Treatment goals
Tests
Relieve symptoms
Symptom questionnaire: McMonnies, OSDI
Enhance lubrication
Lid-wiper fluorescein staining
Stabilize tear film
TFBUT
Protect ocular surface cells
Ocular Protection Index
Retard evaporative tear loss
Tear film lipid layer thickness (by slit lamp)
Suppress inflammation
Oxford scheme/NEI-Industry scheme
Support meibomian gland function
Slit lamp microscopy
Maintain adequate secretion
Schirmer I, tear film meniscus (by slit lamp)
A good understanding of the objectives of therapy is necessary to select the proper course of action for a patient with dry eye. The 2007 DEWS Report on Management and Therapy lists the current treatments available, whose efficacy can be backed by evidence (Table 5.2) (Pflugfelder et al. 2007).
Table 5.2
Dry eye menu of treatments
Artificial tears substitutes |
Gels/ointments |
Moisture chamber spectacles |
Anti-inflammatory agents (topical CsA and corticosteroids, omega-3 fatty acids) |
Tetracyclines |
Plugs |
Secretagogues |
Serum |
Contact lenses systemic immunosuppressives |
Surgery (AMT, lid surgery, tarsorrhaphy, MM and SG transplant) |
Figure 5.1 illustrates my simplified version of the dry eye cycle and the possible areas in the pathogenesis of dry eye wherein those evidence-backed treatments listed in Table 5.2 may be effective.
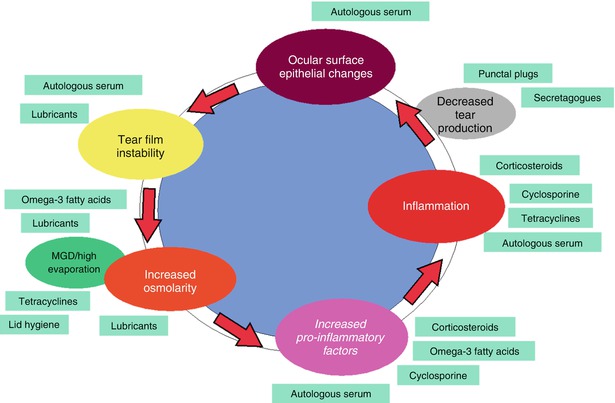
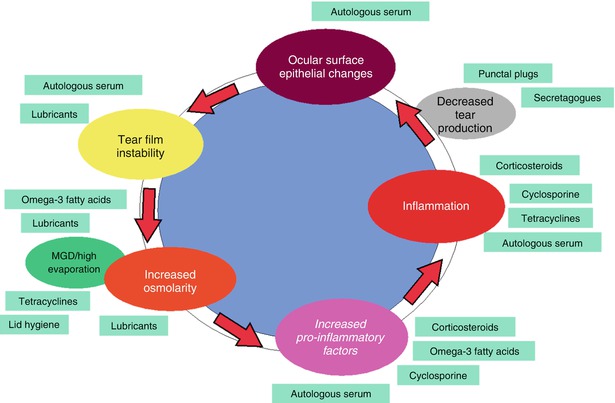
Fig. 5.1
Dry eye cycle
Our currently accepted approach is to base treatment on the severity of the disease, progressively adding treatment modalities with increasing signs and symptoms (as measured by tests described earlier in this book). The 2007 Dry Eye Workshop modified the approach originally taken by the International Task Force Delphi Panel for dry eye treatment, which based treatment recommendations on disease severity (Behrens et al. 2006) (Table 5.3). [N.B. For convenience the treatment recommendations originally formulated by the ITF and modified by DEWS has been appended to the bottom of the table.]
Table 5.3
Dry eye severity grading scheme and treatment recommendations
Dry eye severity level | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
Discomfort, severity, and frequency | Mild and/or episodic | Moderate episodic or chronic | Severe frequent or constant without stress | Severe and/or disabling and constant |
Occurs under environmental stress | Stress or no stress | |||
Visual symptoms | None or episodic mild fatigue | Annoying and/or activity-limiting episodic | Annoying chronic and/or constant limiting activity | Constant and/or possibly disabling |
Conjunctival injection | None to mild | None to mild | +/− | +/++ |
Conjunctival staining | None to mild | Variable | Moderate to marked | Marked |
Corneal staining (severity/location) | None to mild | Variable | Marked central | Severe punctate erosion |
Corneal/tear signs | None to mild | Mild debris, ↓ tear meniscus | Filamentary keratitis, mucus clumping, ↑ tear debris | Filamentary keratitis, mucus clumping, ↑ tear debris, ulceration |
Lid/meibomian glands | MGD variably present | MGD variably present | Frequent | Trichiasis, keratinization, symblepharon |
TFBUT (s) | Variable | ≤10 | ≤5 | Immediate |
Schirmer score (mm/5 min) | Variable | ≤10 | ≤5 | ≤2 |
Treatment | Education and environmental/dietary modifications | If level 1 treatments inadequate, add: | If level 2 treatments inadequate, add: | If level 3 treatments inadequate, add: |
Elimination of offending systemic medications | Anti-inflammatories | Serum | Systemic anti-inflammatory agents | |
Artificial tear substitutes, gels/ointments | Tetracyclines (for meibomianitis, rosacea) | Contact lenses | Surgery (lid surgery, tarsorrhaphy; mucus membrane, salivary gland, amniotic membrane transplantation) | |
Eye lid therapy | Punctal plugs | Permanent punctual occlusion | ||
Secretagogues | ||||
Moisture chamber spectacles |
5.2 Pharmacologic Therapy
5.2.1 Lubricants (“Artificial Tears”)
Ocular lubricants are the first and, for a long time, the only “line of defense” against dry eye. All modern ocular lubricants contain electrolytes, surfactants, and viscosity agents in a hypotonic or isotonic buffered solution (Table 5.4). They vary mostly in electrolyte composition, osmolarity, viscous agent, and the presence or absence of a preservative. But while a few limited studies have tended to show the benefit to the ocular surface of certain preparations containing certain types and concentrations of electrolytes, or a certain degree of osmolarity, or greater retention of the viscous agent, there is no evidence that any agent is superior to another (Pflugfelder et al. 2007) nor is there a consensus among both physicians and patients as to the superiority of any preparation. Figure 5.2, which shows the prescribing preferences of the different types of ocular lubricants across the globe, clearly demonstrates this fact (IMS 2012).
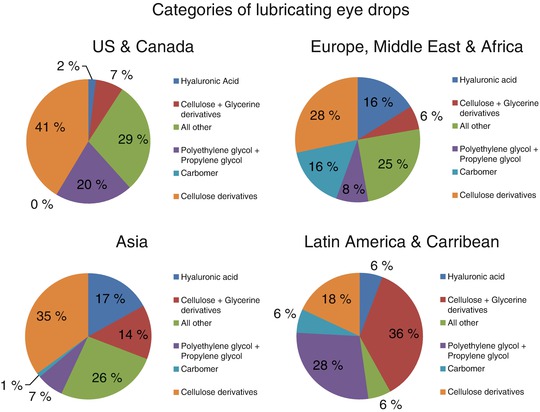
Table 5.4
Ocular lubricant properties
Component/characteristic | Claimed effect/benefit |
|---|---|
Electrolytes | |
Bicarbonate: recovery of damaged epithelial barrier function; maintain normal epithelial ultrastructure; maintain mucin layer (Ubels et al. 1995) | |
Compatible solutes (e.g., glycerin) | Increase intracellular osmolarity, protecting against possible damage from hyperosmolar tears (Lemp 2008) |
Viscosity agents | Increases residence in eye; provides patient comfort; protects damaged surface epithelium; increase tear film lipid layer |
Preservatives | Protects against microbial contamination; toxic to epithelium |
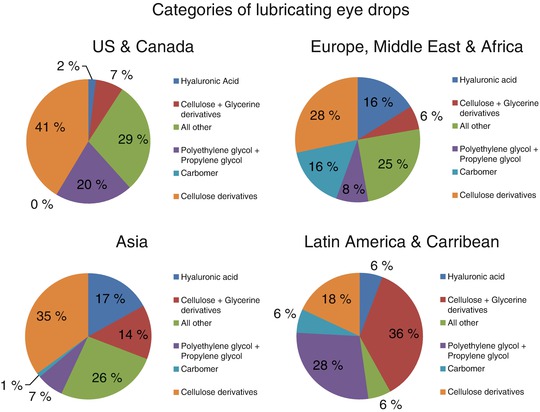
Fig. 5.2
Global ocular lubricants. The statements, findings, conclusions, views, and opinions contained and expressed in this publication are based in part on data obtained under license from the following IMS AG information service(s) (IMS MIDAS (Retail and Hospital) and OTCims (Retail Sales), FY 2012, Alcon Dry Eye Custom Market Definition, Extracted from Q4 2012 database. All Rights Reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its affiliated or subsidiary entities)
Did you know?
The ocular lubricants presently available in the United States are approved based on compliance with the US Food and Drug Administration (FDA) monograph on over-the-counter (OTC) products (21 CFR 349) which provides guidelines for the inclusion of active and inactive ingredients and for solution parameters, but are not based on clinical efficacy (Pflugfelder et al. 2007).
However, there is admittedly a general consensus and considerable evidence that the use of these preparations generally does result in the amelioration of symptoms as well as improvement in objective signs (McCann et al. 2012), especially in cases of mild dry eye, thus justifying their use as a staple in dry eye medication.
Lubricants benefit dry eye patients through one or more of the following mechanisms:
1.
Provides a lubricating layer between the lid-wiper edge of the palpebral conjunctiva of the upper lid and the ocular surface, i.e., relieves lid-wiper epitheliopathy (lid-wiper epitheliopathy is found in as much as 88 % of patients with symptoms – but no clinical signs – of dry eye) (Korb et al. 2010).
2.
Stabilizes the tear film, decreases optical aberrations, and improves the optical quality of vision (Montés-Micó 2007).
3.
May provide a “pseudo anti-inflammatory” effect, by:
(a)
Physical washing away of proinflammatory agents
(b)
Lowering tear osmolarity, through a diluting effect
(c)
Reducing the friction of lid-wiper epitheliopathy and reducing proinflammatory stress (Korb et al. 2005)
(d)
Aiding in corneal epithelial healing resulting in lower inflammation of the ocular surface (Daull et al. 2012)
Caveat
Despite the benefits of ocular lubricants in patients with dry eye, no preparation has been found through controlled studies to have resolved or “cured” the underlying ocular surface disease of dry eye.
5.2.2 Choosing a Lubricant
Often the choice of a lubricant will depend on the convenience to the patient. Will the drop stay in the eye long enough to give a sustained period of relief, or does it have to be re-instilled very frequently? This has special significance with drops containing a preservative, for which 4–6 times a day is the recommended limit (Berdy et al. 1992). Although clearly beneficial, preservative-free preparations in unit dose containers are more expensive and may be more cumbersome to use, especially for elderly patients. Preparations containing non-BAK preservatives may be better tolerated than BAK-preserved drops, although there is no evidence of lower toxicity with increased frequency of use. Lastly, increasing the viscosity of the eye drop improves retention time in the eye but results, in general, in increased blurring of vision and unsightly caking on the lids and matting of the lashes.
Ointments and gels have the advantage over solutions of increased retention time in the eye. This property allows for extended comfort for the patient. Additionally, ointments do not support bacterial growth and therefore need not contain preservatives. However, owing to their higher viscosity, ointments and gels significantly interfere with visual function and as a result are usually reserved for severe cases and nighttime use.
Practical Questions for Choosing a Lubricant
1.
Does the medication relieve symptoms?
2.
Does the preparation stay in the eye long enough to protect the ocular surface and provide comfort?
3.
How often will it be instilled in the eye daily?
4.
Does it contain a preservative, and if it does, which preservative?
5.
Does it impair visual function or cause unsightly caking on the lids and lashes?
Despite lacking clear evidence supporting superior efficacy of one lubricant preparation over another, many clinicians do have certain preferences based on their assessment of the patient’s dry eye condition. They make their choice of lubricant based on the previously mentioned practical considerations, patient preference, and their understanding, based on the limited evidence, of the strengths and purported features of a certain preparation. For example, recent reports have shown that drops containing oil in emulsion, by improving the lipid layer of the tear film, appear to perform better than conventional lubricants HPMC and sodium hyaluronate in evaporative dry eye (McCann et al. 2012). Given the current interest in the role of meibomian gland dysfunction in dry eye, many clinicians prefer to prescribe such oil-based preparations to their patients with MGD and dry eye.
Tables 5.5 and 5.6 below illustrate the ocular residence time and the lubricity (expressed as coefficient of friction) of various substances used in popular commercial preparations (Paugh et al. 2008; Meyer et al. 2007).
Table 5.5
Gross residence time data (time, in min, for signal to regain baseline)
Subject | Saline 1 | 0.3 % PG | CMC 0.5 % | CMC 1.0 % | Oil emulsion | HPMC 0.3 % gel | HPMC 0.3 % solution | Saline 2 |
|---|---|---|---|---|---|---|---|---|
1 | 24 | 44 | 30 | 38 | NTa | 26 | NT | 26 |
2 | 21 | 72 plusb | 34 plus | 72 plusb | NT | 44 | NT | 6.6 |
3 | 22 | 38 | 26 | 24 | NT | 18 | NT | 7.53 |
4 | 22.2 | 47 | 28.6 | 86 | NT | 54 | NT | 40 |
5 | 10.5 | 32 | 14 | 50 | NT | 24 | NT | 22 |
6 | 22.7 | 30 | 12 | 30 | 18 | NT | 31 | 19.5 |
7 | 14.1 | 16.5 | 14.5 | 36 | 7.4 | NT | 16.2 | 12.2 |
8 | 14 | 54.4 | 40 | 40 | 20 | NT | 28.4 | 26 |
9 | 6.1 | 18.7 | 20 | 16.2 | 14 | NT | 20 | 14.5 |
10 | 14.3 | 14 | 12 | 18 | 12 | NT | 13.9 | 16 |
11 | 29.8 | 36 | 18 | 46 | 32 | NT | 26 | 18 |
12 | 18.3 | 28 | 20 | 36 | 12 | NT | 14 | 12 |
13 | 36 | 55.5 | 20 | 54 | 19 | NT | 54 | 12 |
14 | 20 | 40 | 22 | 48 | 28 | NT | 24 | 20 |
15 | 14 | 22 | 24 | 24 | 26 | NT | 26 | 16 |
16 | 16 | 32 | 24 | 34.4 | 10 | NT | 16 | 14 |
Mean | 19.07 | 36.25 | 22.44 | 40.79 | 18.03 | 33.2 | 24.49 | 17.64 |
SD | 7.4 | 15.7 | 7.9 | 18.7 | 7.9 | 15.1 | 11.5 | 8.2 |
Table 5.6
Comparison of post-rinse (stage IV) coefficients of friction (tissue-on-tissue experiments)
Formulation | Final average coefficient for each of 3 replicate experiments | Average (SD) |
|---|---|---|
Saline control | 0.384, 0.263, 0.223 | 0.290 (0.068) |
HPMC solution | 0.109, 0.135, 0.156 | 0.133 (0.019) |
CMC solution | 0.252, 0.453, 0.291 | 0.332 (0.087) |
Glycerin emulsion | 0.265, 0.156, 0.174 | 0.198 (0.048) |
SYS 1 | 0.051, 0.057, 0.047 | 0.052 (0.004) |
SYS 2 | 0.041, 0.017, 0.041 | 0.033 (0.011) |
SYS 3 | 0.047, 0.122, 0.007 | 0.059 (0.048) |
The longer an instilled eye drop stays in the eye, the longer the protection and comfort. The lower the coefficient of friction, the greater the lubricity, resulting in less friction between palpebral conjunctiva and the ocular surface.
Again, while there is no firm evidence that one preparation is superior to the other, knowledge of the physical characteristics which influence the behavior in the eye of these substances aids practitioners in making a more systematic and scientific choice of ocular lubricant.
My Personal Preferences
1.
For mainly symptomatic patients with little or no objective signs of dry eye and whose needs do not require more than 3–4 times application daily, I prefer to use low-viscosity solutions (to avoid blurring) without a preservative or a mild, non-BAK preservative. Additionally, many of these patients suffer from lid-wiper epitheliopathy and benefit from agents with high lubricity (low coefficient of friction).
2.
For patients with moderate symptoms and with ocular surface staining, my preference is for solutions with low viscosity but with higher ocular retention, such as the liquid polyols (especially when linked with a gelling agent like HP-Guar) or sodium hyaluronate. The longer retention time and “bandage effect” of these agents protect and allow healing of the damaged epithelium. Non-preserved preparations are desirable.
3.
Dry eye with MGD requires oil-based emulsions to augment the lipid layer of the tear film and reduce evaporation.
4.
With more severe keratopathy, those preparations with high ocular retention and high colloidal osmolality (for deturgescent effect on damaged epithelial cells) are desirable. Gels and ointments may be necessary for severe cases.
5.3 Anti-inflammatory Therapy
The application of anti-inflammatory therapy (Table 5.7) in cases of dry eye is based on the central role played by inflammation in the initiation and propagation of dry eye. Good clinical evidence supports the efficacy of anti-inflammatory eye drops in improving severity of symptoms and decreasing corneal staining in moderate to severe dry eye, when compared to ocular lubricant therapy alone .
Table 5.7
Anti-inflammatory agents for dry eye treatment
Agent
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|