11 Neoplasia and Tumorlike Lesions
Indications
• Diagnostic biopsy and postoperative control
• Mucopyoceles, retention cysts
• Expansive polyposis
• Granulomas
• Osteoma
• Fibroma, neuroma, adenoma
• Juvenile angiofi broma
• Inverted papilloma
• Squamous-cell carcinoma and adenocarcinoma
• Esthesioneuroblastoma
Principles
A variety of cysts, polyps, and granulomas growing in the nasal and paranasal cavities lie within the reach of endoscopic visualization and can, like most of the benign tumors, be completely removed by noninvasive rhinosurgery. Bioptical diagnosis and postoperative follow-up with the endoscope has become routine in most ENT services. Potential and genuine malignancies, if limited to the endoscopically attainable regions, are also increasingly subjected to endonasal and transnasal surgery. According to their malignant/benign status, location, and extent, the individual procedure varies considerably and may require multidisciplinary action, including radiochemotherapy. Approved techniques will therefore be described in the context of the different diseases.
Operative Technique
Diagnostic Biopsy and Postoperative Management
Nasal obstruction, epistaxis, dysolfaction and other presenting symptoms require endoscopic examination. Whenever miscolored mucosa, ulceration that does not heal, or abnormal granulations have become visible, endoscopic biopsy is indicated. Small biting forceps from the otological armamentarium or fine double-cups are useful, and are usually part of the rhinological equipment. The specimen to be sent for histological examination is taken out of the margin of the suspicious lesion. Questionable results from an area that is difficult to reach have to be repeated. Cytological swabs are only reliable with a positive outcome. If aspect and history raise the suspicion of a noxious infection, a piece or a swab is sent for microbiological and mycological examination.
Postoperative controls are easier to execute because the surgical field is broadly accessible. The bioptical excision, however, must be deep enough to ensure that local recurrences are not hidden by superficial scar tissue. If the biting instrument does not work, for instance on a fl at texture over bone, the area to be scrutinized is curetted and the abraded material is sent for microscopy. Great care must be taken in precisely marking different samples for the location of their origin. The histopathologist must be able to report on the spatial distribution of a recurrence. A simple summary statement “locally recurrent” is uninformative for a goal-directed revision. During a postoperative endoscopic follow-up, granulations and local polypous edema are normal tissue reactions from denuded bone. They must not be misinterpreted as neoplasia but are treated by local abrasion, etching, and smearing with ointment, and eventually with additional systemic corticoid therapy (see Chapter 1).
Mucopyoceles
These tumorlike lesions are defined as space-occupying cystic formations that are internally lined with mucous epithelium; they grow across the natural borders of a preformed cavity like a hernia and are therefore named celes. A simple cyst within a cavity is not a hernia. The formation of a cele is usually due to a defi nite blockade of the normal drainage of a mucosal lining following a sinus operation. This pathogenesis is not rare after an inadequate frontal sinusotomy with external access, whereas endoscopic sinus surgery very seldom provokes noxious retention. Mucoceles can thus be categorized as complications of sinusitis see also Chapter 7). They can reach enormous size and exert pressure on nerves and other organs, and also occlude nasal and pharyngeal pathways (see Fig. 7.9).
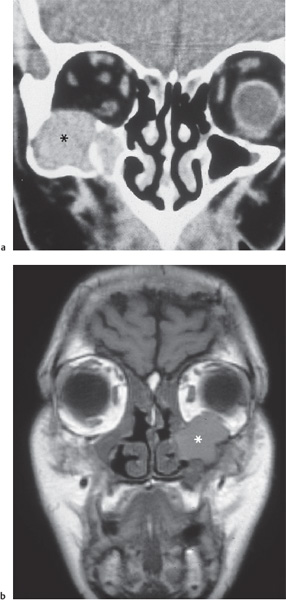
Fig. 11.1 a, b Space-occupying mucoceles (*) from occluded antral mucosa.
a Marked distension of the zygomatic bone and orbital compression from below (coronal CT).
b Orbital invasion after occlusion of the antrostomy by scar formation after Caldwell–Luc operation 20 years ago (coronal MRI, T1-weighted). Double vision and protrusio bulbi since 8 weeks.
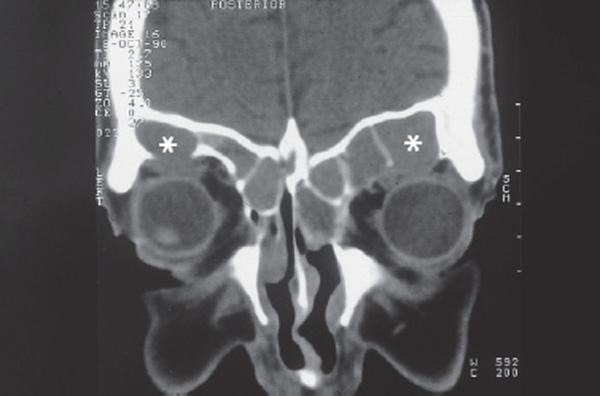
Fig. 11.2 Bilateral mucoceles (*) of both frontal sinuses after previous radical operation depressing the orbits and requiring a combined endonasal–external (two-portal) access. Coronal CT.
The removal of mucoceles is comparatively simple. They need not be enucleated but are marsupialized, which means a broad excision from the covering membrane. After its resection, the upper wall of the cele will shrink and become part of the ethmoidal or sphenoidal roof. The residual internal surface will thus be transformed into the lining epithelium of the underlying cavity. This very easy management can be executed almost everywhere endoscopically, especially in the anterior ethmoid, the maxillary cavity (Fig. 11.1a, b) , at the medial orbital wall, and at the sphenoid. Lateral frontal and deep intraorbital mucoceles without a bony shelf, on the other hand, will often require an external transfacial approach, when visualization and the excision are not feasible with either angled rigid or flexible instruments (see Chapter 7 and Fig. 11.2) (Constantinidis et al. 2001). The Nd:YAG laser can be applied through fl exible fiberscopes and may be sufficient for a resection of celes in such remote areas. Prophylaxis of recurrence should be reconsidered if a solid tunnel of bone is missing and the cele has developed into soft tissues. Then an external plastic reconstruction of the cavity is preferable. The author personally has never seen mucoceles penetrating from the ethmoid or sphenoidal roof through the skull base into the cerebral fossa, but an identical endoscopic management is conceivable.
The management of meningoencephaloceles was described in Chapter 10.
Expansive Polyposis
Nasal and paranasal polyps, mentioned in Chapter 6 as a special form of chronic rhinosinusitis, can in fact grow to an enormous size, and may even lead to atrophy and disfigurement of the adjacent bone (Fig. 11.3). They also can protrude into the nasopharynx or become visible in the nostrils. Such tumorous growth can even involve the middle ear and later the external ear via the eustachian tube. The detection of nasal polyps is always reason enough to order a CT series. Every case must be checked for an inherited entity like Marfan syndrome. The possibility of malignant degeneration must also be considered. The classical therapy consists of a thorough endoscopic removal of the lesions under normal precautions regarding an underlying sinusitis or another disease, flanked by a systemic and local corticoid therapy over a couple of weeks. The ablation from the nasal and paranasal cavities is facilitated by the use of a powered instrument such as the so-called shaver. The extraction of polyps with blunt slings is obsolete because of uncontrolled laceration of neighboring healthy mucosa, often resulting in stenosis and obstruction by scar formation. Also synechiae between the nasal septum and the middle turbinate are a frequent typical sequela of imprecise polypectomy. One reason for this, besides the lack of sharp instruments, is the blurring of the surgical field by hemorrhage. The administration of temporal compressions with cotton swabs soaked in epinephrine may help somewhat, but sometimes a second intervention after some weeks may be more prudent than a blind forceful extraction of every attainable polypoid tissue. The preservation of the nasal septum and of the turbinates is mandatory.
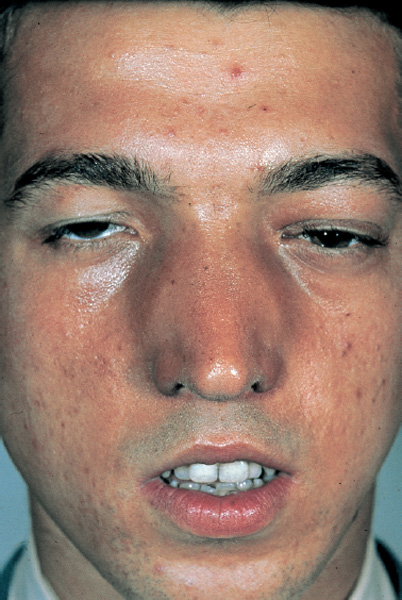
Fig. 11.3 Distension of the nasal pyramid by massive nasal polyposis during childhood.
Granuloma
Unspecific granulomas arise from the submucous tissue in deep inflammatory ulcerations, but may also originate from apparently epithelialized surfaces without a known reason. They can acquire considerable dimensions, and may store cholesterol crystals, and also develop cystic degeneration. Figure 11.4 a–c illustrates such a tumorlike cholesterol cyst in a frontal sinus. The cysts differ histologically from mucoceles by their lack of an internal mucosal lining. The storage of cholesterol is usually ascribed to the metabolism of hemosiderin after hemorrhage from occult trauma. Granulomas in the anterior nasal cavity, especially on the nasal septum, are usually due to chronic mechanical trauma caused by a finger or to other mishabits or to the chemical trauma of snuff-taking. They not uncommonly grow from the edge of a septal defect or on a postoperative bone wound (Fig. 11.5). Their removal by endoscopic or microscopic punching is followed by a single touch with silver nitrate 10% and subsequent application of panthenol ointment. Larger granulomas like that shown in Fig. 11.4 a, b are resected along the shortest endoscopic approach possible, here with an anterior ethmoidectomy and broad endoscopic frontal sinusotomy. Giant cholesterol granulomas may occur in the maxillary cavity, from where they can be removed endoscopically after their debulking into pieces (see Fig. 11.4c).
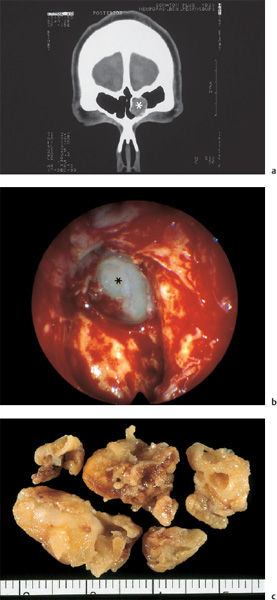
Fig. 11.4 a–c Ossifying cholesterol cyst in the left frontal sinus.
a Delineation of the tumorlike lesion (*) on a coronal CT scan.
b The endoscopic transnasal exposure of the mass in the frontal sinus (*).
c Removed cholesterol granuloma fragments (cm scale).
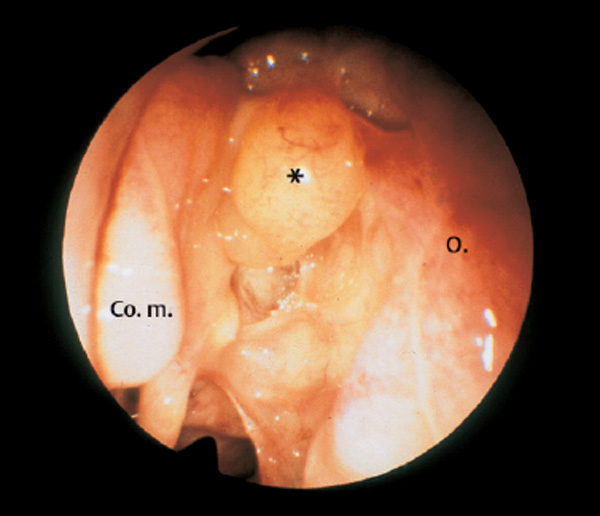
Fig. 11.5 Epithelialized, granulomatous tumorlike lesion (*) in a left anterior ethmoid occluding the nasofrontal duct (70° telescope). Development after previous partial ethmoidectomy.
Osteoma
Osteomas are among the most frequent tumors of the paranasal sinuses. They grow slowly and may remain stationary over a long period. Presenting symptoms are a deep, dull pain, and lateral ocular dislocation if they expand from the anterior ethmoid (Fig. 11.6a, b) . Originating in the frontal sinus, mostly from the lower posterior wall, they may acquire a large volume before exerting pressure and pain. Their consistency and their integration within the adjacent healthy bone vary considerably. Some resemble an ossifying cyst and are easy to lift. Others are harder and difficult to dissect. Some are quasi-pedicled, others are broadly based and can only be drilled out (Fig. 11.7a, b) . Invasion into the adjacent skull base (Fig. 11.8) must raise a suspicion of osteodysplasia.
The exposure of an ethmoid osteoma (Fig. 11.9a, b) is very simple. Since the ethmoid cells are usually not infected, only limited resection is needed, and in particular the medial wall of the middle turbinate should be completely preserved. The tumor is completely exposed by opening the ethmoid bulla, and by piecemeal removal of the overlying cells. If it is large or wedged by lateral processes, it can be broken up in situ with the diamond burr before its removal. Even an osteoma with a wide intraorbital extension can be removed in this way (Fig. 11.10a, b).
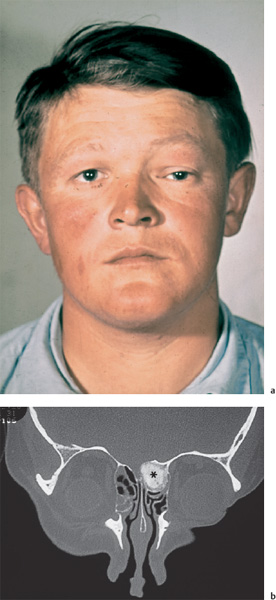
Fig. 11.6 a, b Osteoma of the left anterior ethmoid.
a Lateroinferior displacement of the left ocular bulb causing diplopia.
b Osteoma (*) of a left anterior ethmoid arroding the skull base and medial orbital wall (coronal CT). Endoscopic removal was successful.
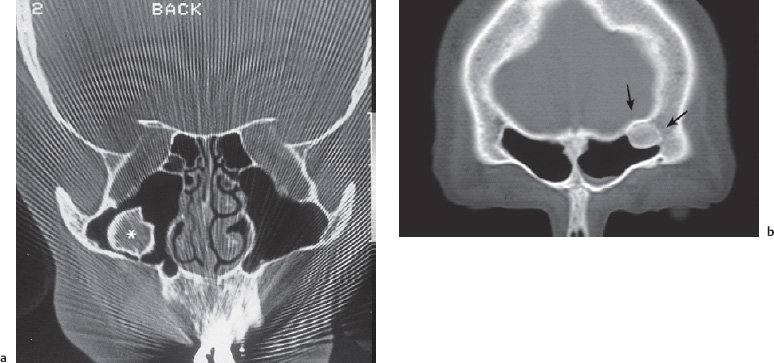
Fig. 11.7 a, b Bone cysts, varieties of osteoma, in the paranasal sinuses (coronal CT).
a Pedicled cyst with bony shell (*) in the right maxillary cavity.
b Broadly based osteoma (arrows) in the lateral recess of a left frontal sinus.
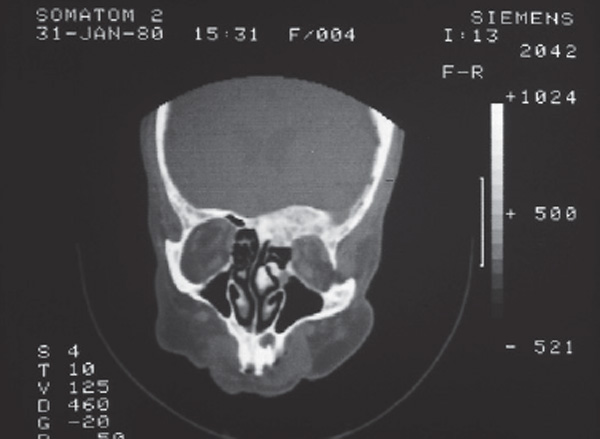
Fig. 11.8 Diffuse growth of bone in the skull base with osteodysplasia (coronal CT).
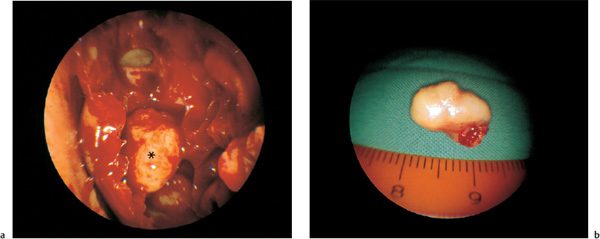
Fig. 11.9 a, b Small osteoma (*) in the typical location of the anterior ethmoid (left side).
a Exposure of an ethmoid osteoma (*) by intranasal partial ethmoidectomy. The left ethmoid has been opened (70° telescope).
b The endoscopically removed specimen (cm scale).
The wound surface can be relied upon to reepithelialize spontaneously because the adjacent healthy mucosa is mostly preserved.
Larger osteomas, if situated in the frontal sinus, are resected by a minimally invasive procedure Schick et al. 2001). Our first choice is a broad frontal sinusotomy from below across the anterior ethmoid. Exposed in this manner, the tumor is fragmented with punch and drill, and can be extracted piecemeal. If the basis of the osteoma stems broadly from the sinus wall, a limited external osteoplastic opening of the cavity is fraised in the lower anterior wall as a portal for the drilling of the tumor under endoscopic control. The mucosa is thus preserved as much as possible. If the frontal sinus infundibulum is compromised by the tumor, its stenotic tunnel is enlarged from both directions under endonasal endoscopic (70° angled optic) guidance from below (see Fig. 6.53). Even larger and widely adherent osteomas can thus be removed with full restoration of the well-ventilated frontal sinus (Fig. 11.11a, b).
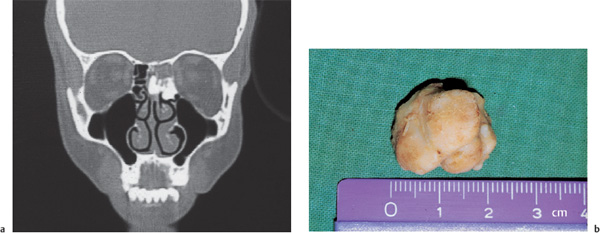
Fig. 11.10 a, b Ethmoid osteoma.
a CT scan before operation.
b The osteoma removed by endoscopy (cm scale).
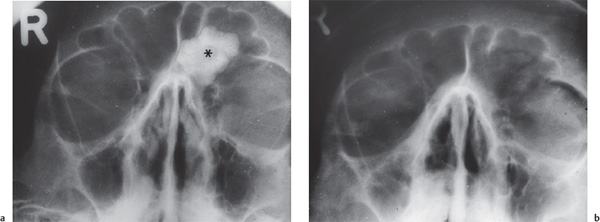
Fig. 11.11 a, b Large, broadly based osteoma (*) of the left frontal sinus not suited for simple endoscopic excision. It was completely removed by a bidirectional two-portal access with endoscopic transnasal and minimal external osteoplastic frontotomy. Frontal radiographs a before and b after surgery, illustrating a reventilated sinus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


