Purpose
To analyze dome-shaped maculas topographic features and related serous retinal detachment (SRD) in eyes with myopic staphyloma.
Design
Retrospective, observational case series.
Methods
We reviewed the records of 48 eyes in 33 patients with dome-shaped maculas who were referred because of decreased vision. Ophthalmologic examination included axial length measurement, spectral domain optical coherence tomography (OCT), and fluorescein and indocyanine green angiography. The height of the macular bulge was measured, and the choroidal thickness was mapped.
Results
Patient mean age was 55.0 ± 13.6 years. Mean axial length was 27.49 ± 2.53 mm. Mean best-corrected visual acuity (BCVA) was 0.50 ± 0.33 logMAR. Three dome-shaped macula patterns were observed: round dome in 10/48 (20.8%) eyes; horizontal oval-shaped dome in 30/48 (62.5%) eyes; and vertical oval-shaped dome in 8/48 (16.7%) eyes. The mean macular bulge height was 407.7 ± 215.1 μm (120–1130) and was significantly greater in vertical oval-shaped domes. The mean central choroidal thickness (CCT) was 146.5 ± 56.0 μm, significantly greater than at 3 mm nasal and temporal to the fovea ( P < 0.0001). The CCT was positively correlated to macular bulge height but not to BCVA. Foveal SRD was present in 25/48 eyes and significantly increased for macular bulge height greater than 350 μm ( P = 0.0047). BCVA was significantly lower when SRD was present ( P = 0.043).
Conclusions
Most dome-shaped maculas did not display a round but a horizontal or vertical oval-shaped dome and could be missed on a single OCT scan. Chronic foveal SRD was associated with decreased vision and was more common when the macular bulge was highly elevated.
A dome-shaped macula is an entity recently thought to be responsible for vision loss in eyes with myopic staphyloma. The condition was first described in 2008 using optical coherence tomography (OCT) and is characterized by an abnormal convex, anterior protrusion of the macula within the concavity of a posterior staphyloma in myopic eyes. It can be complicated by chronic serous retinal detachment (SRD). The pathogenesis contributing to the development of the dome-shaped macula remains unclear. Several hypotheses have been advanced, such as a resistance to deformation of scleral staphyloma, localized choroidal thickening in the macular area, ocular hypotony, scleral infolding through collapse of the posterior portion of the eye wall, and tangential vitreoretinal traction. More recently, Imamura and associates demonstrated that a dome-shaped macula was associated with a relative localized thickness variation of the sclera under the macula.
Dome-shaped maculas cannot be categorized into any of the types of posterior staphyloma known in myopic eyes, as described by Curtin. Dome-shaped macula diagnostic and prognostic criteria remain inaccurate and have to be clarified. Spectral domain (SD) OCT and three-dimensional (3D) reconstructions of the macula based on SD-OCT images allow precise analysis of the morphology of the macular bulge in a dome-shaped macula. This investigation aimed to analyze the varying clinical presentations of dome-shaped maculas and their topographic features, including the choroidal thickness, as well as the related complications, by using SD-OCT. We also sought to define diagnostic and prognostic criteria.
Methods
The medical records of myopic patients referred because of visual impairment and diagnosed in our high-myopia consultation settings (Lariboisière and Strasbourg) for dome-shaped maculas in one or both eyes were reviewed retrospectively. This study adhered to the principles of the declaration of Helsinki. The ethics committee of the French Society of Ophthalmology did not find any challenges to the medical and scientific rules of ethics as accepted in France, and it approved this retrospective review of patient records.
Exclusion criteria were the presence of an inferior staphyloma (type V staphyloma, according to the Curtin classification ) alone or associated with a tilted disk in which the macula lay on the edge or slope of the inferior staphyloma. Eyes with media opacity preventing detailed imaging or histories of macular choroidal neovascularization (CNV), other macular disease (foveal schisis, full-thickness macular hole or lamellar macular hole), or retinal surgery were also excluded.
Between October 2010 and September 2012, all affected patients had undergone at least one complete ophthalmologic examination that included best-corrected visual acuity (BCVA) assessment using Snellen visual acuity charts, slit-lamp examination of the anterior segment, fundus biomicroscopy, color fundus photography, enhanced depth imaging (EDI) SD-OCT, and fluorescein and indocyanine green angiography. The last three techniques were obtained for all patients using the Spectralis HRA + OCT (Heidelberg Engineering, Heidelberg, Germany). OCT examination was performed in both eyes of each patient as follows: a 10 mm horizontal and vertical SD-OCT scan centered on the fovea; a raster of 7 horizontal EDI-SD-OCT lines within a 5 × 20-degree rectangle centered on the fovea, each line being composed of 100 averaged scans; and a macular map composed of 25 horizontal SD-OCT lines, with a minimum of 9 averaged scans for each line, in a 20 × 20-degree square centered on the fovea. In 15 eyes, OCT was also recorded on the Cirrus HD-OCT (Carl Zeiss Meditec, Dublin, California, USA) with multiple maps arranged in a montage covering the posterior pole in some cases. The axial length of the eye was measured using partial optical coherence interferometry (IOL-Master, Carl Zeiss Meditec, Jena, Germany). Original refractive errors were identified in the eyes with histories of cataract or refractive surgery.
Dome-shaped macula diagnosis was based on the presence of a convex elevation of the retina, retinal pigment epithelium (RPE) and choroid within the concavity of a posterior staphyloma in at least one axis, on either horizontal or vertical, on SD-OCT scans. Various dome-shaped macula profiles were included. A typically dome-shaped macula is characterized by a macular elevation within a posterior myopic staphyloma. The macular curvature is convex, that is, opposite from the normal curvature of the posterior pole, in both horizontal and vertical axes. We have extended this definition to cases in which the elevation was asymmetric with a main axis either horizontal or vertical, then splitting the posterior staphyloma into two parts. In all cases, the macular curvature was clearly convex in at least one axis.
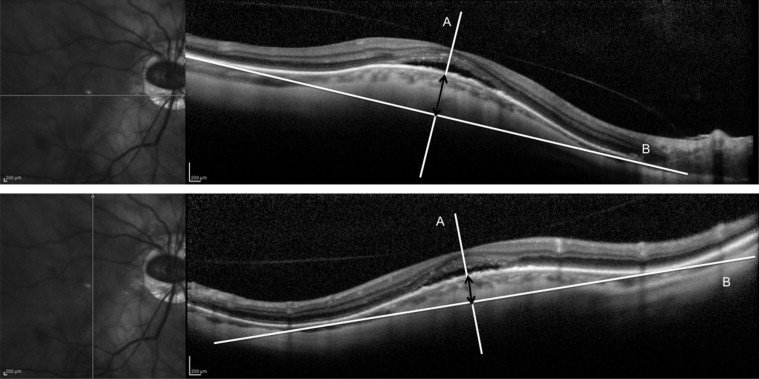
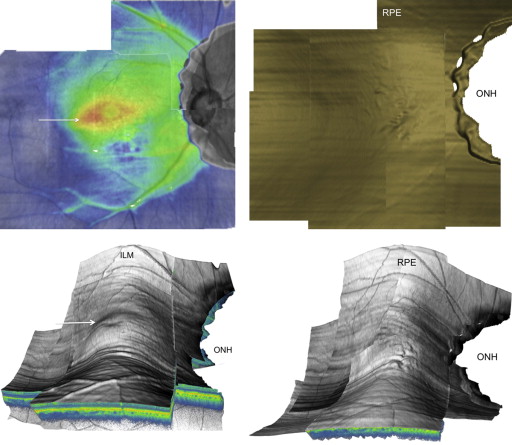
Two aspects have been specifically studied on SD-OCT: the macular bulge height and the orientation of the main axis of the bulge. The macular bulge height relative to the bottom of the staphyloma was measured on horizontal and vertical SD-OCT scans by using the caliper tool of the Spectralis between the outer border of the RPE at the fovea and the line tangent to the outer border of the RPE at the bottom of the staphyloma. We drew a line (A) passing through the center of the fovea and perpendicular to a line (B) tangent to the outer border of the hyper-reflective line corresponding to the RPE at the bottom of the posterior staphyloma. The bulge height was defined as the distance between the intersection of line (A) with the outer border of the RPE and the intersection of line (A) with line (B) ( Figure 1 ). When the macular curvature was not symmetric in the vertical and horizontal axes, the main axis of the bulge was defined as the less convex curvature. The topography of the macular bulge was analyzed on horizontal and vertical SD-OCT scans and on the 3D macular map reconstruction based on SD-OCT images.
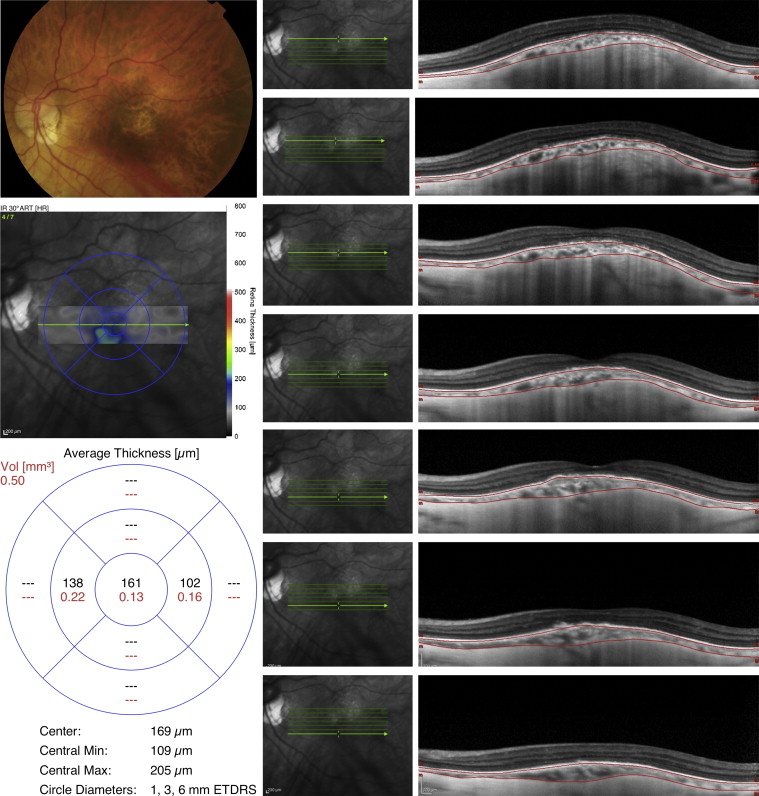
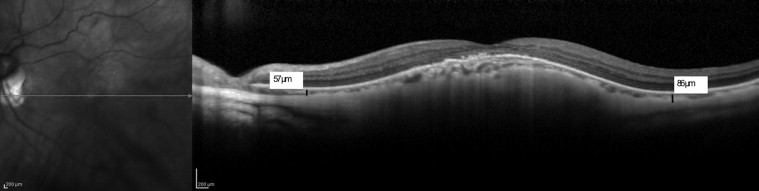
For each eye, a map of choroidal thickness was created manually using the 7-EDI-SD-OCT–line raster (240 μm spacing), allowing for measurement of the mean choroidal thickness within a 5 × 20-degree rectangle centered on the fovea. The choroid was delimited manually by 2 lines on each of the seven EDI-SD-OCT lines, using the Spectralis linear measurement tool: 1 line passed through the outer border of the RPE and the other through the inner scleral border. The sclera was identified on EDI-SD-OCT scans as a highly reflective multilaminar and avascular layer beneath the choroid ( Figure 2 ). Choroidal thickness was also measured at 3000 μm nasal and temporal to the fovea, by using the caliper tool of the Spectralis viewer. Choroidal thickness was defined as the vertical distance between the RPE layer and the sclera ( Figure 3 ).
The presence of a foveal SRD on horizontal and vertical SD-OCT scans was recorded for each eye.
Results are presented as mean ± standard deviation (range). Parametric tests were used when Gaussian conditions were observed; otherwise nonparametric tests were preferred. Statistical software programs were used: GraphPad InStat 3.10 (2009) and Statview 5.0 (SAS Institute Cary, North Carolina, USA, 1998). A P value less than 0.05 was considered significant.
Results
Population Characteristics
In the study we included 48 eyes with dome-shaped maculas in 33 myopic patients. The patients’ mean age was 55.0 ± 13.6 years (range, 26 to 89). The condition was bilateral in 15 of 33 (45.5%) patients. Patient characteristics are summarized in Table 1 . Of the 33 patients, 25 (76%) were female. The mean spherical equivalent refractive error of the eyes studied was −10.54 ± 5.15 diopters (D) (range, −1.50 to −21.5). Axial length measurement was available for 32 eyes. Mean axial length was 27.49 ± 2.53 mm (range, 23.73 to 32.70). Median BCVA was 20/50 (mean logarithm of the minimum angle of resolution [logMAR] BCVA: 0.50 ± 0.33 [range, 0 to 1.30]).
| Number of eyes/Number of patients | 48/33 |
| Sex | 25 females/8 males |
| Age (years) | 55.0 ± 13.6 (26 to 89) |
| Axial length (mm) | 27.49 ± 2.53 (23.73 to 32.70) |
| Best-corrected visual acuity (logMAR) | 0.50 ± 0.33 (0 to 1.30) |
| Spherical equivalent refractive error (diopters) | −10.54 ± 5.15 (−1.50 to −21.5) |
| Macular bulge height (in the most cambered axis) (μm) | 407.7 ± 215.1 (120 to 1130) |
| Central choroidal thickness (μm) | 146.5 ± 56.0 (53 to 267) |
| Mean choroidal thickness at 3000 μm nasal to the fovea (μm) | 87.6 ± 35.2 (51 to 286) |
| Mean choroidal thickness at 3000 μm temporal to the fovea (μm) | 102.0 ± 50.5 (56 to 287) |
| Presence of foveal SRD | 25/48 (52.1%) |
Dome-Shaped Macula Patterns
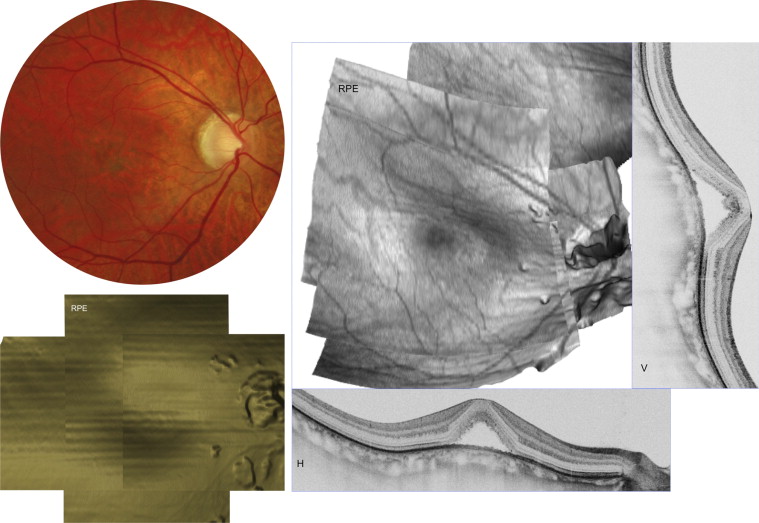
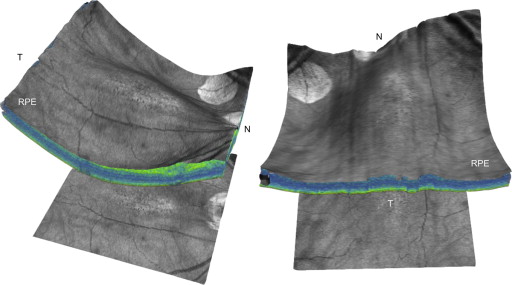
On fundus biomicroscopy, all patients exhibited a posterior staphyloma resembling Curtin type I or II but modified by the presence of the macular bulge. The analysis of horizontal and vertical OCT scans as well as the 3D reconstruction of the macular area on the Spectralis or the Cirrus SD-OCTs allowed differentiation among 3 dome-shaped macula patterns. The first dome-shaped macula pattern was a typical round dome in a Curtin-type I or II staphyloma and was observed in 10 of 48 eyes (20.8%). The macular elevation was grossly symmetric in both horizontal and vertical axes and was surrounded in all directions by the staphyloma ( Figure 4 ). The second dome-shaped macula pattern consisted of a roughly horizontally oriented oval-shaped dome splitting a staphyloma into two parts, superior and inferior, and was observed in 30 of 48 eyes (62.5%). The vertical axis was the most cambered on SD-OCT, and the horizontal axis was either slightly convex or flat. In some cases, the nasal edge of the horizontal bulge either reached the optic disk edge or plunged down in the peripapillary conus ( Figure 5 ). The third dome-shaped macula pattern consisted of a vertically oriented oval-shaped dome splitting the staphyloma into two parts, temporal and nasal, and was observed in 8 of 48 eyes (16.7%). The horizontal axis was the most cambered on SD-OCT, and the vertical axis was either slightly convex or flat ( Figure 6 ). These last two patterns share a common characteristic: their oval-shaped dome splits the staphyloma into two parts. In all cases, the macular curvature was clearly convex in at least one axis. The characteristics of the three dome-shaped macula patterns are reported in Table 2 .
| Dome-shaped macula pattern | Central round dome | Horizontally oriented oval-shaped dome | Vertically oriented oval-shaped dome |
|---|---|---|---|
| Number of eyes | 10/48 (20.8%) | 30/48 (62.5%) | 8/48 (16.7%) |
| Sex | 7 females/2 males | 17 females/5 males | 6 females/2 males |
| Age (years) | 50.9 ± 11.6 | 57.4 ± 14.7 | 51 ± 6.2 |
| Spherical equivalent refractive error (diopters) | −10.35 ± 4.95 | −11.56 ± 4.78 | −7.31 ± 5.86 |
| Axial length (mm) | 27.02 ± 2.48 | 27.86 ± 2.38 | 26.57 ± 3.58 |
| Best-corrected visual acuity (logMAR) | 0.53 ± 0.29 | 0.46 ± 0.35 | 0.63 ± 0.32 |
| SD-OCT characteristics | Both horizontal and vertical scans show a grossly symmetric, convex macula | Vertical scan shows a clearly convex macula; horizontal scan shows a slightly convex or flat macula | Horizontal scan shows a clearly convex macula; vertical scan shows a slightly convex or flat macula |
| SD-OCT 3D reconstruction characteristics | Round dome macular elevation surrounded in all directions by the staphyloma | Oval-shaped macular elevation splitting the staphyloma into 2 parts: superior and inferior | Oval-shaped macular elevation splitting the staphyloma into 2 parts: nasal and temporal |
| Macular bulge height (in the most cambered axis) (μm) | 326.6 ± 120.7 | 343.6 ± 129.5 | 749.6 ± 248.8 |
| Central choroidal thickness (μm) | 155.8 ± 57.5 | 131.3 ± 50.2 | 184.3 ± 59.2 |
| Presence of foveal SRD | 6/10 (60%) | 12/30 (40%) | 7/8 (87.5%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


