Mooren’s Ulcer
C. Stephen Foster
Bowman first described what we now call Mooren’s ulcer of the cornea (also known as chronic serpiginous ulcer and ulcus rodens) in 1849 (1). Mooren published cases describing the disorder in detail and establishing it as a distinct clinical entity in 1867 (1). Mooren’s ulcer is a painful, relentlessly progressive chronic ulcerative keratitis that begins peripherally and progresses circumferentially and centrally. It is, by definition, idiopathic, occurring in the absence of any diagnosable systemic disorder associated with peripheral ulcerative keratitis (PUK). Its exact pathophysiology remains uncertain. Advances have been made in better understanding the etiopathogenesis and in the management of this disorder, but a significant percentage of cases remain refractory to available therapies and result in severe visual morbidity.
EPIDEMIOLOGY
Mooren’s ulcer is uncommon. Lewallen and Courtright’s (2) review of 20 published series of Mooren’s ulcer numbered 187 patients. Some of the cases in the published series are probably cases of PUK in patients with occult systemic diseases such as rheumatoid arthritis (RA), Wegener’s granulomatosis (WG), relapsing polychondritis (RP), or polyarteritis nodosa (PAN), judging from the scleral involvement of some of the cases (Mooren’s does not result in necrotizing scleritis).
Wood and Kaufmann (3) have concluded, based on their review of the literature and a study of their own patients, that there were two distinct clinical types of Mooren’s ulcer: unilateral, with mild to moderate symptoms, generally responding well to medical and surgical therapy, and often occurring in older patients (typical or benign Mooren’s ulcer), and a more malignant, bilateral form with more pain and poor response to local medical and surgical therapy. This second type tends to occur in younger patients.
Mooren’s ulcer is bilateral in 25% of the benign type and in 75% of the malignant type (4,5). Keitzman (6) published a series of 37 cases of Mooren’s ulcer primarily in Nigerian men in their 20s and 30s. A later report confirmed the frequent occurrence of the “malignant” form in young Nigerian men (7). As a result of these reports, it is commonly believed that the progressive and relentless atypical form of Mooren’s ulcer has a predilection for young black men.
Lewallen and Courtright (2), however, in their review of the published series on Mooren’s ulcer, suggest that these concepts about the epidemiology of Mooren’s ulcer are not supported by the available data. For example, they found that 43% of older patients had bilateral disease, whereas bilateral disease was present in only one third of patients younger than 35 years. Also, whites were more than twice as likely to have bilateral disease than blacks. Although they found that men were 1.6 times more likely to have Mooren’s ulcer than were women, the authors point out that this may be attributed to factors such as increased incidence of ocular trauma in men (an association with Mooren’s ulcer is reported) or cultural patterns that discourage female clinic attendance in certain countries, and that this finding may not reflect a true biologic propensity for men.
Lewallen and Courtright (2) conclude that the available data are flawed by a collection period spanning more than 85 years, differences in the criteria for definition of the disease, poor documentation and follow-up, and problems inherent in non-population-based data collection, in 20 series from more than 14 different countries. Lewallen and Courtright do not suggest that their own statistical analysis is necessarily accurate either.
CLINICAL FEATURES
Patients with Mooren’s ulcer complain of painful, red, tearing, photophobic eye. The pain is often incapacitating and may seem out of proportion to the inflammation noted on examination. Vision is affected secondary to associated iritis, central corneal involvement, or irregular astigmatism from peripheral corneal thinning.
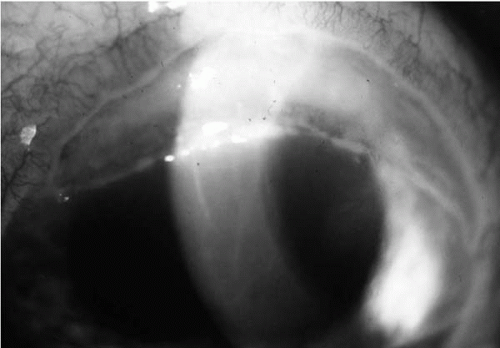
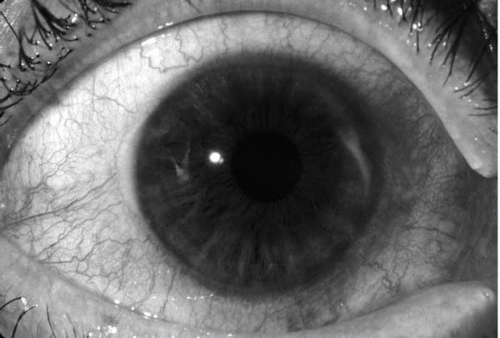 FIGURE 24-1. Early stage of Mooren’s ulcer, with an inflammatory infiltrate in the anterior corneal stroma, 2 o’clock periphery, with associated conjunctival injection but without scleritis. |
The first notable pathosis may be patchy, peripheral stromal infiltrates, which then coalesce, more often in the medial and lateral quadrants than in the superior and inferior ones. An epithelial defect and shallow furrow then develop. The tissue destruction extends to the limbus (unlike the keratitis infiltrate typical of staphylococcal hypersensitivity marginal keratitis) (Fig. 24-1), but not past the limbus, into the sclera (unlike the PUK so often seen in association with RA, PAN, WG, and RP) (Fig. 24-2) (5,8). The ulcer spreads circumferentially, posteriorly (deeper and deeper toward Descemet’s membrane), and centrally to involve the entire cornea eventually. The anterior half, or more, of the stroma is involved, and one curious, semidiagnostic feature occurs early in the process: the undermined edge of the irregularly scalloped (as if eaten by a rat, hence ulcer rodens) central edge of the ulcer (Fig. 24-3). This same PUK morphology can occur in the eye as a consequence of RA, RP, PAN, or WG, and hence the importance of including these systemic (potentially lethal) diseases in the differential diagnosis of suspected Mooren’s PUK. But these latter disorders generally (eventually) also produce significant scleral damage, and also (eventually) reveal other clinical or laboratory abnormalities that make clear the systemic diagnosis.
The extent of the corneal damage is almost always far greater than is obvious during slit-lamp biomicroscopy examination. The depth to which the matrix metalloproteinase enzymatic degradation of the corneal collagens and glycosaminoglycans has extended may be relatively obscured by the so-called overhanging lip or edge of the anterior-most cornea at the edge of the active PUK, with the anterior-most lamellae of the cornea infiltrated slightly with neutrophils, but not yet dissolved, and so “flopping” down onto and covering from view the deep gutter portion of the PUK. Indeed, even the application of 2% fluorescein dye to the ocular surface may produce the misleading finding of an “intact” surface, with simply a fine, thin line of fluorescein dye that has trickled into the gutter, fluorescing. But even more shocking, even to the corneal specialist who has evaluated one or more patients with Mooren’s ulcer previously, is the extraordinary extent of stromal digestion central to the PUK gutter, beginning at the gutter base. A fine probe (such as one tine of a Tubingen-Harms tying forceps) gently exploring the extent of damage central to the PUK gutter always discloses a cleavage plane in the stroma, with easy passage of the probe 1 to 4 mm into what clinically appeared to be normal cornea.
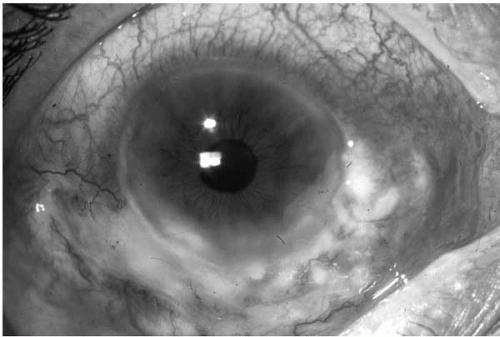 FIGURE 24-2. Example of peripheral ulcerative keratitis (PUK) in a patient with Wegener’s granulomatosis, with associated adjacent scleritis, obviously very different from the characteristics of Mooren’s ulcer shown in Fig. 24-1.(see color image) |
The damaged cornea peripheral to the advancing edge of the active, progressing ulcer is thinned as a consequence of the stromal digestion during the ulcer’s active phase, but it reepithelializes, scars, and vascularizes, and generally (unless traumatized) does not perforate (although it can) (Figs. 24-4 and 24-5). This destructive inflammatory process progresses until (a) effective therapy stops it, or (b) the entire geographic extent of the cornea has been involved, at which
point inflammation and pain subside, leaving the patient with a thinned, scarred, vascularized cornea and poor vision.
point inflammation and pain subside, leaving the patient with a thinned, scarred, vascularized cornea and poor vision.
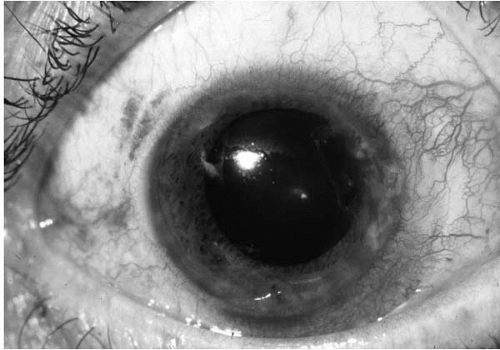 FIGURE 24-4. Vascularized, thinned peripheral bed of previously ulcerating cornea in a patient with PUK caused by Mooren’s ulcer; note the area at approximately 2 o’clock.(see color image) |
The conjunctiva, episclera, and sclera may be edematous and inflamed in areas adjacent to active corneal inflammation. Iritis may be present, but hypopyon is rare unless secondary infection occurs. Glaucoma and cataract may complicate matters. Perforation has been noted in up to 36% of cases, especially if there is minor trauma to the weakened cornea (8).
ASSOCIATIONS AND PROPOSED ETIOLOGIES
Various entities have been associated with Mooren’s ulcer, often leading to conjecture that there may be a causal relationship. In Nigeria, there has been an association with helminthiasis; four of five cases were so associated in one series (7). Another study suggested that the progression of the ulcerative keratitis was arrested by local therapy in combination with systemic therapy for the parasitic infection (6). Schanzlin (9) has proposed a causal relationship, suggesting that helminth toxins or antigens deposited in the cornea may lead to antigen-antibody reactions or that infection may cause alteration of the host immune system, allowing the keratitis to occur. But helminthiasis is epidemic among the population involved in these studies and Mooren’s ulcer is extremely rare, even in these populations.
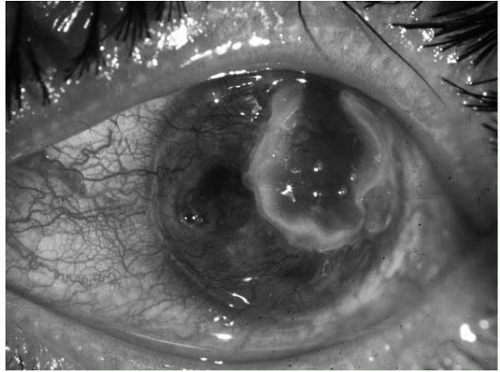 FIGURE 24-5. A more advanced example of progressive Mooren’s ulcer, with only a small residual area of remaining full-thickness cornea, with the infiltrated edge of the overhanging lip, and a vascularized, thinned residuum of cornea left in the wake of the advancing ulcer.(see color image) |
Chronic hepatitis C infection was documented in two patients with bilateral Mooren’s ulcers (12). The keratitis in both patients improved after treatment of the hepatitis with interferon-α2b. The authors propose that molecular mimicry may be involved, with the hepatitis C virus stimulating an autoimmune response to corneal antigens through cross-reacting epitopes. Alternately, they also propose that deposition of immune complexes in the limbal or peripheral corneal tissues may lead to an immune response and the release of proteolytic enzymes. Hepatitis C virus-associated vasculitis is a well-recognized entity, and careful analysis of biopsy specimens from conjunctiva and episclera adjacent to the PUK of patients with hepatitis C-associated Mooren’s ulcer should settle the matter of this latter hypothesis. Chronic hepatitis C infection is not rare, and, if a causal relationship is present, Mooren’s ulceration would be expected to be seen more frequently. Other infections that have been associated with Mooren’s ulcer have included syphilis, tuberculosis, and salmonella (11).
Mooren’s ulcer has also been reported following corneal disease. Specific associations include physical trauma (3), foreign body (12), chemical burn (15), herpes simplex infection (14), herpes zoster infection (15), and surgical procedures such as cataract extraction and penetrating keratoplasty (16,17). Some of these may not represent true cases of Mooren’s ulcer; if they do, definitive associations and causal relationships have not been demonstrated.
PATHOPHYSIOLOGIC FEATURES
The exact pathophysiologic mechanism of Mooren’s ulceration remains unknown, but there is much evidence to suggest that it is an autoimmune process, with both cell-mediated and humoral components. Plasma cells (18), neutrophils (19), mast cells, and eosinophils (18,20) have been found in the involved areas (21). Brown (18) demonstrated high levels of collagenase in the affected conjunctiva. And we found numerous activated neutrophils in the ulcerating cornea, and proposed that the neutrophils are the source of the proteases and collagenases (19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree