Class I—one subsite of the oropharynx, no adverse features
Class II—involves more than one subsite, no adverse features
Class III—only one subsite, adverse features
Class IV—involve more than one subsite, adverse features
Subsites of the oropharynx: base of tongue, tonsil, soft palate
Adverse features: carotid artery exposure, communtication with the neck, >50 % soft palate resection
Table 1 Illustration I CORD Classification System for TORS defects
Table 2
Structural and functional considerations of TORS reconstruction
Structural Considerations |
Create an anatomic barrier between the neck and the pharynx |
Carotid artery coverage |
Functional Considerations |
Restore swallowing function |
Preserve speech and articulation |
Prevent aspiration |
Maintaining velopharyngeal competence |
Class I defects include any single subsite of the oropharynx without any complicating features such as carotid artery exposure, pharyngocervical communication, or extensive palatal defect. The majority of these defects are typically left to remucosalize secondarily and often do so with minimal functional morbidity (Fig. 1). For tongue base defects, exposed deep intrinsic tongue muscles serve as the vascularized bed for remucosalization. Posterior pharyngeal defects wherein the prevertebral fascia is exposed, mucosa will reline the area within several weeks. After pharyngectomy, fat from the parapharyngeal space provides vessel coverage and a surface for epithelialization (Fig. 2). Small defects of the palate, however, may require a series of sutures to close the free edge of the remaining palate to the posterior pharyngeal wall, thus closing the enlarged nasopharyngeal aperture. The goal of this technique is to minimize velopharyngeal insufficiency to improve speech and swallowing.

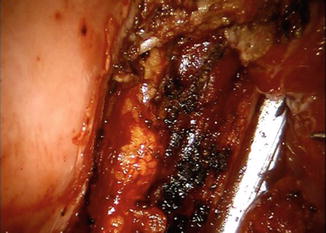

Fig. 1
Class I defect involving only one subsite of the oropharynx (tonsil) with no complicating defects
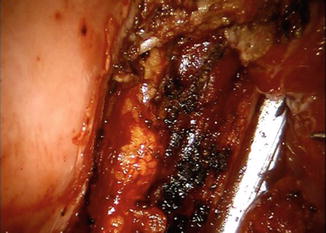
Fig. 2
Parapharyngeal fat outpouching from the lateral pharyngeal wall after TORS resection (blue arrow)
Seikaly et al. described reconstruction of the palate using a size-based classification system with defects classified into one of three categories [14]. For defects of less than one-fourth of the palate, they suggest primary closure of the palate to the posterior pharyngeal wall. In their series of 22 patients with small defects closed primarily, only one patient complained of nasopharyngeal regurgitation at 1 year after operation. In the same cohort, one patient remained gastric tube dependant and three required nutritional supplementation.
Class II defects are similar to class I defects in that they have no complicating features; however, they are more advanced in that more than one subsite is involved. Rarely do class II defects require a regional or free flap for reconstruction. Defects involving the tongue base extending into the tonsil are often left to heal secondarily. For defects of the tonsillar–palatal complex, a local musculomucosal flap may be used to seal the nasopharyngeal port. This flap is typically based on the mucosa and the superior constrictor muscle of the posterior pharyngeal wall. A monopolar cautery or contact laser is typically mounted in one of the robotic arms and used to raise this flap in the submuscular plane carefully to avoid potential injury to the internal carotid artery. This flap can then be rotated toward the posterior edge of the palate and sutured in order to reduce the size of the nasopharyngeal port. This technique has been previously described by Gehanno [29] and has also been referred to as a superior constrictor advancement rotation flap. The advantage of this local flap is that it is theoretically a neurotized flap and can preserve the dynamic function of the constrictor muscles during swallowing.
Class III defects were classified as those that involved one subsite of the oropharynx, but had adverse features such as internal carotid artery exposure in the pharynx, communication with the neck, or >50 % soft palate resection (Fig. 3). Class IV defects involved multiple subsites of the oropharynx and one or more of the adverse features mentioned in Class III (Table 1). We advocate regional or free flap reconstruction for class III and class IV defects or smaller defects in patients who have received prior radiotherapy. In a recent review of 92 patients TORS patients at Mount Sinai Medical Center the majority of the patients fell in the Class II category (n = 45, 49 %), while Class I, III and IV defects were 34 % (n = 31), 3 % (n = 3), and 14 %(n = 13), respectively [30].
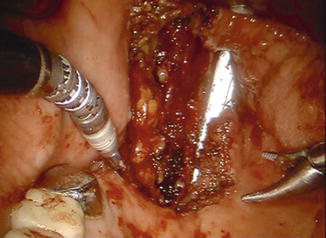
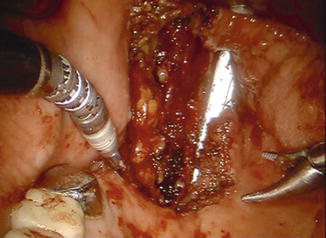
Fig. 3
Class 3 defect involving a portion of the soft palate, the tonsil, base of tongue. This patient also had communtication with the neck after the TORS resection
Rationale and Goals of Transoral Robotic Surgery Assisted Microvascular Reconstruction
Pharyngocervical Communication
When TORS is performed with a concomitant neck dissection, a pharyngocutaneous fistula may develop inadvertently or as part of the planned resection. A recent study by Moore and colleagues showed that 29 % of patients had a pharyngocervical communication intraoperatively, while only 4 % of these developed a permanent communication [31]. While some have advocated for a staged neck dissection to reduce the risk of fistula formation, tumors invading through the pharyngeal constrictor muscles may require a resection resulting in a surgically created fistula. Several techniques have been advocated for management of a fistula in the acute setting; however, in large defects or in patients who have received previous external beam radiotherapy, regional or free tissue transfer may represent the only reliable method of reconstruction. Flap reconstruction may be accomplished with the use of local flaps such as the infrahyoid or sternocleidomastoid muscle flap (Fig. 4a, b) or the submental island flap (Fig. 5) [32, 33]. Irrespective of the technique used to reconstruct the defect it is important to separate the upper aero digestive tract from the neck, to prevent postoperative fistula and vascular complications associated with the great vessels of the neck.
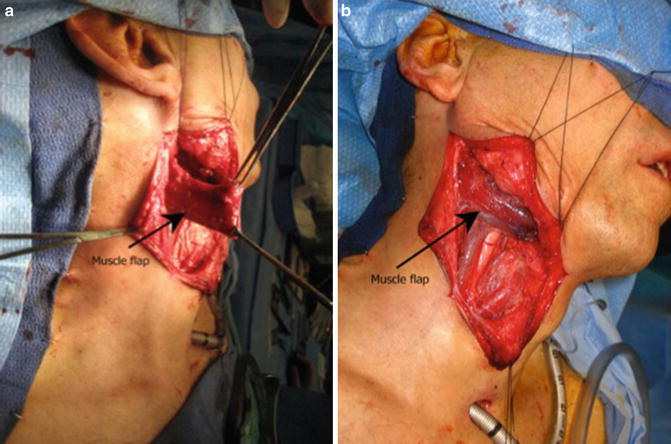

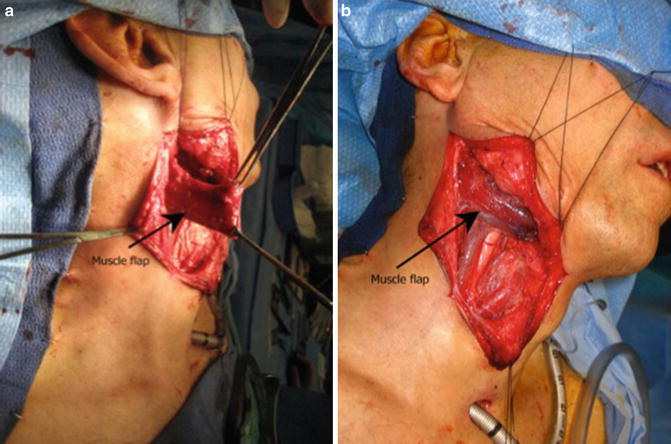
Fig. 4
(a) Sternocleidomastoid muscle flap raised in the neck for inset into the oropharynx. (b) Sternocleidomastoid muscle flap positioned in the neck to reinforce the robotic defect

Fig. 5
Pedicled submental island flap for oropharynx reconstruction after a TORS resection
Carotid Artery Exposure
Rupture of the carotid artery is a well-known complication following surgery when the great vessels are exposed to salivary contaminants and or in the setting of prior external beam radiotherapy. It can occur in 3–14 % [34, 35] of patients after oropharyngeal surgery. In most cases of tonsil cancer resection, the parapharyngeal fat is left in place protect the carotid artery and provide a vascularized surface or remucosalization. In advanced cancers of the pharynx, the fat pad may require resection resulting in exposure of the carotid artery. In such cases, it is important to provide coverage and protection of the great vessels. A recent survey of TORS surgeons across the United States revealed the rate of postoperative hemorrhage ranges between 2.5 and 4.5 % in a total of 2015 reported procedures. They also reported 6 deaths within 30 days after TORS, all from hemorrhage related to the surgery [36]. While the majority of these events are likely related to branches of the external carotid the importance of vessel coverage cannot be underestimated.
Extensive Palatal Defects
Defects of the soft palate that involve more than 50 % of the soft palate represent a unique functional problem [26]. It has been shown that such defects of the soft palate result in high rates of velopharyngeal insufficiency, dysphagia, and a compromise in quality of life [37]. These defects often require a velopharyngoplasty in addition to soft tissue reconstruction. The velopharynoplasty can typically be achieved using a posterior-based musculomucosal flap that is approximated with the cut edge of the soft palate. The soft tissue reconstruction is best achieved with a regional or free tissue transfer to provide the appropriate soft tissue coverage. This is approach has proven effective in reestablishing speech and swallowing [14].
Radiotherapy
The impact of external beam radiotherapy on wound healing has been well documented. In patients who have undergone prior external beam radiotherapy, transoral robotic salvage surgery can be fraught with complications if the surgical defect is not managed appropriately [38]. Because the tissue has been compromised and the wound healing is suboptimal, free tissue transfer provides an opportunity to interpose well-vascularized tissue into the defect. This approach is been shown safe and effective for the management of these complex wounds [39]. In contrast to the extensive defects described previously, we advocate the use of free tissue transfer for modest defects of the pharynx because of the high risk of fistula, great vessel exposure, and catastrophic complications. In our experience, failure to reconstruct these patients with free tissue transfer leads to adverse scarring, are high risk of fistula formation, and significant compromise and decreased functional performance.
Surgical Technique
TORS-assisted microvascular reconstruction requires planning and a coordinated effort. Preoperative assessment is important in anticipating the defect. The use of gadolinium-enhanced MRI as well as contrast-enhanced CT scan may be necessary to assess the extent of tumor involvement of the oropharynx. In patients undergoing salvage surgery after radiotherapy, we start by selecting the optimal donor site in the event that a comples reconstruction is required. In most cases, the radial forearm donor site provides a source of thin and pliable tissue that can be manipulated to achieve the native contouring of the oropharynx. In select cases the anterolateral thigh or lateral arm donor sites may be appropriate. Most importantly, preoperative coordination the instrumentation and room set up is critical. Ideally a large OR should be utilized to provide space for robotic and microscopic instrumentation, and we have noted that when bringing the microscope into the room after resection of the primary tumor, neck dissection, and identification of the donor vessels while the flap harvest is already underway provides better logistical use of the OR space and prevents congestion. For large tumors, we perform the superior mucosal incisions around the tumor with the robot and in combination with a transcervical pharyngotomy with the inferior mucosal incisions while palpating the tumor in order to achieve safe inferior mucosal and deep margins. If a combined transcervical approach is warranted, we then remove the patient from suspension and proceed with neck dissection, mobilization of the hypoglossal nerve, and transcervical pharyngotomy with completion of the inferior resection.
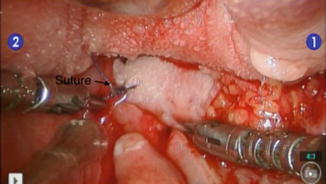
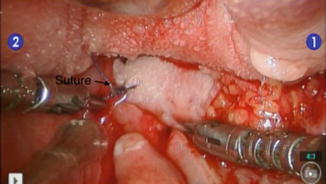
After flap harvest and obtaining negative mucosal margins, the inset is performed. Defects that are confined to the soft palate and the tonsil can be closed transorally with traditional transoral or robotic techniques the majority of the time. However, as the defect extends inferiorly into the base of tongue, the glossotonsillar sulcus, and the pharyngeal wall at the level of the pyriforms sinus, the robotic instrumentation becomes essential for visualization and water-tight closure of the defect. It should be noted that once the tumor has been excised, we place two to four sutures at the inferior apex of the defect in order to use them as a guide for the most inferior edge of the mucosa were the flap needs to be sutured for a water tight closure. Commonly, these sutures are placed transcervically to achieve a reliable distal mucosal closure. If the defect is very inferior, we recommend placing the initial two or three sutures transcervically and then pushing the flap into the defect. This will allow for positioning of the vascular pedicle as it is tunneled into the neck as well. The robot is then brought into place and the patient is suspended. If we decide that the defect can be closed with the robot completely then using a 30° camera, the caudal aspect of the flap can be sutured to the adjacent native tissue of the hyopharynx (Fig. 6). Then, complete inset of the flap is performed before microvascular anastomosis. Robotically placed sutures should be trimmed to avoid tangling with instrumentation, which complicates robotic knot throwing. In tight spaces, urologic needles may be used which have a smaller radius and aid dramatically in robotic suturing.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


