization of peripheral hearing loss |
| Kaltenbach et al (2001) | Hyperactivity of dorsal cochlear nucleus |
In general, many of these models are insightful and clever. For models to be useful, they should be testable or should lead to a broader understanding and eventually a testable hypothesis.
I believe that, whatever the initial source of tinnitus, it must be perceived in the auditory cortex (see Tyler, 1981, p. 136). Broadly, there are three different ways that the mechanism of tinnitus can be coded in the auditory cortex:
• Increased spontaneous activity fed by increase or decrease in activity or edge in activity (Kiang et al, 1970)
• Cross-fiber correlation with normal or increased spontaneous activity (Eggermont, 1984; Moeller, 1984)
• More fibers with similar best frequency following hearing loss–induced auditory plasticity (Salvi et al, 1996, 2000)
Fig. 1–1 shows a schematic representation of how we hear, interpret, and react to sounds. Sound is transformed from acoustic to electrical information in the cochlea. It is transmitted through the brainstem to the auditory centers of the brain within the temporal lobe of each hemisphere. Other parts of the brain are involved in our memory for sounds and our emotional reaction to them. Such neurophysiological models of hearing have existed for decades and were applied to tinnitus as early as 1988 (Goodey, 1988). Although the mechanism responsible for the source of tinnitus initiation may arise anywhere, its representation in the nervous system must be transmitted to the brain. Wilson (1987, pp. 30, 31) suggested that tinnitus is coded in the auditory cortex “by virtue of the pattern of activity over many cells.” Like normal sounds, any reactions patients have to their tinnitus must involve other regions of the brain, such as the amygdala and the autonomic nervous system. Hallam et al (1984, p. 44) discussed “neurophysiological models of habituation” and their importance in understanding and treating the emotional components of tinnitus. This model was widely accepted at the time (e.g., Hazell et al, 1985, p. 74).
Noise-induced hearing loss, one of the most common causes of tinnitus, is known to inflict cochlear damage. Early studies of noise-induced hearing loss emphasized that outer hair cells are affected first and then inner hair cells (e.g., Liberman and Dodds, 1984). However, I have argued that tinnitus must also intimately involve the brainstem and cortex (Tyler, 1981, p. 136). This was based on several observations, including that
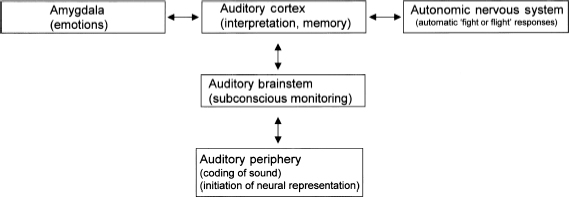
Figure 1–1 A general schematic representation of the process of hearing, interpreting, and reacting to sounds. The mechanism for the initiation of tinnitus may arise anywhere, but its representation eventually occurs in the auditory cortex. Any emotional responses must involve the amygdala and the autonomic nervous system.
• Sectioning the auditory nerve is often ineffective in reducing tinnitus.
• Masking can be just as effective in the ear ipsilateral to the tinnitus as in the ear contralateral to the tinnitus (e.g., Tyler and Conrad-Armes, 1984).
• One can observe that a person who is convinced about hearing tinnitus in the right ear can suddenly hear the tinnitus in the left ear when the right ear tinnitus is masked.
Coles (1987) also noted, as have many others since, that disorders of the central auditory pathways can cause tinnitus.
It is of interest, and perhaps a puzzle, that tinnitus can be influenced by other neurophysiological systems (for recent reviews, see Cacace, 2003, 2004; Levine et al, 2003). For example, in some patients tinnitus can be altered by touches to the hand, jaw movement, pressure to the head, and changes in eye gaze.
Of course, because tinnitus can provoke emotional reactions, other neurophysiological systems that are responsible for emotions must also be involved, including the autonomic nervous system and the amygdala. Both Hallam et al (1984) and Slater and Terry (1987) described how the autonomic nervous system is involved in tinnitus. This unconscious involuntary control system is for “fight or flight.” The sympathetic system sets up the body for action, and the parasympathetic system operates after the extra alertness is past, to bring the body from its “highly aroused state to its normal state” (Slater and Terry, 1987, p. 177). The authors emphasized how the “dangers” sensed are typically stress related, and reviewed in great deal the neurophysiological responses. They suggested coping strategies (e.g., relaxation techniques) as a treatment for the “inappropriate” autonomic response of tinnitus patients. It has been known for decades that the limbic system of the brain is involved whenever emotions are triggered (for reviews, see LeDoux, 1994; Mega et al, 1997). Jastreboff (1990) pointed out that the limbic system therefore must be involved in tinnitus patients who have emotional reactions. Cacace (2003) prefers the term amygdala to limbic system.
I like the way Goodey (1988, p. 84) explains tinnitus to his patients: “Too few messages are passing through the ear to keep the hearing nerve busy and … especially in quiet conditions, the electrically active nerve generates its own messages which are heard as tinnitus.”
Psychological Models of Tinnitus
Physiological and psychological models are inherently linked. One cannot have a change in thinking or behaving without some neurophysiological correlate. Studies, and related conceptual frameworks, that focus on thinking and behaving can be considered psychological. Table 1–2 reviews some psychological frameworks for considering tinnitus treatment.
These models are certainly not mutually exclusive. For example, Hallam et al (1984), in their habituation model, noted that an organism needs to analyze (or attend to) new and potentially important stimuli. How we think about tinnitus influences our inclination to attend to it. External events can reinforce or inhibit our behavior. Learning theory, particularly classical conditioning, has been proposed as an important factor in the reaction to tinnitus (e.g., Jastreboff, 2000; McKenna, 2004). Hallam et al (1984, p. 44) suggested that “habituation can be delayed by intense, aversive and unpredictable stimuli to which affective significance has been attached by learning.”
| Cognitive | Have developed inappropriate ways of thinking about tinnitus | Sweetow (1984, 1986) Andersson and Kaldo (Chapter 8) Hallam and McKenna (Chapter 6) |
| Habituation | Bothersome tinnitus is failure to habituate | Hallam et al (1984) Hallam (1989) Hallam and McKenna (Chapter 6) |
| Attention | Failure to shift attention away from tinnitus | Hallam et al (1984) Hallam (1989) Hallam and McKenna (Chapter 6) |
| Learning | Responses to tinnitus are learned | Jastreboff and Hazell (1993) Bartnik and Skarżyński (Chapter 10) also McKenna (2004), Hallam et al (1984) |
Categories of Tinnitus Treatments
We can categorize tinnitus treatments in two ways. First, a treatment can focus on the tinnitus directly, reducing its magnitude or eliminating it completely. This can be accomplished by medications (e.g., Dobie, 1999; Murai et al, 1992) or electrical suppression (e.g., Dauman, 2000; Dobie et al, 1986; Quaranta et al, 2004; Rubinstein and Tyler, 2004; Zwolan et al, 1992). Although there have been important gains in both of these approaches, no clinical protocol is currently available, and they will not be reviewed in this book.
Second, it is possible to treat a patient’s reaction to tinnitus. Medications can be used to treat patients with depression and anxiety and to help with sleep problems. Chapter 4 in this book highlights how some of the more common medical conditions influence the counseling strategy. Medications for some patients are important, but they are not specific to tinnitus and will not be reviewed here. Counseling and sound therapy are two treatments that have been in common use since the early 1980s.
Counseling in the Treatment of Tinnitus
Whether we spend 1 minute or 60 minutes with a patient, talking with and listening to the patient are the cornerstone of the current treatment. Counseling for tinnitus patients is often performed by audiologists without a strong theoretical background in the many counseling strategies available. Psychologists frame different counseling approaches (and there are literally hundreds) using very specific guidelines. Table 1–3 provides a few examples of these frameworks, taken from an excellent summary by Flasher and Fogle (2004).
| Existential therapy | Concerns with individual’s overall existence in life, and how one deals with problems. Considers uncertainty meaning, and isolation (see Chapter 15) |
| Cognitive therapy | Thoughts influence behavior, erroneous ways of thinking are identified, and steps for coping and correcting thoughts are identified (see Chapters 6 and 8) |
| Humanistic therapy | Promotes personal growth and positive support in a nondirective fashion (see Chapters 5 and 15) |
| Behavioral therapy | Focus is on changing the ways patients behave (see Chapters 6, 9, and 14) |
These theoretical frameworks are also not mutually exclusive, but I suspect that tinnitus counseling would benefit from a deeper understanding of the theoretical background of different counseling approaches. Those clinicians who have some training in these approaches will put themselves in a better position to serve their tinnitus patients.
Be Supportive
We, and others, have noted how important it is to be supportive and to offer positive encouragement to the tinnitus patient (e.g., Coles and Hallam, 1987; Hazell, 1987; Tyler et al, 2001). This applies to any counseling strategy and includes the following:
• Be perceived as a knowledgeable professional.
• Demonstrate that you understand tinnitus.
• Provide a clear therapy plan.
• Be sympathetic.
• Show that you sincerely care.
• Provide reasonable hope.
Whatever counseling strategy is adopted, adherence to these general guidelines will likely be helpful.
Provide Information
Most of the therapies designed for tinnitus provide information. Whichever neurophysiological or psychological model you adhere to, providing information helps patients better understand their problems and feel less victimized, and puts them in a position of moving forward in treatment. Table 1–4 outlines the kinds of information that can be provided.
The relative importance of each of these topics is unclear. It is unlikely that discussing any of them would have a negative impact, and thus the question really is which to include or exclude, and how much time to spend on each topic. Obviously, too much information can be overwhelming for some patients, and it is possible to provide the information in too much detail or without sufficient clarity. This may prevent a patient from engaging in the other aspects of the treatment. We have proposed using pictures to facilitate the counseling process (see Tyler and Bergan, 2001).
| Hearing | How we hear Anatomy and physiology of hearing |
| Hearing loss | Anatomy and physiology of hearing loss Consequences of hearing loss |
| Tinnitus epidemiology | Prevalence of tinnitus Causes of tinnitus Common problems associated with tinnitus |
| Tinnitus mechanisms | Spontaneous activity of nerves Neurophysiological models (see Table 1–1) |
| Central nervous system | Role of the brain in perceiving and reacting to sound |
| Habituation | Effect of repeated exposure to stimuli Consequences of fearful stimuli Consequences of not habituating to tinnitus |
| Attention | Factors that contribute to attention |
| Learning | Factors that contribute to learning |
| Sleep | Factors that influence sleep |
| Concentration | Factors that contribute to concentration |
| Auditory training | Things that influence our hearing and understanding |
| Lifestyles | How our overall lifestyle, including eating, exercise, and activities, influences our health |
| Self-image | How our self-image influences our beliefs and reactions |
| Treatment options for hearing loss | Variety of treatment options available for hearing loss, including hearing aids, cochlear implants, and auditory training |
| Treatment options for tinnitus | Variety of treatment options available for tinnitus, including coping strategies, relaxation therapy, cognitive behavior therapy, and sound therapies |
Many of the counseling components of treatment focus primarily on providing information about hearing, hearing loss, and tinnitus (e.g., Bentler and Tyler, 1987; LaMarte and Tyler, 1987; Sheldrake et al, 1985; Tyler and Babin, 1986; Tyler and Baker, 1983). Some researchers, such as Hallam (1989), include discussions about habituation and attention in their approaches (see Chapters 6 and 10 in this book), whereas others focus more on brain mechanisms and learning. All of the clinicians writing in this book provide information on their particular counseling approach, and the diversity of topics and emphasis is evident. For example, in Chapter 2, Sizer and Coles present an informative brochure for patients, often a useful item to help patients remember tinnitus facts. Andersson and Kaldo in Chapter 3 show how the Internet can be used by patients to facilitate the transfer of information in conjunction with clinic visits. Newman and Sandridge in Chapter 14 show how the information can be shared efficiently in group therapy.
Many treatments for tinnitus are limited to providing information, and for many patients that is enough. If you can explain the causes of some problems, and perhaps even tell patients how they should react, this can be sufficient for patients’ understanding of their problems. With such knowledge, some patients will change their behavior regarding tinnitus. This is generally referred to as cognitive restructuring.
However, much more is involved in most counseling procedures than just providing information, or directing patients to some information that may be important. The next section discusses some counseling options.
Components of Counseling
Briefly, there are three components of most successful counseling programs:
• Changing thoughts
• Changing behavior
• Understanding an individual patient’s needs
CHANGING THOUGHTS
Providing information can change the way patients think about their tinnitus. However, simply lecturing a patient is not enough, even if the information is useful. Understanding what caused the tinnitus, how the patient learned to react to it, and how the patient can help himself or herself is important. This is a key part of treatments that include aspects of cognitive therapy (see Hallam et al, 1988; see also Chapters 6, 8, and 10 in this book), even for young children (see Chapter 16).
CHANGING BEHAVIOR
Sometimes it is possible to change behavior simply by providing information. However, it is usually more effective to practice the desired behavior. Some coping strategies involve changing behavior; others deal with emotional reactions. Providing specific tasks to engage in is part of changing behavior. Chapters 5, 9, and 14 offer numerous examples of engaging the patient in behavior management.
UNDERSTANDING AN INDIVIDUAL PATIENT’S NEEDS
A broader perspective on tinnitus treatment involves understanding the individual patient, how the person views tinnitus, what support the patient has, and how tinnitus fits into the bigger picture of the patient’s overall life. Listening, as opposed to providing information, is the first step. Tinnitus existentialist therapy, as discussed in Chapter 15, is a wonderful example of this.
Examples of Counseling Treatment Protocols
Several counseling treatment protocols and strategies have been proposed. Most contain some aspect of providing information. Several go beyond that. Tyler and Baker (1983) suggest that counseling needs to consider all of the patient’s difficulties. They recommend that the major emphasis of counseling address the emotional problems related to tinnitus. Hazell (1987, p. 113) suggests that “it is fruitless and unrealistic to approach the tinnitus in isolation.” Table 1–5 reviews some of these protocols and strategies.
| Tyler and Baker (1983) Tyler and Babin (1986) Tyler et al (1989) | Informational counseling | Providing information Considering emotional problems related to tinnitus |
| Clark and Yanick (1984) | Informational counseling | Understanding individual patient needs Nurturing expectations |
| Sweetow (1984, 1986) | Cognitive behavioral therapy | Providing information Sleep Changing attitude and self-esteem Diversionary tactics (attention) Coping strategies Cognitive behavior therapy |
| Hallam (1989) | Habituation therapy | Habituation Attention Relaxation Modifying the environment |
| Coles (1987), Coles and Hallam (1987) | Habituation therapy | Providing information Relaxation Habituation of reaction to tinnitus |
| Hazell (1987) | Masking therapy | Providing information Consideration of all the patient’s problems (e.g., business, financial, and domestic) Reassurance Attention Relaxation The use of diaries Modifying the environment |
| Slater and Terry (1987) | Guided therapy | Providing information Attention Activities Habituation Lifestyle changes (being positive and active) |
| Lindberg et al (1988) | Tinnitus behavior therapy | Providing information Coping Various relaxation procedures |
| Stouffer et al (1991) | Informational counseling | Providing information Keeping diaries Changing activities |
| Jastreboff and Hazell (1994) | Retraining therapy | Providing information “Directive” approach |
| Davis (1995) | Living with tinnitus | Providing information Stress management Sleep Changing thinking |
| McKenna (1998) | Habituation therapy | Providing information Habituation Relaxation Reactions to stress Listening to the patient |
| Henry and Wilson (2001, 2002) | Cognitive behavioral therapy | Providing information Self-help strategies Sleep, depression Attention control Cognitive behavior therapy Relaxation Coping strategies Relapse prevention |
| Tyler and Erlandsson (2000) | Refocus therapy | Three tiers of treatment Attention Engagement in other activities |
COGNITIVE BEHAVIORAL THERAPY
Cognitive behavioral therapy has been applied to tinnitus for some time, has been discussed in the literature in great detail, and is arguably the only approach that has been shown to be effective in controlled studies (Andersson and Lyttkens, 1999; Dobie, 1999). Several general concepts are used in many tinnitus counseling protocols, although not always acknowledged. The “providing information” component is intended to change the way individuals think about their tinnitus. The basic premise of cognitive behavioral therapy (Henry and Wilson, 2001, 2002; Sweetow, 1984, 1986; see also Chapter 8 in this book) is the following: Your tinnitus is there. The way that you think about it results in a particular emotional reaction.
DIRECTIVE COUNSELING
One approach, directive counseling, or retraining therapy, stands alone in that it explicitly frowns upon considering individual needs, addressing personal concerns, and providing suggestions for initiating behavioral changes. For example, Jastreboff (1999, p. 291) describes it as a “teaching session”: “It is not, and never was, intended to be … collaborative.” Furthermore, it was never intended to “change a patient’s perception, attention and emotions towards tinnitus …, to improve a patient’s well-being, everyday life, social interactions and work abilities.”
The directive counseling approach prompted some concerns from several clinicians. For example, Wilson et al (1998) criticized retraining therapy for its “teaching” approach to counseling, which seemed to disregard standard counseling procedures that include a more interactive approach. Retraining therapy omitted basic principles leading the patient to discover unhelpful thoughts, develop realistic beliefs and attitudes, and modify their emotional response. Kroener-Herwig et al (2000) went on to criticize many components of retraining therapy, one of which was that it “completely neglected” procedures to help the patient modify behavior. They believed that many tinnitus sufferers require more sophisticated strategies than simply teaching information to them. Instead, they felt that some patients should receive intervention programs to change their beliefs about tinnitus, their emotions and behavior. McKenna (2004) questioned the underlying philosophy of Jastreboff’s model, noting that its reliance on a classical conditioning perspective ignores the human component of tinnitus.
Sound Therapies for Treating Patients’ Reactions to Tinnitus
Sound has been used for decades to treat tinnitus. Its role can be understood in terms of
• Reducing the attention drawn to the tinnitus
• Reducing the loudness of the tinnitus
• Substituting a less disruptive noise (background sound) for an unpleasant one (tinnitus)
• Giving the patient some control (Coles, 1987; Vernon, 1977)
Sound therapies include the use of background sound, hearing aids, total masking, partial masking (including retraining therapy), and music therapy. Most of the chapters in this book include sound therapy directly or indirectly.
Counseling for Sound Therapies
Virtually all sound therapies are combined with some form of counseling, even if it is just providing information. More typically, in addition to basic information about tinnitus, hearing loss, attention, and habituation, specific counseling is included on the use of sound. This is true whether the sound therapy uses hearing aids or partial masking. Bentler and Tyler (1987), in their discussion of sound therapies, noted that, regardless of the management regimen chosen, counseling needs to be considered an integral component. Coles (1987, p. 395) said that “good counseling will go far toward interrupting the sort of vicious cycles” in addition to the sound therapy. Table 1–6 lists some of the topics that are typically covered in counseling for sound therapy.
Occasionally, sound therapies are represented as if they do not include counseling. For example, Henry and Wilson (2002, p. 574) suggest that no specific counseling protocol has been published for partial or total masking. This is at odds with the tinnitus partial masking therapy proposed by Hazell (1987). In Hazell’s discussion of masking therapy, detailed counseling strategies are an essential component. In my opinion, no sound therapy should be administered without counseling. Davis (Chapter 11), Searchfield (Chapter 12), and Folmer et al (Chapter 13) share this perspective.
Use of Hearing Aids
Listening to background sound has been recommended in treating tinnitus for over 50 years (Goodhill, 1950). Because most patients with tinnitus also have hearing loss, the use of hearing aids to amplify the background noise is a logical step (Johnson and Goodwin, 1981; Vernon and Schleuning, 1978), and many clinicians note the benefit (e.g., Bentler and Tyler, 1987). Chapter 12 provides an excellent detailed strategy for fitting hearing aids for tinnitus patients.
| Rationale behind the use of background sound |
| Caution about using noise generators that are too intense; may interfere with speech and everyday sound perception and may damage hearing |
| Selecting the type of noise generators |
| Selecting the ear or ears to receive noise generators |
| Selecting the ear mold(s) to use, if applicable |
| Trial periods of the background noise |
* After Hazell, 1987; Tyler and Bentler, 1987.
Total Masking Therapy
With total masking therapy, the patient no longer hears the tinnitus. This has some obvious appeal, and many patients find it very helpful. An important benefit is providing the patient with control. A detailed total masking therapy was proposed by Vernon and Schleuning (1978), Vernon and Meikle (2000), Hazell (1987) (see also Hazell et al, 1985), and Slater and Terry (1987). Hazell and Wood (1981) emphasized the importance of using a broadband signal. The large-scale study of tinnitus maskers by Hazell et al (1985) demonstrated the effectiveness of tinnitus masking. They found that counseling is helpful and that masking can provide additional benefit. However, some patients do not like the noise generated with masking, and for others the required noise can be too loud. One of the main advantages of total masking over other forms of masking, including setting noise at the “mixing point,” as in retraining therapy (Jastreboff and Hazell, 1993), is that some patients enjoy the immediate relief of the complete elimination of the tinnitus.
There is a misperception that total masking therapy provides only temporary relief and that the benefit of total masking is helpful only while the tinnitus is being masked (see, e.g., Henry and Wilson, 2002; Jastreboff and Hazell, 2004, p. 210). Neither of these points is true. Providing the patient with relief and control is very important with total masking and all forms of partial masking. With counseling, all forms of sound therapy can break the vicious cycle and facilitate dramatic long-term benefits. For example, Hazell (1987) recommended that patients be instructed not to expect maximum benefit immediately; instead, 2 or 3 months of masker use may be required. Furthermore, Hazell noted the beneficial long-term effects of masking: “As the patient focuses less attention on the tinnitus while it is masked, it may become less troublesome and obtrusive when the masker is removed” (p. 114). Total masking therapy is one of the options discussed in Chapter 13.
Fig. 1–2 shows a schematic representation of total masking. For many patients, it will not be possible to mask the tinnitus, and for others, the noise required is so intense that total masking is inappropriate.
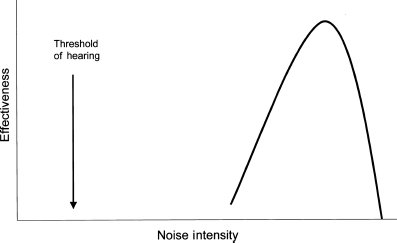
Figure 1–2 A schematic representation of total masking. With total masking, the tinnitus cannot be heard. Instead, the masker is perceived.
The noise can sometimes result in an increase in the tinnitus. Tyler and Bentler (1987) suggest
• Occasional rest from the noise generator
• Changing the level or spectrum of the noise generator
Other strategies for limiting the potential influence of noise on speech or everyday sound perception are
• Use low-level noise in the region of 500 to 3000 Hz.
• Use a unilateral masker.
Partial Masking Therapy
In the late 1970s and early 1980s, several researchers observed that some patients required high levels of noise to mask the tinnitus, or even could not mask the tinnitus completely. Vernon and Schleuning (1978) stressed that the actual level of the noise should be under the control of the patient. Hazell and Wood (1981) found that the masking noise can be set so that the patient hears both the masking sound and the tinnitus. They noted that the noise provides a distraction that makes patients concentrate less on the tinnitus itself. Other authors reported that the intensity of the tinnitus can be reduced with the use of noise that did not completely mask the tinnitus, or partial masking.
This approach allowed patients to determine the level of noise they could tolerate. Hazell (1987, p. 114) said that the masking sound “is most often effective at an apparent intensity much less than that of the patient’s tinnitus.”
Partial masking is a term that comes from the psychoacoustic literature, referring to the observation that the loudness of a tone can be reduced in the presence of background noise (see, e.g., Scharf, 1971). Jastreboff and Hazell (1993) have argued that using partial masking at the mixing point, with the noise and the tinnitus audible, is important to facilitate habituation. This may or may not be true. Habituation can occur with counseling alone (see Chapter 6 in this book), even with total masking therapy. If it is important to be able to hear the tinnitus to facilitate habituation, it may be that low levels of partial masking below the mixing point are more desirable because the sound of the tinnitus would be similar to its usual quality and loudness. I was taught that the terms masking referred to a psychophysical phenomenon and suppression to a physiological phenomenon, but these words often have been used interchangeably. We do not know the mechanism of partial masking, but it is important that we be clear when we reference psychophysical or physiological observations.
Table 1–7 reviews several sound therapies that have promoted partial masking, together with the instructions provided to the patient.
Detailed protocols for fitting “maskers,” including partial masking, is provided by Hazell and Wood (1981), Sheldrake et al (1985), and Hazell (1987). The use of sound therapy, including partial masking, is reviewed in Chapter 13.
Fig. 1–3 shows a schematic representation of partial masking. The advantages of this procedure are that a comfortable level can be found for most patients and that precise levels are not targeted, which may concern a patient or focus attention on the tinnitus. One disadvantage is that even low levels can interfere with speech perception; another is that some patients will find any background sound bothersome. These disadvantages are found for all types of sound therapy.
| Tyler and Babin (1986) | “Both the noise and tinnitus are heard, but the tinnitus is reduced in loudness” (p. 3213). Patients should “use the lowest level masker that provides adequate relief” (p. 3213). |
| Coles and Hallam (1987) | “A low level background sound against which the loudness of the tinnitus is reduced” (p. 994). |
| Erlandsson et al (1987) | Reduced the noise from the complete masking condition until it was “comfortable enough to listen to” (p. 40). |
| Hazell (1987) | “The masking sound does not completely cover the tinnitus,” and it provides a “distracting background sound” (p. 107). The “tinnitus tends to ‘break through’ the masking noise” (p. 112). |
| Coles (1987) | “When the masker is used to provide only a low level of background sound against which the loudness of the tinnitus is reduced” (p. 398). |
| Tyler and Bentler (1987) | “Sometimes a masker can reduce the tinnitus loudness or annoyance, even though the tinnitus remains audible” (p. 55). “Partially mask the tinnitus yet produce the lowest SPLs and the least interference with speech” (p. 59). |
| Bentler and Tyler (1987) | “Urge the patient to use the lowest… masker level that provides adequate relief” (p. 30). |
| Jastreboff and Hazell (2004) | “Below the level creating annoyance or discomfort” (p. 210). |
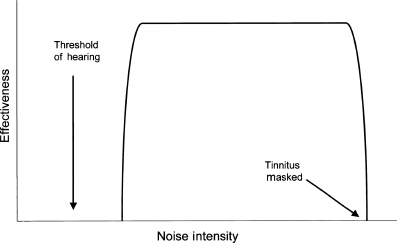
Figure 1–3 A schematic representation of partial masking. The advantage of this procedure is that a comfortable level can be found for most patients, and precise levels are not targeted, which may concern the patient or focus attention on the tinnitus. One disadvantage is that even low levels can interfere with speech perception with some patients; another is that some will find any background sound bothersome. These disadvantages are found for all types of sound therapy.
PARTIAL MASKING AT A SIMILAR MAGNITUDE TO THE TINNITUS (THE MIXING POINT)
A specific subcategory of partial masking has been described by several authors. Hazell (1987), for example, noted how it is better for some patients to have the tinnitus just audible through the masking sound. Coles (1987) suggested that the masker be turned up until its loudness is equal to that of the tinnitus, when the patient will often have to listen hard to hear it: “When this … is done the patient will usually accept that [the tinnitus] is no longer something to worry about” (p. 398).
Jastreboff (1998, p. 93) later referred to this as the mixing point, “where the patient perceives that the tinnitus sound and the external sound start to mix or blend together.”
The value of the mixing point over other levels afforded by partial masking has not been tested. As noted by Hazell (1987) and Coles (1987) above, the partial masking level at which the noise and tinnitus are similar will likely be preferable for some patients.
Fig. 1–4 shows a schematic representation of the mixing point, where the masking noise is at a level similar in magnitude to the tinnitus. Some patients find it difficult to determine the mixing point, whereas others find that the noise required for a mixing point is so intense that the lower levels of partial masking are preferable.
Music Therapy
For many tinnitus sufferers, listening to background music represents a more acceptable and even pleasant alternative to background noise. Slater and Terry (1987) found that almost 50% of tinnitus patients they sampled listened to music to help with their tinnitus. I believe that the use of music therapy with tinnitus patients deserves much more attention than it currently gets. The use of background music is recommended by Searchfield in Chapter 12 and by Folmer and colleagues in Chapter 13. A very specific protocol is reviewed by Davis in Chapter 11.
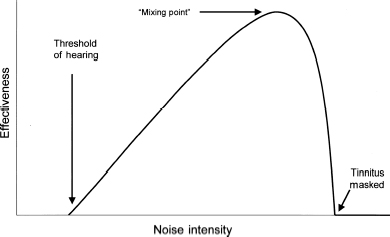
Figure 1–4 A schematic representation of one particular form of partial masking, referred to by Hazell (1987) as having tinnitus “just audible through the masking sound”; by Coles (1987) as “the masker can be turned up until its loudness is equal to that of the tinnitus, when the patient will often have to listen hard to hear the tinnitus”; and by Jastreboff (1998) as the mixing point “where the patient perceives that the tinnitus sound and the external sound start to mix or blend together” (p. 93).
Sound Therapy for Tinnitus Accompanied by Hyperacusis
WHAT IS HYPERACUSIS?
In a patient with hyperacusis, sounds that would normally be considered loud are instead heard as very loud. Thus loudness discomfort levels for pure tones are lower than normal, perhaps at 80 or 90 dB HL (for a review, see Nelting, 2003). It has been many years since hyperacusis was first associated with tinnitus (Tyler and Conrad-Armes, 1983). Hazell et al (1985) reported that the mean uncomfortable loudness levels in tinnitus patients were 10 to 15 dB lower than in hearing-impaired patients without tinnitus. However, the relationship between tinnitus and hyperacusis remains obscure. Loudness is thought to be coded by the number or level of activity of nerve fibers. The presence of hyperacusis implies that, for a given intensity, more nerve fibers or a higher rate of activity is produced than would occur normally. Hazell (1987) suggested that the central nervous system exerts a “gain control” mechanism to increase peripheral sensitivity affecting outer hair cell activity and tinnitus. This concept was included in a later model proposed by Jastreboff (1990) of a gain control mechanism involved in tinnitus.
HYPERACUSIS TREATMENT IN TINNITUS PATIENTS
The presence of hyperacusis in tinnitus patients requires some additional counseling and sound therapy considerations. Some patients develop a fear of sounds, or phonophobia. The main difficulty with hyperacusis in the treatment of tinnitus arises because the use of sound therapy can sometimes result in exacerbation of the hyperacusis or phonophobia. Therefore, it is important that clinicians treating tinnitus determine if their patients have hyperacusis, and to accommodate this if they are using sound therapy.
Sheldrake (1986, cited by Coles, 1987) recommended that noise generators be worn for hyperacusis patients for ∼6 hours per day. The noise should be “audible but comfortable (not necessarily completely masking any tinnitus …)” (p. 399). Sheldrake suggested that hyperacusis patients recovered over a period of a few days to up to 6 months in some cases; many patients gradually regain their tolerance of loud sounds.
Hazell (1987, p. 109) proposed a treatment of hyperacusis using a gradual and continuous introduction of sound into the ear to desensitize the ear to the effects of loud sounds. He noted that many hyperacusis patients use earplugs or earmuffs to protect their ears from loud sounds, but said that “it cannot be overstressed how counterproductive these measures are,” and that their use should be discouraged. Instead, he proposed a hyperacusis treatment procedure that begins with low levels of masking sound. Hazell recommended that the noise level be increased in level and duration gradually. A similar approach to hyperacusis has been suggested by Jastreboff et al (1998), except that they suggested the noise be used all the time. We note that hyperacusis patients often have hearing loss, and that the use of noise “all the time” may be unrealistic and can interfere with speech perception. Coles (1987) also cautioned against the use of earplugs in hyperacusis patients. Vernon and Press (1998) have suggested a desensitization protocol, whereby patients listen to intense, but not uncomfortable, “pink” noise for ∼2 hours per day.
Phonophobia, the abnormal fear of sounds, is not necessarily related to loudness. The fear can be related to a specific sound or general class of sounds. Phonophobia can be helped by treating hyperacusis. It may be useful to follow the psychological principles of successive approximations. Starting with the least aversive sound, the approach would be to gradually expose the patient to sounds that are more and more similar to the sounds that elicit the phonophobia. Research is needed on treating hyperacusis and phonophobia.
Obstacles to Tinnitus Treatment
Negative Beliefs by Clinicians or Patients
Many clinicians have beliefs that represent obstacles to tinnitus treatment. For example, they believe that
• They do not have the training.
• They cannot help the patient.
• They will not be reimbursed.
One of the primary purposes of this book is to provide very concrete examples of a variety of treatment strategies. Audiologists, clinical psychologists, and otologists should have the training to implement most of these options. I believe patients can be helped by all the treatments described in this book. Research will eventually determine which are the most helpful and which treatments work best for which patients. Reimbursement should follow studies showing treatment effectiveness; when that happens, more clinicians will make the time to provide tinnitus treatment. It is our job, as clinicians, to show patients how to learn to live with their tinnitus.
Patients also have concepts that are obstacles. They sometimes believe that
• There is nothing that can be done.
• No one understands their tinnitus.
• Someone, somewhere, has the cure.
Patients who believe nothing can be done to ease the tinnitus often do not seek treatment. This can delay intervention and creates a more problematic case of tinnitus by the time the patient finally seeks help. The beliefs that nothing can be done and that no one understands are distressing to patients. Their crisis deepens, and they may withdraw further. Desperate patients with the financial resources will travel great distances and pay substantial fees if they believe there is hope for them. If they are unsuccessful, this often makes their situation worse. By providing good therapy, and demonstrating it by measuring clinical effectiveness and making this information public, patients in need will seek help.
DURATION AND NUMBER OF SESSIONS
The optimal number and duration of treatment sessions will vary across patients. Some patients will require long-term follow-up visits; this should not be viewed as inherently undesirable. For many patients, a simple 5-minute discussion will be sufficient. For others, much longer sessions will be necessary (see Tyler and Erlandsson, 2000, for strategies). The clinical psychology literature indicates that most patients will benefit from several short (less than 1 hour) visits over several weeks.
Hazell (1987) suggested that sound therapy typically requires 2 to 3 months of noise-generator use before any benefit is achieved. Research can be used to determine the optimum treatment duration. This will vary across individuals. The number of sessions and their duration will likely be linked to reimbursement.
REIMBURSEMENT
Reimbursement is often available for diagnosing hearing loss and tinnitus. In the United States, there are reimbursement codes for treating central auditory processing disorders and for providing aural rehabilitation. Additionally, there are numerous reimbursement codes for providing psychological treatments, including insight-oriented, behavior-modifying, and supportive psychotherapy, interactive psychotherapy, family psychotherapy, biofeedback, behavior modification, and cognitive behavior therapy. These codes are typically used by clinical psychologists and psychiatrists. Research demonstrating clinical effectiveness of tinnitus treatment will facilitate reimbursement.
QUALIFICATIONS OF AUDIOLOGISTS TO DO PSYCHOLOGICAL COUNSELING
Counseling of tinnitus patients should be performed only by clinicians who have the training and professional license to do so. Flasher and Fogle (2004) suggest that audiologists can use basic psychological principles and techniques for which they have knowledge. Clearly, patients who have clinical depression, anxiety disorders, or other psychiatric ailments demand appropriate referrals. This does not mean that audiologists cannot be involved in treating the tinnitus in these cases, however. In my experience, psychiatrists and psychologists often welcome a collaborative effort with an audiologist who has experience in treating tinnitus.Treating tinnitus patients requires a commitment, a plan, and some clinical expertise. You are likely committed if you are reading this book, and if you do not have a plan, this book will offer several options. Clinical expertise comes from training, experience, and certain personal characteristics that can be learned and are often facilitated by personal supervision of real clinical experience. Some of the desirable characteristics are as follows (after Flasher and Fogle, 2004; Gladding, 2000; Riley, 2002):
• Ability to listen
• Patience
• Ability to be encouraging to the patient
• Ability to talk candidly about depression, anxiety, and other psychological problems
• Emotional insightfulness
• Self-awareness
• Ability to laugh at the bittersweet aspects of life
• Positive self-esteem
• Emotional stability
Conclusion
Counseling and sound therapy are the fundamental treatments for tinnitus. There are many counseling options, and most include providing information on hearing loss, tinnitus, and attention. Differences exist on how much time to spend on each area, but this is a secondary issue. I believe that counseling should consider the individual’s emotional state and focus on providing coping strategies. I think audiologists can learn more from aspects of cognitive and behavioral therapy as they are applied to other problems. A greater emphasis should be placed on improving sleep. Some patients may benefit from systematic therapies covering concentration and relaxation, but these can be offered as optional. The detailed comprehensive therapy plans provided by Henry and Wilson (2001, 2002) are important contributions and supplement the comprehensive therapy protocols of Hallam (1989), Slater and Terry (1987), and Davis (1995). The chapters in this book demonstrate varied approaches to counseling.
Sound therapy, involving wearable and nonwearable devices, should be considered an option for most tinnitus patients. Providing background sound removes some of the annoying characteristics of a piercing tinnitus. I believe that total and partial masking therapies with a focus on the mixing point do help some patients, but for many the resulting background noise levels are too intense. Lower levels of partial masking generally are more acceptable. Also, many patients do not want to listen to any levels of noise, and attempts to force sound therapy on them can be counterproductive. Finally, the use of music and other types of nonrandom noise in treating tinnitus should be explored.
Acknowledgments
We wish to acknowledge grant support provided by the American Tinnitus Association and the National Institutes of Health (NIH Grant 5R01DC005972–02).
Richard Tyler is an Obermann Scholar at the Obermann Center for Advanced Studies at the University of Iowa. David Baguley, Anthony Cacace, Scott Mitchell, Richard Salvi, and Grant Searchfield made very helpful suggestions on an earlier draft.
References
Andersson G, Lyttkens L. A meta-analytic review of psychological treatments for tinnitus. Br J Audiol 1999;33:201–210
Bentler RA, Tyler RS. Tinnitus management. ASHA 1987;May:27–32
Cacace AT. Expanding the biological basis of tinnitus: cross-modal origins and the role of neuroplasticity. Hear Res 2003;175:112–132
Cacace AT. The limbic system and tinnitus. In: Snow J, ed. Tinnitus: Theory and Management. Hamilton, Canada: BC Decker; 2004:162–170
Clark JG, Yanick P. Tinnitus and Its Management. Springfield, IL: Charles C Thomas; 1984
Coles RRA. Tinnitus and its management. In: Stephens SDG, Kerr AG, eds. Scott-Brown’s Otolaryngology. Guildford, UK: Butterworth; 1987
Coles RRA, Hallam RS. Tinnitus and its management. Br Med Bull 1987;43:983–998
Dauman R. Electrical stimulation for tinnitus suppression. In: Tyler RS, ed. Tinnitus Handbook. San Diego: Singular; 2000:377–398
Dauman R, Tyler RS. Some considerations on the classification of tinnitus. In: Aran J-M, Dauman R, eds. Proceedings of the Fourth International Tinnitus Seminar. Bordeaux, France: Kugler & Ghedini; 1992:225–229
Davis P. Living with Tinnitus. Woolahra, Australia: Gore & Osment; 1995
Dobie RA. A review of randomized clinical trials in tinnitus. Laryngoscope 1999;109:1202–1211
Dobie RA, Hoberg KE, Rees TS. Electrical tinnitus suppression: a double-blind crossover study. Otolaryngol Head Neck Surg 1986;95(3):319–323
Eggermont JJ. Tinnitus: some thought about its origin. J Laryngol Otol 1984;9:31–37
Eggermont JJ. Physiological mechanisms and neural models. In: Tyler R, ed. Tinnitus Handbook. San Diego: Singular; 2000
Eggermont JJ, Roberts LE. The neuroscience of tinnitus. Trends Neurosci 2004;27:676–682
Erlandsson S, Ringdahl A, Hutchins T, Carlsson SG. Treatment of tinnitus: a controlled comparison of masking and placebo. Br J Audiol 1987;21:37–44
Flasher LV, Fogle T. Counseling Skills for Speech-Language Pathologists and Audiologists. Clifton Park, NY: Thomson/Delmar Learning; 2004
Fowler EP, Fowler EP Jr. Somatopsychic and psychosomatic factors in tinnitus, deafness, and vertigo. Ann Otol Rhinol Laryngol 1955;64:29–37
Gladding S. Conseling: A Comprehensive Profession. Upper Saddle River, NJ: Prentice Hall; 2000
Goodey R. Tinnitus: When the patient complains of noises in the ear. Patient Management 1988;17(9):75–89
Goodhill V. The management of tinnitus. Laryngoscope 1950;60:442–450
Hallam RS, Jakes SC, Hinchcliffe R. Cognitive variables in tinnitus annoyance. Br J Clin Psychol 1988;27:213–222
Hallam RS. Tinnitus: Living with the Ringing in Your Ears. New York: HarperCollins; 1989
Hallam RS, Rachman S, Hinchcliffe R. Psychological aspects of tinnitus. In: Rachman S, ed. Contributions to Medical Psychology. Vol 3. Oxford: Pergamon Press; 1984:31–53
Hazell JWP. Tinnitus masking therapy. In: Hazell JWP, ed. Tinnitus. London: Churchill Livingston; 1987:96–117
Hazell JWP, Jastreboff PJ, Meerton LE, Conway MJ. Electrical tinnitus suppression: frequency dependence of effects. Audiology 1993;32:68–77
Hazell JWP, Wood SM. Tinnitus masking: a significant contribution to tinnitus management. Br J Audiol 1981;15:223–230
Hazell JWP, Wood SM, Cooper HR, et al. A clinical study of tinnitus maskers. Br J Audiol 1985;19:65–146
Henry JL, Wilson PH. The Psychological Management of Chronic Tinnitus: A Cognitive-Behavioral Approach. Boston: Allyn & Bacon; 2001
Henry JL, Wilson PH. Tinnitus: A Self-Management Guide for the Ringing in Your Ears. Boston: Allyn & Bacon; 2002
Jastreboff MM. Controversies between cognitive therapies and TRT counseling. In: Hazell J, ed. Proceedings of the Sixth International Tinnitus Seminar. London: THC; 1999:288–291
Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 1990;8:221–254
Jastreboff PJ. Tinnitus: the method of P.J. Jastreboff. In: Gates G, ed. Current Therapy in Otolaryngology Head and Neck Surgery. 6th ed. St. Louis: Mosby-Year Book; 1998:90–95
Jastreboff PJ. Tinnitus habituation therapy (THT) and tinnitus retraining therapy (TRT). In: Tyler RS, ed. Handbook of Tinnitus. San Diego: Singular; 2000:357–376
Jastreboff PJ, Gray WC, Mattox DE. Tinnitus and hyperacusis. In: Cummings CWet al, eds. Otolaryngology Head and Neck Surgery. Vol 4. 3rd ed. St. Louis: Mosby; 1998:3198–3222
Jastreboff PJ, Hazell JWP. A neurophysiological approach to tinnitus: clinical implications. Br J Audiol 1993;27:7–17
Jastreboff PJ, Hazell JWP. Neurophysiological model of tinnitus: dependence of the minimal masking level on treatment outcome. Hear Res 1994;80:216–232
Jastreboff PJ, Hazell JWP. Treatment of tinnitus base on a neurophysiological model. In: Vernon J, ed. Tinnitus and Relief. Boston: Allyn & Bacon; 1998:201–216
Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. New York: Cambridge University Press; 2004
Johnson RM, Goodwin P. The use of audiometric tests in the management of the tinnitus patient. J Laryngol Otol Suppl 1981;48–51
Kaltenbach JA, Zhang J, Zacharek MA. Neural correlates of tinnitus. In: Snow JB, ed. Tinnitus: Theory and Management. London: BC Decker Inc; 2004:141–161
Kentish RC, Crocker SR, McKenna L. Children’s experience of tinnitus: a preliminary survey of children presenting to a psychology department. Br J Audiol 2000;34:335–340
Kiang NYS, Moxon EC, Levine RA. Auditory-nerve activity in cats with normal and abnormal cochleas. In: Wolstenholme GEW, ed. Sensorineural Hearing Loss. London: J&A Churchill; 1970, pp. 241–273
Kroener-Herwig B, Biesinger E, Gerhards F, Goebel G, Verena Greimel K, Hiller W. Retraining therapy for chronic tinnitus. Scand Audiol 2000;29:67–78
LaMarte FP, Tyler RS. Noise-induced tinnitus. AAOHN J 1987;35(9):403–406
LeDoux J. Emotion, Memory, and the Brain. New York: Simon & Schuster; 1994
Levine RA, Abel M, Cheng H. CNS somatosensory-auditory interactions elicit or modulate tinnitus. Exp Brain Res 2003;153:643–648
Liberman MC, Dodds LW. Single-neuron labeling and chronic cochlear pathology, III: Stereocilia damage and alteration of threshold tuning curves. Hear Res 1984;16:43–53
Lindberg P, Scott B, Melin L, Lyttkens L. Behavioural therapy in the clinical management of tinnitus. Br J Audiol 1988;22:265–272
McFadden D. Tinnitus: Facts, Theories, and Treatments. Washington, DC: National Academy Press; 1982
McKenna L. Psychological treatments for tinnitus. In: Vernon JA, ed. Tinnitus Treatment and Relief. Boston: Allyn & Bacon; 1998:140–155
McKenna L. Models of tinnitus suffering and treatment compared and contrasted. Audiological Medicine 2004;2:1–14
Mega MS, Cummings JL, Salloway S, Malloy P. The limbic system: an anatomic, phylogenetic, and clinical perspective. J Neuropsychiatry Clin Neurosci 1997;9:315–330
Moeller AR. Pathophysiology of tinnitus. Ann Otol Rhinol Laryngol 1984;93:39–44
Murai K, Tyler RS, Harker LA, Stouffer JL. Review of pharmacologic treatment of tinnitus. Am J Otol 1992;13(5):454–464
Nelting M, ed. Hyperakusis. Stuttgart: Georg Thieme Verlag; 2003
Penner MJ, Bilger RC. Adaptation and the masking of tinnitus. J Speech Hear Res 1989;32:339–346
Quaranta N, Wagstaff S, Baguley DM. Tinnitus and cochlear implantation. Int J Audiol 2004;43:245–251
Riley J. Counseling: an approach for speech-language pathologists. Contemporary Issues in Communication Disorders 2002;29:6–16
Rubinstein JT, Tyler RS. Electrical suppression of tinnitus. In: Snow J, ed. Tinnitus: Theory and Management. Hamilton, Canada: BC Decker; 2004:326–335
Salvi RJ, Lockwood AH, Burkard R. Neural plasticity and tinnitus. In: Tyler R, ed. Tinnitus Handbook. San Diego: Singular; 2000:123–148
Salvi RJ, Wang J, Powers NL. Plasticity and reorganization in the auditory brainstem: implications for tinnitus. In: Reich GE, Vernon JA, eds. Proceedings of the 5th International Tinnitus Seminar. Portland, OR: American Tinnitus Association; 1996:457–466
Scharf B. Fundamentals of auditory masking. Audiology 1971;10:30–40
Sheldrake JB, Wood SM, Cooper HR. Practical aspects of the instrumental management of tinnitus. Br J Audiol 1985;19:147–150
Slater R, Terry M. Tinnitus: A Guide for Sufferers and Professionals. London: Croom Helm; 1987
Stouffer JL, Tyler RS. Characterization of tinnitus by tinnitus patients. J Speech Hear Disord 1990;55:439–453
Stouffer JL, Tyler RS, Kileny P, Dalzell L. Tinnitus as a function of duration and etiology: counseling implications. Am J Otol 1991;12(3):188–194
Sweetow RW. Cognitive-behavioral modification in tinnitus management. Hearing Instruments 1984;35:14–52
Sweetow RW. Cognitive aspects of tinnitus patient management. Ear Hear 1986;7(6):390–396
Tonndorf J. Stereociliary dysfunction: a case of sensory hearing loss, recruitment, poor speech discrimination and tinnitus. Acta Otolaryngol 1981;91:469–479
Tyler RS. Tinnitus. In: Evered D, Lawrenson G, eds. Tinnitus. (Ciba Foundation Symposium 85). London: Pitman; 1981:136,137
Tyler RS. Perspectives on tinnitus. Br J Audiol 1997;31:381–386
Tyler RS, Babin RW. Tinnitus. In: Cummings CW, Fredrickson J-M, Harker L, Krause CJ, Schuller DE, eds. Otolaryngology–Head and Neck Surgery. St. Louis: Mosby; 1986:3201–3217
Tyler RS, Baker LJ. Difficulties experienced by tinnitus sufferers. J Speech Hear Disord 1983;48:150–154
Tyler RS, Baker LJ, Armstrong-Bednall G. Difficulties experienced by hearing-aid candidates and hearing-aid users. Br J Audiol 1983;17:191–201
Tyler RS, Bentler RA. Tinnitus maskers and hearing aids for tinnitus. Semin Hear 1987;8(1):49–61
Tyler RS, Bergan C. Tinnitus retraining therapy: a modified approach. Hearing J 2001;54(11):36–42
Tyler RS, Conrad-Armes D. The determination of tinnitus loudness considering the effects of recruitment. J Speech Hear Res 1983;26:59–72
Tyler RS, Conrad-Armes D. Masking of tinnitus compared to masking of pure tones. J Speech Hear Res 1984;27:106–111
Tyler RS, Erlandsson S. Management of the tinnitus patient. In: Luxon LM, Furman JM, Martini A, Stephens D, eds. Textbook of Audiological Medicine. Oxford: Isis; 2000:571–578
Tyler RS, Haskell G, Preece J, Bergan C. Nurturing patient expectations to enhance the treatment of tinnitus. Semin Hear 2001;22:15–21
Tyler RS, Smith RJ. Management of tinnitus in children. In: Newton VE, ed. Paediatric Audiological Medicine. Philadelphia: Whurr; 2002:397
Tyler RS, Stouffer JL, Schum R. Audiological rehabilitation of the tinnitus client. J Acad Rehab Audiol 1989;22:30–42
Vernon JA. Attempts to relieve tinnitus. J Am Aud Soc 1977;2:124–131
Vernon JA, Meikle M. Tinnitus masking: theory and practice. In: Tyler RS, ed. Handbook of Tinnitus. San Diego: Singular; 2000:313–356
Vernon JA, Moeller AR. Mechanisms of Tinnitus. Boston: Allyn & Bacon; 1995
Vernon JA, Press L. Treatment for hyperacusis. In: Vernon JA, ed. Tinnitus: Treatment and Relief. Boston: Allyn & Bacon; 1998:223–227
Vernon J, Schleuning A. Tinnitus: a new management. Laryngoscope 1978;88:413–419
Wilson JP. Theory of tinnitus generation. In: Hazell JWP, ed. Tinnitus. London: Churchill Livingstone; 1987:20–45
Wilson PH, Henry JL, Andersson G, Hallam RS, Lindberg P. A critical analysis of directive counseling as a component of tinnitus retraining therapy. Br J Audiol 1998;32:273–287
Wilson PH, Henry JL, Nicholas M. Cognitive methods in management of chronic pain and tinnitus. Aust Psychol 1993;28:172–180
Zwolan TA, Kileny PR, Souliere CR, Kemink JL. Tinnitus suppression following cochlear implantation. In: Aran J-M, Dauman R, eds. Tinnitus 91: Proceedings of the Fourth International Tinnitus Seminar. Amsterdam: Kugler; 1992:423–426
< div class='tao-gold-member'>



