Purpose
To describe clinical outcomes of complications afflicting the autologous oral mucous membrane graft after modified osteo-odonto keratoprosthesis surgery in chronic Stevens-Johnson syndrome (SJS).
Design
Prospective case series.
Methods
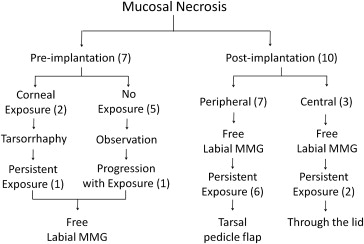
This study included 30 eyes of 30 patients with SJS-induced dry keratinized ocular surfaces; the patients underwent various stages of this procedure between August 2009 and February 2012. Mucosal complications were classified as either necrosis or overgrowth. Mucosal necrosis was managed according to a predesigned algorithm based on timing (pre- and postimplantation) and location (central or peripheral) of necrosis. Cases with mucosal overgrowth underwent mucosal debulking and trimming.
Results
Mucosal necrosis developed in 15 (50%) eyes and overgrowth in 4 (13.3%) eyes. Preimplantation necrosis (n = 7) was initially managed conservatively, but 2 eyes required free labial-mucous membrane grafting for persistent corneal exposure. Free labial-mucous membrane grafting was performed in all cases of postimplantation necrosis (n = 10), but 8 eyes required additional tarsal pedicle flaps (n = 6, for peripheral necrosis) or through-the-lid revisions (n = 2, for central necrosis). Debulking and trimming effectively managed all cases of mucosal overgrowth, but 3 eyes required repeat procedures. At 24.1 ± 6.5 months postimplantation, the keratoprosthesis was retained in all eyes, and the probability of maintaining 20/60 or better vision was similar in eyes with or without mucosal necrosis (86 ± 8.8% vs 80 ± 10.3%).
Conclusions
Mucosal complications, especially necrosis, occurred commonly following modified osteo-odonto keratoprosthesis surgery in dry keratinized post-SJS eyes. The algorithm-based management approach described in this study was successful in treating these complications, retaining the prosthesis and preserving useful vision.
Osteo-odonto keratoprosthesis, developed by Strampelli and modified by Falcinelli, is arguably the best keratoprosthesis available today in terms of both long-term visual performance and anatomic retention rates. Although Boston type 1 keratoprosthesis, with its improved design and postoperative medical regimen, has become increasingly popular in wet eyes with end-stage corneal disease, osteo-odonto keratoprosthesis remains the procedure of choice in completely dry eyes with keratinized ocular surfaces. Alternative keratoprostheses designed for such severe cases of corneal blindness are Pintucchi (dacron-felt) keratoprosthesis, Temprano (osteo) keratoprosthesis and Boston type 2 keratoprosthesis, all of which have poorer retention rates as compared to osteo-odonto keratoprosthesis (88% at 5 years and 81% at 20 years).
Notwithstanding its benefits, the main drawbacks of osteo-odonto keratoprosthesis include the complicated surgical technique, poor cosmetic outcome and difficulty in treating postoperative complications. These factors have often dissuaded both surgeons and patients from performing or undergoing this procedure, respectively. Among its various postoperative complications, those requiring repeated surgical interventions, especially in patients with Stevens-Johnson syndrome (SJS), are those related to the transplanted oral-buccal mucous membrane graft. This study describes the treatment strategies and clinical outcomes of mucosal complications in modified osteo-odonto keratoprosthesis in completely dry post-SJS eyes.
Methods
This prospective case series included 30 eyes of 30 patients who underwent various stages of modified osteo-odonto keratoprosthesis between August 2009 and February 2012. The osteo-odonto keratoprosthesis program was initiated following approval of the ethics committee of L V Prasad Eye Institute, Hyderabad, India, and under the guidance of Professors Giancarlo Falcinelli (Rome, Italy) and Geetha Iyer (Chennai, India), who personally supervised various stages of the procedure in the first four cases. Written informed consent was obtained from all patients before they were included in this study.
Patients
Cases selected for osteo-odonto keratoprosthesis surgery included adult patients (>16 years of age) with: (1) bilateral corneal blindness following an acute episode of SJS; (2) completely dry eye or eyes, defined as Schirmer test scores of 0 with totally keratinized ocular surfaces; (3) best-corrected visual acuity (BCVA) of counting fingers at one meter or less in the better eye; (4) normal posterior segment on ultrasound B scan; (5) intact canine teeth and normal buccal mucosa with oral hygiene deemed adequate for surgery by a faciomaxillary surgeon (active smokers and betel-nut chewers were not selected for surgery); and (6) realistic understanding of the risks and benefits of the procedure as assessed by a clinical psychologist.
Surgical Technique of Modified Osteo-Odonto Keratoprosthesis
The surgical procedure consisted of four stages. In stage 1 ( Supplemental Figure , top row), the cornea was exposed and a complete iridectomy along with cryoassisted intracapsular cataract extraction was performed. In stage 2 ( Supplemental Figure , second row from the top), a 30-mm × 30-mm autologous buccal mucous membrane graft was harvested and sutured onto the exposed ocular surface, the four recti and the conjunctival edges. In stage 3 ( Supplemental Figure , second row from the bottom), a canine tooth with the adjoining bone of the upper jaw was excised and reshaped to fashion the osteodental acrylic lamina into which the optical cylinder of appropriate diopteric power, based on the patient’s axial length, was fitted. This complex was placed in a subcutaneous pouch over the opposite zygoma and left in situ for 8 to 12 weeks. In stage 4 ( Supplemental Figure , bottom row), the osteodental acrylic lamina was retrieved and placed on the eye after lifting the buccal mucosal flap and making a central opening in the cornea. The osteodental acrylic lamina was sutured onto the ocular surface and the buccal mucosal flap was reposited. A central opening was made in the mucosa to exteriorize the optical cylinder. In the first four cases, stages 2-3 and 1-4 were combined as two separate extraocular and intraocular procedures with an intervening gap of 3 months, in accordance with the Rome-Vienna protocol. This was done to facilitate supervision of the procedure by Professors Facilnelli and Iyer.
Mucosal Complications and Management
Problems with the transplanted oral mucosal graft were classified as either mucosal necrosis or overgrowth. Mucosal necrosis was defined as ulceration of the mucosa with exposure of the underlying ocular surface or osteodental acrylic lamina. The possibility of infection was ruled out on the basis of scrapings from the edges and base of the ulcer, which was sent for microbiologic examination (smears and culture). Mucosal necrosis was further classified as preimplantation (after stage 2 but before stage 4) or postimplantation (after stage 4), which was again subdivided into central (around the optical cylinder) or peripheral involvement (around the edges of the osteodental acrylic lamina). The management strategy for eyes with mucosal necrosis is summarized in Figure 1 . This algorithm was developed on the basis of findings in previous studies and discussions with surgeons experienced in osteoodontal keratoprosthesis. In brief, initially all cases of preimplantation necrosis were managed conservatively or by performing a tarsorrhaphy (if the cornea was exposed), but if the necrosis persisted or worsened for two weeks, free labial-mucous membrane grafting was performed. In cases of postimplantation necrosis, surgical intervention was immediate so as to prevent infection or extrusion. Free labial-mucous membrane grafting was done first, and if it failed, a tarsal-pedicle flap for peripheral necrosis and through-the-lid revision for central necrosis was performed.
Mucosal overgrowth was defined as mucosa covering the optical cylinder of the osteodental acrylic lamina. Mucosal overgrowth was managed surgically as soon as it interfered with visual function in the form of blurring of vision or subjective reduction in the patient’s visual field.
Surgical Technique of Free Labial-Mucous Membrane Grafts
The necrotic mucosa was excised, and the margins of the defect were freshened. The extent of the defect was measured by calipers, and a 10%-oversized graft was obtained from the mucosa of the lower lip. This graft was secured, epithelial side up, on the ocular or laminar surface and secured to the underlying tissue with fibrin glue. The margins were then sutured to the adjoining mucosa, conjunctiva, or lid margin with a combination of mattress and interrupted 6-0 polyglactin sutures ( Figure 2 , top row).
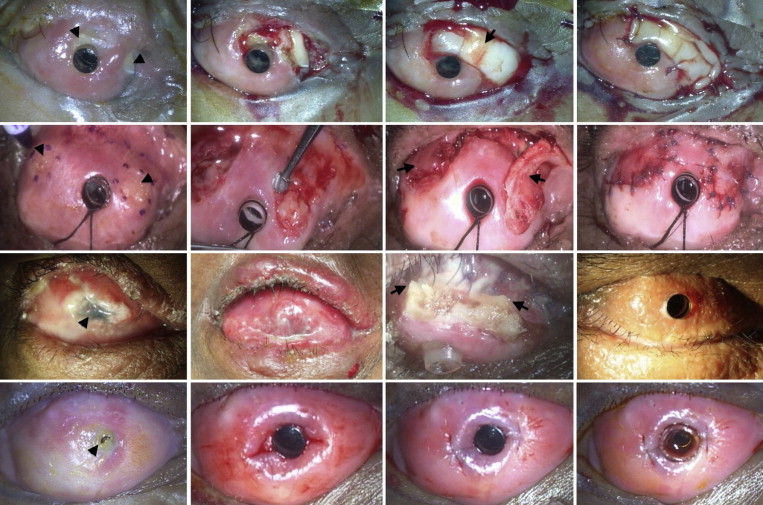
Surgical Technique of Tarsal-Pedicle Grafts
After excision of the necrotic and thinned-out mucosa and freshening of the margins of the defect, any sharp edges or spicules of the underlying bony lamina were smoothened using a dental burr. One or more appropriately sized tarsal-pedicle flaps, hinged at the lid margin, were fashioned by dissecting the posterior lamina of the lid and turned over to cover the defect. These flaps were sutured in place with a combination of mattress and interrupted polyglactin sutures ( Figure 2 , second row from the top).
Surgical Technique of Through-the-Lid Revision
After excision of the necrotic mucosa and freshening of the margins of the defect, the posterior lamella of the upper lid was removed. The anterior lamella of the upper lid, containing the orbicularis and the skin, was pulled over the optical cylinder of the osteodental acrylic lamina to cover the bared area, and the anterior lid margin was sutured to the freshened edge of the remaining buccal mucosal graft using 6-0 polyglactin sutures. The optical cylinder was exposed through the skin after two weeks ( Figure 2 , second row from the bottom).
Surgical Technique of Mucosal Debulking
The excess mucosa covering the cylinder was excised. Two incisions were made through the mucosa, extending 3 mm radially from the cylinder. The submucosal tissue was trimmed using a Vannas scissors in the annular 3-mm zone around the cylinder. The incisions were sutured with interrupted 6-0 polyglactin sutures. A silicone sleeve was placed around the optical cylinder for a week to prevent regrowth of the mucosa over it ( Figure 2 , bottom row).
Postoperative Follow-Up
Patients were followed on day 1, week 1, month 1, and week 6 after each stage of the procedure and every 3 months thereafter or as deemed necessary by the surgeons (SB, VSP). Unless combined, the minimum duration between each stage of the procedure was 6 to 8 weeks. If preimplantation necrosis developed, stage 3 was deferred until at least 6 weeks after the mucosa had completely healed. At each follow-up visit patients underwent a comprehensive ophthalmic examination of both eyes. Following each ocular procedure patients received oral prednisolone (starting at 1 mg/kg of body weight and tapered over 6 weeks); topical ciprofloxacin 0.3% or chloramphenicol 0.5% ointment (thrice daily for one week); and oral acetazolamide tablets for increased intraocular pressure. After every oral surgery, patients received systemic antibiotics for one week and chlorhexidine 0.2% mouthwash for one month.
Data Collection and Analysis
A single investigator (SB) collected the pre-, intra-, and postoperative clinical data in a predesigned spreadsheet at each follow-up visit. Descriptive statistics were used for analysis. Continuous parametric variables were expressed in terms of mean ± standard deviation (SD). Kaplan-Meier survival analysis was performed to determine the probability of retaining BCVA of 20/60 or better over time. A log-rank test was used to analyze the survival probabilities in eyes with or without mucosal necrosis. The Wilcoxon signed rank test was used to analyze the improvement of BCVA over time. A P value less than 0.05 was considered to be statistically significant. All statistical analysis was done using MedCalc version 11.3 for Windows (MedCalc Software, Mariakerke, Belgium).
Results
Demographics
The mean age of the patients was 31.6 ± 12 (range, 17 to 56) years, and the mean duration between SJS and osteo-odonto keratoprosthesis implantation was 5 ± 1.6 (range, 1 to 12) years. The male-to-female ratio was 8:7, and the right-to-left eye ratio was 3:2. Preoperative visual acuity ranged from light perception to counting fingers in all operated eyes. Eleven (36.7%) of the 30 eyes had undergone previous ocular surgeries, including amniotic membrane grafting (n = 9), symblepharon release (n = 4), lid margin mucous membrane grafting (n = 3), tissue adhesive application (n = 3), tarsorrhaphy (n = 2), and unsuccessful parotid duct translocation (n = 2).
Mucosal Necrosis
Mucosal necrosis occurred in 15 (50%) of the 30 eyes. Preimplantation necrosis was seen in 5 eyes, postimplantation necrosis in 8 eyes, and both in 2 eyes ( Figure 1 ). Among the 7 cases of preimplantation necrosis, 5 resolved with scarring, either spontaneously or following tarsorrhaphy, whereas 2 eyes needed supplemental free labial-mucous membrane grafting. Both these eyes also developed central postimplantation mucosal necrosis, underwent repeat labial-mucous membrane grafting that also sloughed off, and ultimately needed through-the-lid revisions. Among the 8 eyes that developed primary postimplantation necrosis, 1 eye each with central and peripheral necrosis had successful resolution with labial-mucous membrane grafting, whereas 6 eyes with peripheral necrosis needed a tarsal-pedicle flap. At a mean follow-up of 24.1 ± 6.5 (range, 12 to 42) months, the prosthesis was retained in all eyes without any recurrence of mucosal necrosis ( Figure 3 ). None of the patients developed any oral mucosal complications. The labial or buccal mucosal wound usually healed completely within one to two weeks, depending on the size of the mucosal graft.





