Infections of the Nose and Paranasal Sinuses
Wolfgang Issing
Andreas Leunig
Introduction
Infections of the nasal cavity and the paranasal sinuses present with similar symptoms. A comprehensive history and examination, including nasendoscopy, is necessary to arrive at a differential diagnosis. Viral infections are ubiquitous. Despite a similar spectrum of bacterial infective organisms, there is geographical variation to antibiotic sensitivity and some infections (rhinoscleroma, fungal rhinosinusitis) are endemic.
Infections of the external nose
ERYSIPELAS
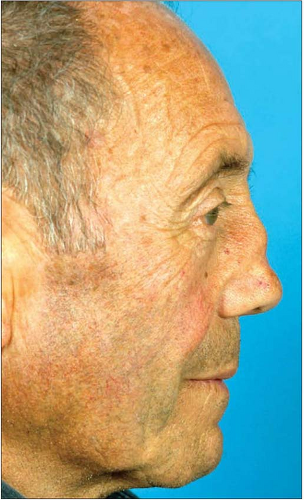
This is a cellulitic infection of the skin of the face. There is an erythematous area of skin with well demarcated edges (5.1). It is caused by a streptococcal (group A) infection, which usually starts in a small laceration of the skin. The laceration may not be visible but often starts in the nasal vestibule or outer ear canal, i.e. is secondary to a vestibulitis or otitis externa. The disease is associated with pain and high temperature. In rare cases blisters and necrotic areas can appear. The first-line treatment is intravenous penicillin.
HERPES SIMPLEX
This infection is caused by herpes simplex virus 1. Following a primary infection, recurrent infections can occur after activation of the dormant virus. Sun exposure and stress are common triggers. The typical lesions are found around the lips and the nose. The first symptoms are paraesthesia and a burning sensation. Later, small blisters develop which burst and leave the typical crusted, herpetic lesion (5.2). The herpes simplex infection disappears without scarring after a couple of days. There is no evidence to support the use of topical antiviral agents, but in severe cases, especially in immunocompromised patients, systemic antivirals (acyclovir and famciclovir) may reduce the duration of symptoms if taken early in an attack. Prevention is possible in the presence of clear-cut triggers.
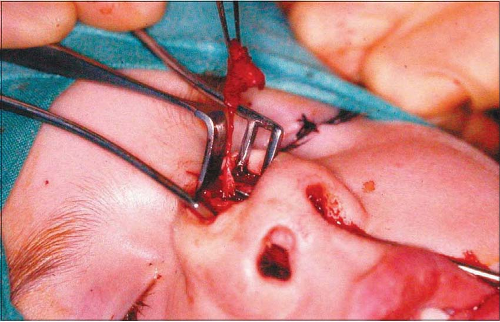
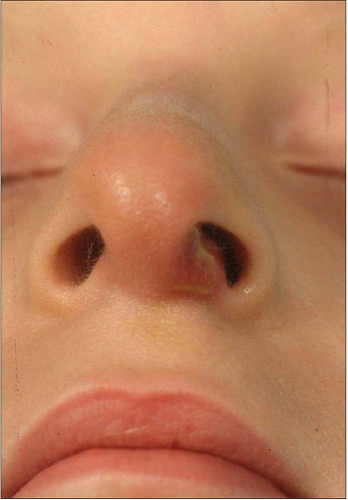
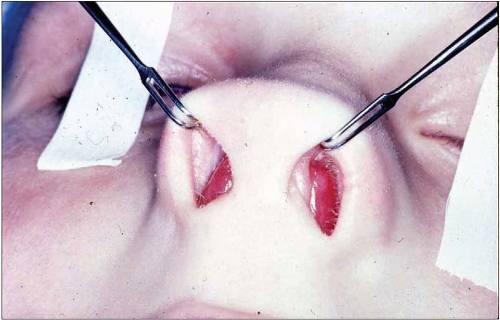
FISTULA OF THE NASAL DORSUM
Rarely, incomplete separation of the superficial ectoderm from the neuroectoderm during the embryological development results in the development of a dermoid or a fistula of the nasal dorsum (5.3). The fistula comprises a duct of squamous cell epithelium and can extend from the glabella to the tip of the nose. In rare cases there can be an extension intracranially. Intermittent secretions from the opening of the fistula can occur and secondary infections are common. A complete excision of the fistula and the duct is the therapy of choice in order to avoid recurrence (5.4).
FOREIGN BODIES
Foreign bodies (e.g. shrapnel) which are implanted in the soft tissue of the external nose and face due to trauma or explosions can migrate, even decades after the original injury and cause fistulas (5.5, 5.6). Treatment is the complete removal of the foreign body. Piercings and studs around the nasal vestibule can be the focus of a Staphylococcus aureus infection or a localized cellulitis (streptococcal). Removal of the foreign body and appropriate antibiotic therapy is required.
Infections of the nasal cavity
VESTIBULITIS
Infections of the nasal vestibule are usually caused by Staphylococcus aureus. In children, digital trauma leads to a chronic inflammation of the vestibule which becomes secondarily infected. Recurrent epistaxis is common and topical antiseptic creams will often eradicate the bacterial overgrowth and allow resolution of the vestibulitis and the recurrent epistaxis. In adults, infection in the hair follicles of the nasal vestibule causes a folliculitis (5.7).
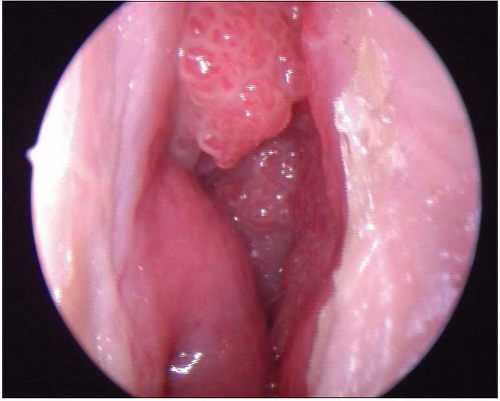
VIRAL PAPILLOMA
The human papilloma viruses cause warts or benign epithelial proliferations both on the skin of the nose and on the mucosal surfaces around the nasal vestibule. Inside the nose the proliferations are much more filliform and treatment is surgical removal as topical agents and cryotherapy are difficult to administer in this region (5.8).
SEPTAL HAEMATOMA AND SEPTAL ABSCESS
Trauma to the cartilaginous part of the nose can lead to a septal haematoma. A direct blow on the nasal tip is the commonest mechanism of injury, and there may or may not be an associated nasal fracture. The haematoma detaches septal perichondrium from the septal cartilage. If this occurs bilaterally the septal cartilage becomes detached from its blood supply, which comes via the perichondrium, and undergoes necrosis. Septal haematoma is a less common result of nasal trauma than a fractured nose. It can occur with relatively minor injuries, particularly in children, where an associated fracture is unusual. In adults an associated nasal fracture is more common and it can also occur as an early complication following septal surgery.
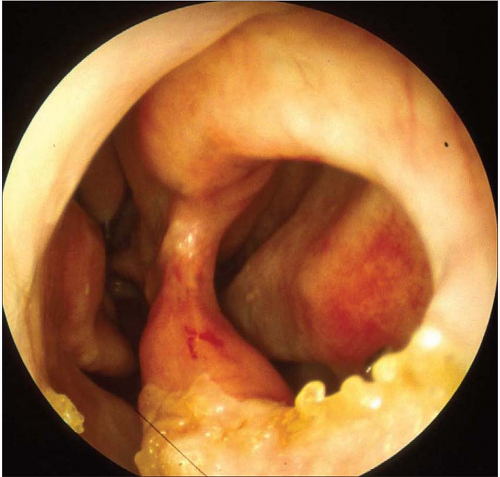
Haematomas will therefore present with a history of nasal obstruction following on from an episode of trauma. Anterior rhinoscopy reveals obliteration of the nasal cavity bilaterally by a soft swelling arising from the septum. They need early surgical drainage as left untreated the haematoma becomes secondarily infected and by 7 days the haematoma has become a septal abscess.
A septal abscess will present 5 or more days after the trauma and the patient will have developed toxaemia, pyrexia, and increasing pain (5.9). Acutely, this condition has a significant associated morbidity with cavernous sinus thrombosis, orbital cellulitis, and meningitis all described as possible complications. Prompt surgical drainage is required but by this stage there is always a loss of septal cartilage, leading to a septal perforation (5.10). If this is excessive, or if it occurs in a child, this will often lead to a saddle nose deformity in the long term (5.11).
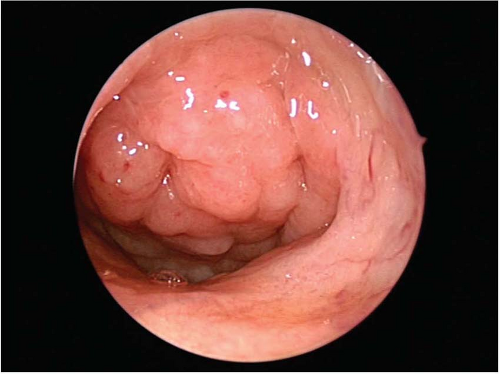
NASAL POLYPOSIS
The origin of this disease is still unknown. Infection is not normally thought to be part of the aetiology in the majority of cases, but patients with nasal polyps are more prone to problems with chronic infective rhino-sinusitis (see below). In addition, some patients with chronic sinusitis can develop an inflammatory hyperplasia of the nasal mucosa. This leads to the development of localized nasal polyps, which will originate in the area of the uncinate process and the middle meatus (5.12). Simple inflammatory nasal polyps present with nasal obstruction and hyposmia as the main symptoms, with little accompanying pain. Treatment is predominantly surgical although steroids used both topically or systemically may have a role. Polyps associated with underlying infected chronic sinusitis are more likely to have associated sinus pain.
NASAL FOREIGN BODIES
Children between 2 and 4 years of age have a tendency to insert foreign bodies into their noses. Round objects such as plastic beads are common and tend to become stuck just anterior to the inferior turbinate, where they are visible and cause nasal obstruction. Foreign bodies such as sponge, paper, and vegetable matter become secondarily infected after 24-48 hours and the child will present with a foul smelling unilateral nasal discharge. The foreign body may not be visible, so all children presenting with a unilateral foul smelling nasal discharge need an examination under anaesthesia to exclude the presence of a foreign body.