Microbiology of ENT Infections
Manjusha Narayanan
Microorganisms that cause human infections
Infections in the human body can be caused by microorganisms present in the endogenous environment (e.g. microorganisms colonizing the host’s skin, respiratory tract, and the gut, considered to be normal flora) or in the exogenous environment (e.g. fomites, food, water, cross infection from humans or animals). They can be broadly classified as shown in Table 2.1, but infections relevant to ENT are mostly bacterial, fungal, or viral in nature.
Table 2.1 Classification of microorganisms | |||
|---|---|---|---|
|
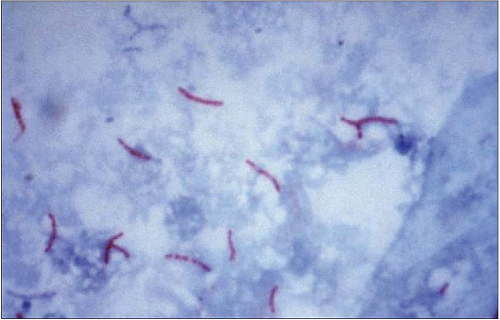
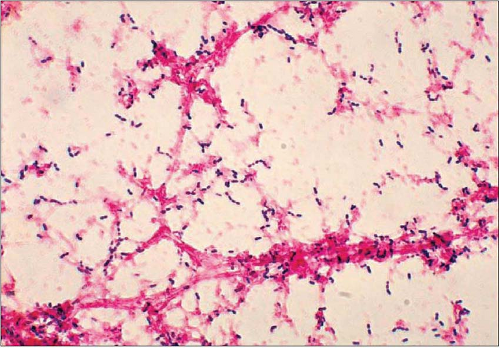
In the laboratory, for simple preliminary identification, bacteria are classified into gram-positives and gramnegatives microscopically, based on the staining characteristics of their cell walls (2.1, 2.2). Cell walls of gram-positive bacteria are thicker and retain the colour of the blue dye crystal violet, whereas gram-negative bacteria with a thinner but more complex cell wall lose the blue dye and take the colour of red or pink counterstain (e.g. safranin). Yeasts and moulds are gram-positive on gram stain (2.3, 2.4) and can also be identified by various other stains microscopically.
 2.1 Gram stain shows gram-positive (blue) lanceolate diplococci belonging to Streptococcus pneumoniae. Gram-positive cocci in chains are usually streptococci. |
 2.2 Gram stain showing Fusobacterium necrophorum, an anaerobic gram-negative bacillus. (Courtesy of CDC, Dr VR Dowell, Jr.) |
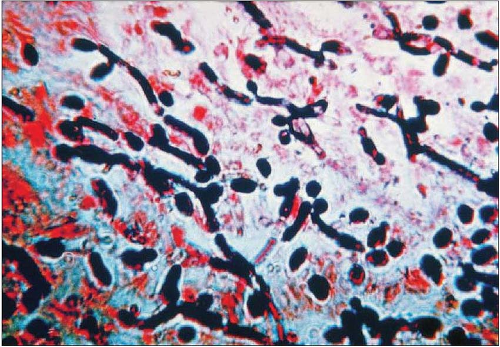 2.3 Photomicrograph showing yeast cells and pseudohyphae of Candida species. (Courtesy of CDC, Sherry Brinkman.) |
 2.4 Microscopic appearance of Aspergillus niger showing a globose conidial head containing fungal spores. (Courtesy of CDC, Dr Lucille K Georg.) |
Mycobacteria are identified on slide smears by Carbol fuchsin stain (e.g. Ziehl Nielsen, 2.5) or fluorochrome stains (e.g. auromine, rhodamine). Viruses (2.6) are the smallest of infective agents visible under electron microscope and are taxonomically classified according to viral structure (e.g. presence/absence of envelope, shape, symmetry) and antigenic composition.
Commensals
The upper respiratory tract harbours various micro-organisms, mostly bacteria, which form part of normal local flora. The bacteria are gram-positive and gram-negative aerobes and anaerobes and most of these are of low pathogenicity. Significant pathogens like β-haemolytic streptococci and Staphylococcus aureus can also be part of the normal flora in some individuals.
Saliva and gingival crevices from healthy adults yield heavy growths of coliforms and anaerobic bacteria such as Prevotella, Porphyromonas, Bacteroides, and Fuso bacterium which together with other commensal mouth flora can cause Ludwig’s angina and submandibular abscesses. Commensals of the mouth such as Actinomyces israelli and other Actinomyces spp. can cause chronic suppurative infection.
The naso- and oropharynx can harbour Streptococcus pneumoniae, Neisseria meningitides, and Haemophilus influenzae, usually without evidence of disease process, but occasionally can be a cause of pharyngitis. The nares are also usually colonized with Staphylococcus aureus, Streptococcus pneumoniae and, in a small percentage, with Neisseria meningitides. In hospitalized premature infants, the nasopharynx may be found to grow members of the Enterobactericiae ae (coliforms like Escherichia coli, Klebsiella oxytoca, and Enterobacter cloacae) and Pseudomonas spp., usually representing a more generalized disease process.
The external auditory canal is colonized with skin flora such as staphylococci and diphtheroids but may also carry S. pneumoniae, Pseudomonas aeruginosa, and anaerobic bacteria such as Propionibacterium acnes. Colonization with Aspergillus niger and Candida albicans can be a precursor of fungal otitis externa in children or diabetics. The middle and inner ear are usually sterile.
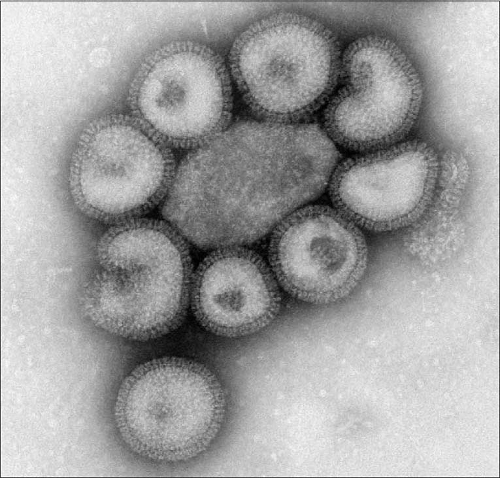 2.6 Negative stained transmission electron micrograph (TEM) depicting a number of influenza virus particles or ‘virions’. |
Principles of microbiological diagnosis
It is imperative to take appropriate specimens for culture and sensitivity to guide treatment and its duration. Based on the kind of specimen, appropriate specimen transport media should be used (2.7, 2.8, 2.9, 2.10 and 2.11). Microbiological diagnosis in most laboratories is based on microscopy and culture for bacteria and fungi. Blood culture bottles (2.12) inoculated with blood from patients with suspected sepsis are incubated in semi-automated blood culture cabinets. Some hazardous specimens and growing microorganisms are processed in biological safety cabinets (2.13) to prevent dangerous infections in laboratory personnel. Bacteria and fungi have characteristic appearance on a variety of culture medium (2.14, 2.15, 2.16, 2.17, 2.18, 2.19, 2.20, 2.21, 2.22 and 2.23). The final identification is based on biochemical tests (by recognition of metabolic end-products or enzymes). In the microbiology laboratory, differentiating normal from pathogenic flora depends on information provided about clinical presentation, findings, and also on local epidemiological knowledge.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree