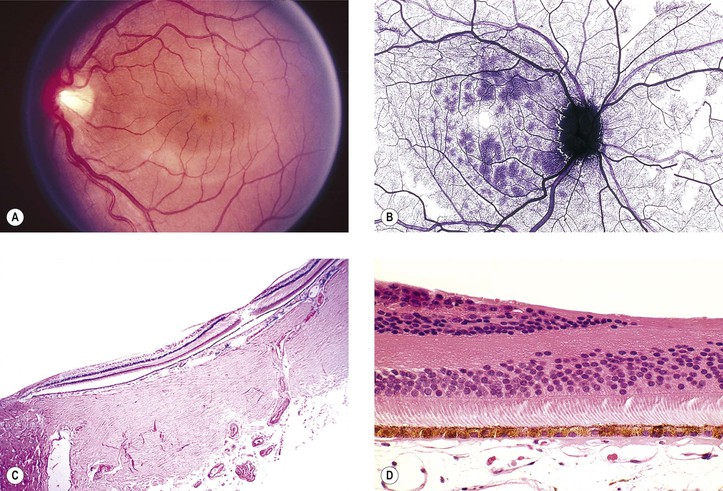
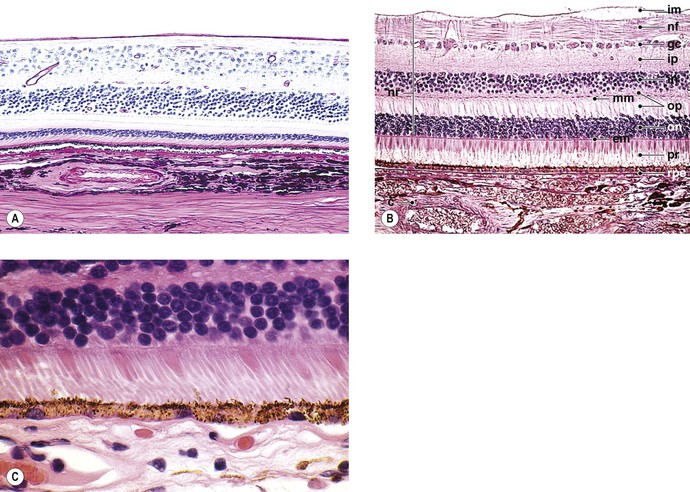
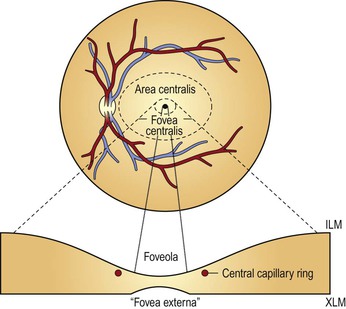
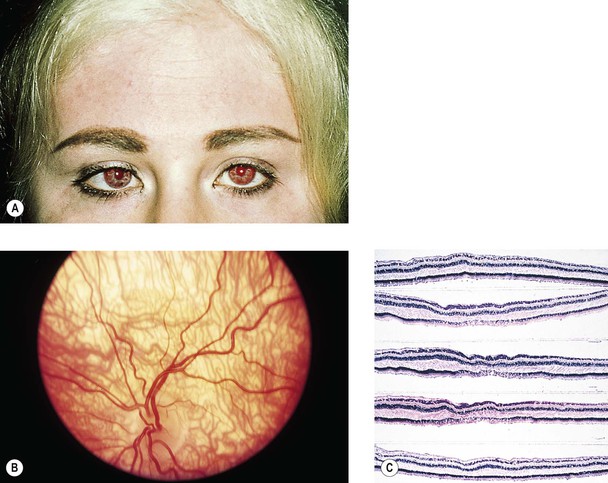
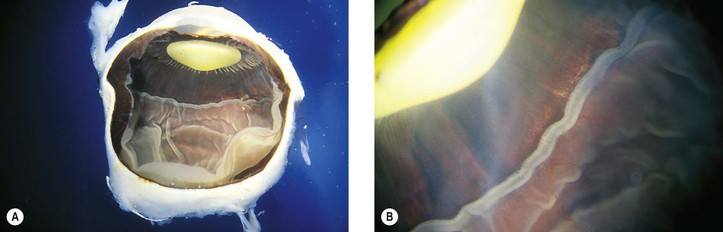
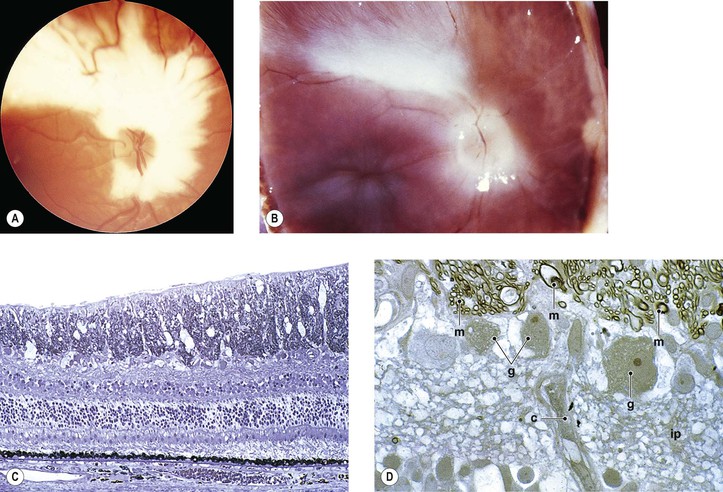
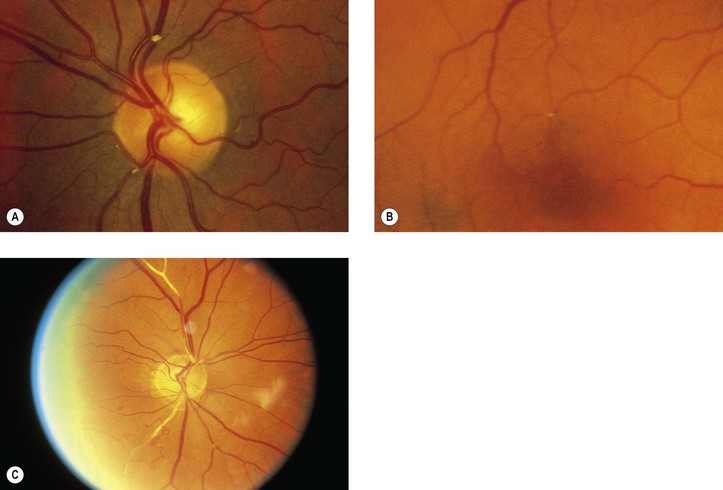
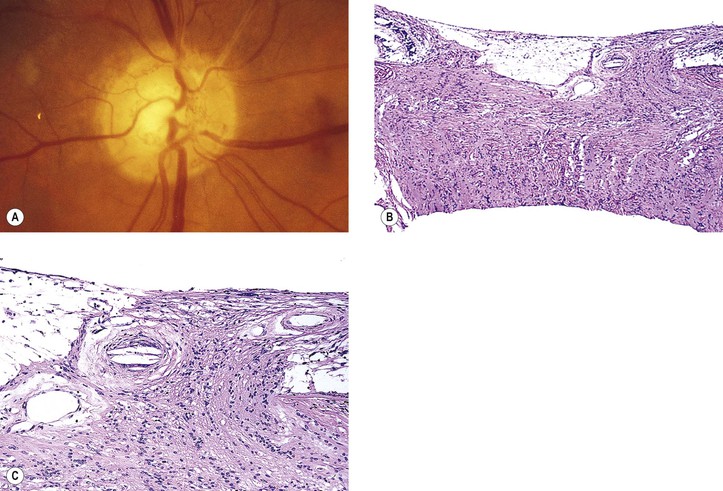
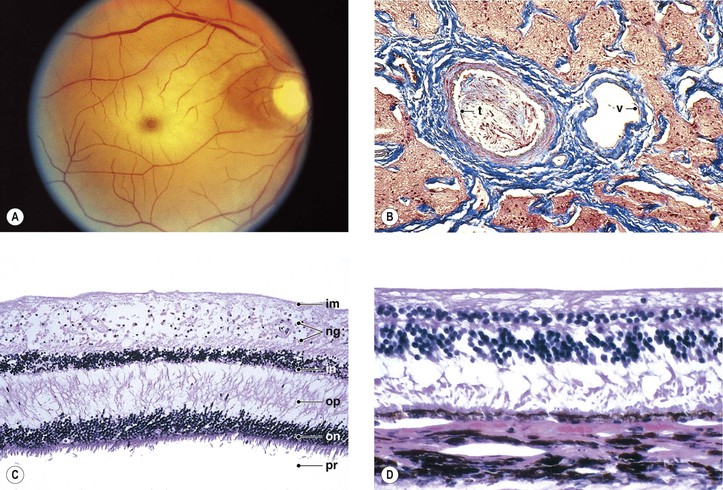
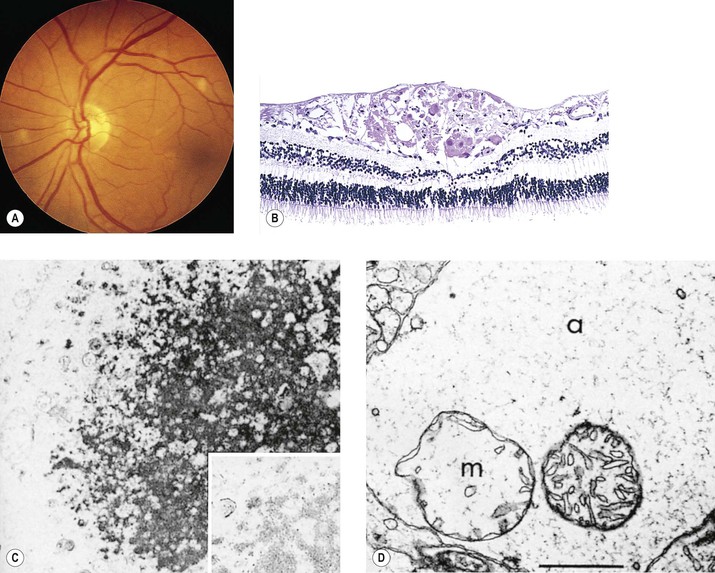
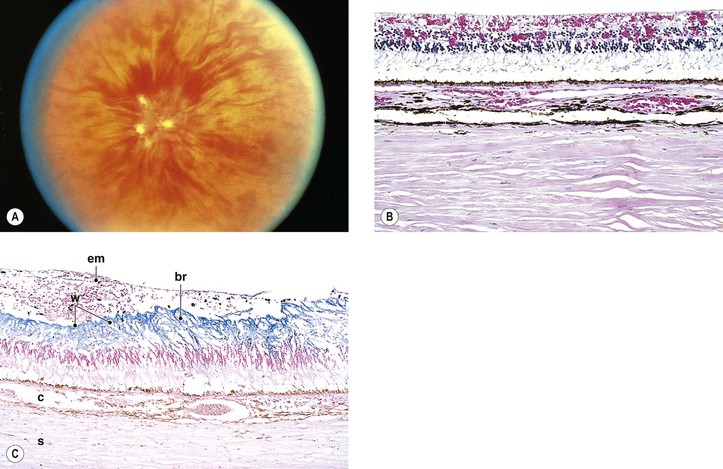
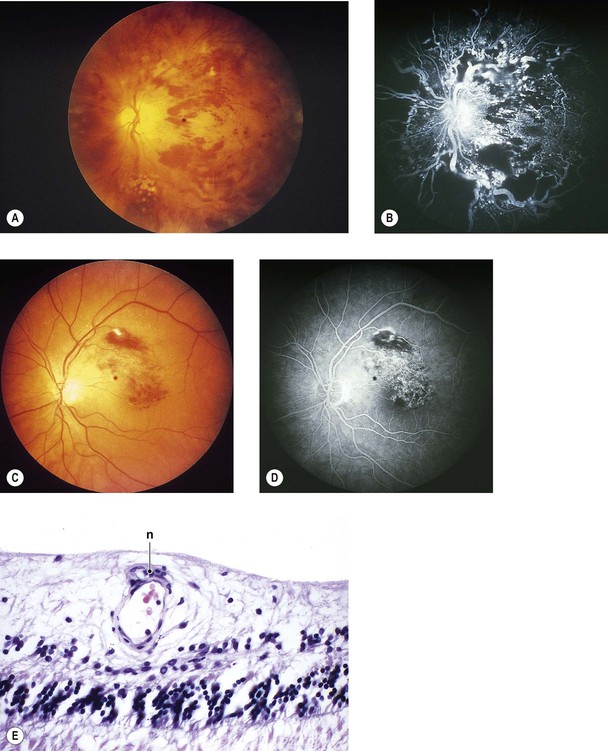
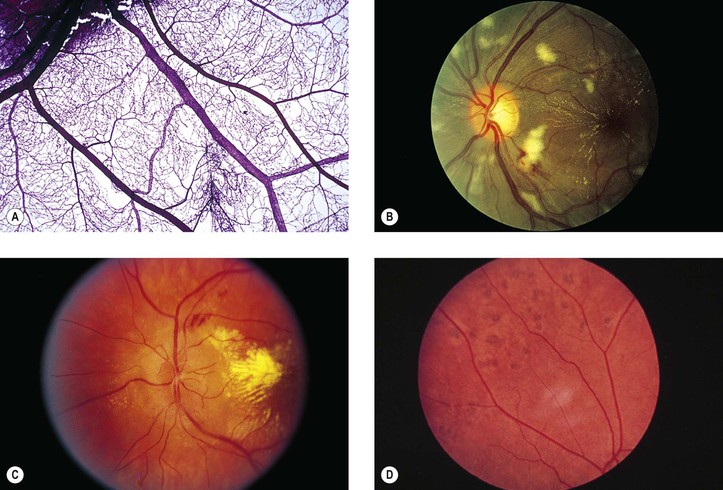
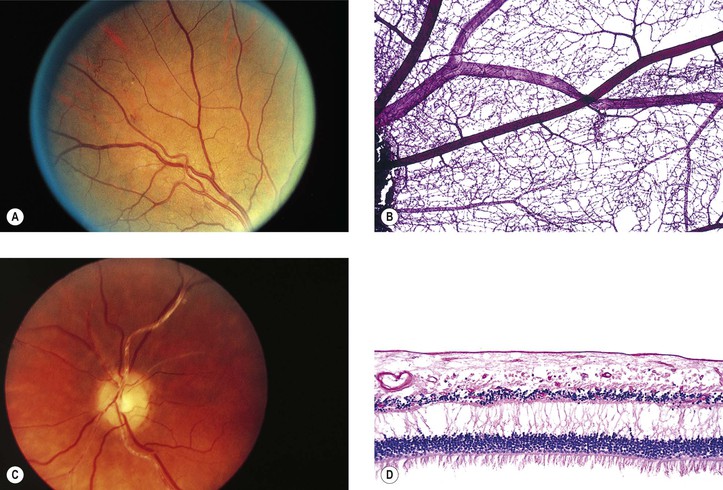
I. The neural retina (Figs. 11.1–11.3) is a highly specialized nervous tissue, in reality a part of the brain that has become exteriorized. A. Traditionally, the retina, from the RPE externally to the internal limiting membrane internally, is divided into 10 layers (see Fig. 11.2B). II. Foveomacular region of the neural retina A. Clinicians often confuse the proper use of the terms fovea, macula, and posterior pole (see Fig. 11.3). 4. The anatomic macula (which corresponds to the clinical posterior pole) comprises an area larger than the anatomic fovea. a. The term macula is derived from the term macula lutea. c. The anatomic macula actually encompasses an area contained just within the optic nerve and the superior and inferior retinal temporal arcades, and extends temporally approximately two disc diameters beyond the central fovea. III. The conditions are noted at birth. B. Color vision is normal. Nyctalopia does not occur. IV. Histology A. The RPE is depleted of pigment. B. Macromelanosomes may be present within the RPE. A. Inheritance is autosomal recessive. B. The condition is one of the immunodeficiency diseases (see Chapter 1) and is associated with a lack of resistance to infection and generalized lymphadenopathy. The condition is fatal from generalized infection, usually during the second decade of life. I. The typical coloboma “of the choroid” (see Fig. 9.8) involves the region of the embryonic cleft (fetal fissure; i.e., inferonasally) and is bilateral in 60% of patients. The coloboma may involve the total region, a large part of it, or one or more small isolated parts. II. Histologically, the RPE seems to be primarily involved and is absent in the area of the coloboma. A. The neural retina is atrophic and gliotic and may contain rosettes. I. Myelinated nerve fibers (MNF; Fig. 11.6) usually occur as a unilateral condition, somewhat more common in men than in women. B. Rarely, MNF occur after infancy and can progress. II. Clinically, they appear as an opaque white patch or arcuate band with feathery edges. I. Choroidal vascular insufficiency II. Retinal vascular insufficiency A. Large-artery disease anywhere from aortic arch to central retinal artery 1. Atherosclerosis shows patchy subendothelial lipid deposits and erosion of media. b. Embolic manifestations (Figs. 11.7 and 11.8; see also Fig. 5.54) 3) Rarely, ocular emboli cause a condition masquerading as temporal (cranial; giant cell) arteritis. 5. Temporal (cranial; giant cell) arteritis (see Chapter 13) B. Arteriolar and capillary disease of neural retinal vasculature 1. Arteriolosclerosis is associated with hypertension. 2. Branch retinal artery occlusion has many causes, including emboli (see Figs. 11.7 and 11.8), arteriolosclerosis, diabetes mellitus, arteritis, dysproteinemias, collagen diseases, and malignant hypertension. 3. Diabetes mellitus (see Chapter 15) 4. Malignant hypertension, toxemia of pregnancy, hemoglobinopathies, collagen diseases (Fig. 11.9), dysproteinemias, carbon monoxide poisoning, and blood dyscrasias of many kinds may involve the small retinal vessels and cause neural retinal ischemia. I. Early (Fig. 11.10; see also Figs. 11.9 and 11.15D) A. The neural retina shows coagulative necrosis of its inner layers, which are supplied by the retinal arterioles. 1. The neuronal cells become edematous during the first few hours after occlusion of the artery. 2. The intracellular swelling accounts for the clinical gray neural retinal opacity. B. If the area of coagulative necrosis (see Chapter 1) is small and localized, it appears clinically as a cotton-wool spot. 1. The cotton-wool spot observed clinically (Fig. 11.11; see also Fig. 11.9) is a result of a microinfarct of the nerve fiber layer of the neural retina. 2. The cytoid body, observed microscopically (see Figs. 11.9 and 11.11), is a swollen, interrupted axon in the neural retinal nerve fiber layer. II. Late (see Fig. 11.10) A. The outer half of the neural retina is well preserved. I. Occlusion of central retinal vein, branch retinal vein, or venule A. CRVO may be considered to consist of two distinct types. 1. Nonischemic retinopathy (~65% of cases, but approximately one-fourth of these eyes will convert to the ischemic type) 2. Ischemic (hemorrhagic) retinopathy a. It is caused by occlusion of the central retinal vein at, or anterior to, the lamina cribrosa, associated with retinal ischemia that leads to significant retinal hypoxia. 4. Bilateral CRVO may occur as part of the acquired immunodeficiency syndrome (AIDS). B. Branch retinal vein occlusion (BRVO) 1. BRVO occurs approximately three times more frequently than CRVO. In approximately two-thirds of cases, the superior temporal neural retinal vein is involved. Most of the remaining cases show involvement of the inferior temporal retinal vein. b. A hemispheric vein occlusion behaves like an ischemic CRVO. II. Papillophlebitis (retinal vasculitis, mild and moderate papillary vasculitis, benign retinal vasculitis, optic disc vasculitis) C. The prognosis for vision is excellent. I. Macular hemorrhagic infarction may result in permanent loss of vision. II. Leakage of fluid into the macula may result in cystoid macular edema. III. Iris neovascularization (clinically seen rubeosis iridis) A. Iris neovascularization (see Figs. 9.13 and 9.14) occurs mainly with ischemic CRVO; it rarely occurs with nonischemic CRVO or BRVO. IV. Neovascularization of the neural retina (Fig. 11.13) occurs mainly with BRVO; it rarely occurs with ischemic or nonischemic CRVO. I. Early—hemorrhagic necrosis of neural retina A. Massive intraneural retinal hemorrhage involves all the neural retinal layers. 1. The hemorrhage frequently spreads within the nerve fiber layer of the neural retina (see Fig. 15.18) and appears clinically in sheets or flame-shaped. B. Cytoid bodies (see Fig. 11.11) are common histologically but may be masked by the hemorrhages clinically. As the hemorrhages resorb, hard, waxy exudates may appear (see Chapter 15 and later in this chapter). II. Late—organization of hemorrhage and gliosis B. Gliosis (“scarring”) is usually seen in the inner neural retinal layers. C. Hemosiderosis of the retina (see Fig. 11.12C) is present, with the hemosiderin often located in macrophages. I. Hypertensive retinopathy (Fig. 11.14) A. Grade I: a generalized narrowing of the arterioles B. Grade II: grade I changes plus focal arteriolar spasms C. Grade III: grade II changes plus hemorrhages and exudates 1. Flame-shaped (splinter) hemorrhages (see Figs. 11.12–11.14; see also Fig. 15.18) are characteristic and present in the nerve fiber layer. 2. Dot-and-blot hemorrhages (see Figs. 11.13 and 15.18) may be seen in the inner nuclear layer with spreading to the outer plexiform layer. 3. Cotton-wool spots (see Figs. 11.11 and 11.14; see earlier in this chapter) are characteristic. 4. Hard (waxy) exudates may be seen; these are lipophilic exudates located in the outer plexiform layer (see Figs. 11.14, 15.13, and 15.16). D. Grade IV: all the changes of grade III plus optic disc edema II. Arteriolosclerotic retinopathy (Fig. 11.15) A. Grade I: an increase in the arteriolar light reflex B. Grade II: grade I changes plus arteriolovenular crossing defects C. Grade III: grade II changes plus “copper-wire” arterioles D. Grade IV: grade II changes plus “silver-wire” arterioles I. Neural retinal hemorrhages (see Figs. 11.12 and 15.18) may be caused by many diseases, such as diabetes mellitus (see Chapter 15), sickle-cell disease, retinal venous diseases, hypertension, blood dyscrasias, leukemias, polycythemia vera, subacute bacterial endocarditis, cytomegalovirus retinitis, acute retinal necrosis (ARN), lymphomas, idiopathic thrombocytopenia, trauma, multiple myeloma, pernicious anemia, collagen diseases, carcinomatosis, anemia, and many others. II. Histologically, the size and anatomic location of the hemorrhage determine its clinical appearance (see Fig. 15.18). III. Roth’s spots I. Retinal exudates (see Figs. 11.14, 15.13, and 15.16) II. Circinate retinopathy consists of a circular deposit of masses of hard, waxy exudates around a clear area, often within the anatomic macula. A. It is degeneration secondary to ischemic vascular disease (e.g., diabetes mellitus). B. Histologically, the exudates are identical to isolated, small, hard, waxy exudates. III. Histology A. Hard, waxy exudates (see Chapter 15) B. Cotton-wool spots (cytoid bodies; see earlier in this chapter and see Chapter 15)
Neural (Sensory) Retina
Normal Anatomy
Congenital Anomalies
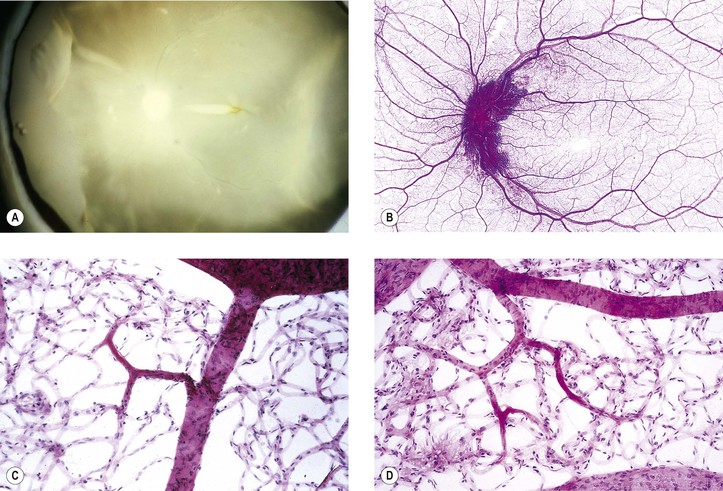
Albinism (Fig. 11.4)
Coloboma
Myelinated (Medullated) Nerve Fibers
Vascular Diseases
Definitions
Retinal Ischemia
Causes
Histology of Retinal Ischemia
Retinal Hemorrhagic Infarction (Fig. 11.12)
Causes and Risk Factors of Hemorrhagic Infarction
Types of Hemorrhagic Infarction
Complications of Hemorrhagic Infarction
Histology of Retinal Hemorrhagic Infarction (See Fig. 11.12)
Hypertensive and Arteriolosclerotic Retinopathy1
Hemorrhagic Retinopathy
Exudative Retinopathy
Neural (Sensory) Retina
11