CHAPTER 37 Management of postoperative complications following glaucoma surgery
The clinical examination
Intraocular pressure
Finally, evaluation of the IOP is important to assess surgical complications. Often the eye is soft following filtering surgery, thus making IOP measurement difficult, especially if there is significant lid edema or chemosis. Additionally, accurate pressure reading may be particularly challenging with a shallow or flat AC. If there is lens or intraocular lens (IOL)–corneal touch, the applanation pressure may appear falsely elevated, as one may be essentially applanating the lens of the eye. In these circumstances, one may need to rely on assessment of the pressure by tactile tension to determine if the globe is soft or firm. See Figure 37.1.
Complications associated with a shallow or flat anterior chamber
Flat AC/low bleb/low IOP
Bleb leak
Formation of a healthy, well-functioning bleb is essential for a successful outcome following trabeculectomy. A complete, watertight closure of the conjunctival incision at the time of surgery is imperative. If the closure is incomplete or there is a defect in the overlying conjunctiva, the bleb will leak aqueous uncontrollably. Brisk leaks can cause failure bleb formation or lead to its collapse. Bleb leaks in the late postoperative period may result from conjunctival erosion from an underlying suture or perforation of a thin, avascular cystic bleb. In addition to a flat AC and hypotony, complications of untreated bleb leaks include formation of adhesions between intraocular structures, cataracts, corneal edema, hypotony maculopathy, blebitis, bleb failure, and endophthalmitis1,2.
Clinical features
Location of the surgical incision and bleb morphology may also contribute to the risk of developing bleb leaks. Limbal incisions are more likely to leak and have a positive Seidel test when exposed to positive pressure during the short-term postoperative period. During the long-term postoperative period, many surgeons feel that blebs with a limbal incision are flatter, more diffuse, and thus less prone to develop a late bleb leak. However, bleb leak incidence is not solely incision dependent. The additional surgical steps required to create a trabeculectomy can also contribute to bleb leakage. For example, the use of anti-metabolites intra- and/or postoperatively increases the risk of bleb leaks1,2.
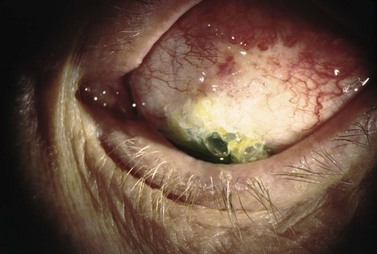
Leaks are best diagnosed at the slit lamp using fluoroscein and the Seidel test. Using the Indiana Bleb Appearance Grading Scale, a S0 bleb has no leak, S1 has multiple pinpoint leaks, and an S2 bleb has a brisk, streaming leak. The incidence of late bleb leaks ranges from 1 to 10%3,4. Bleb leaks are more common today secondary to anti-metabolite use, which produces thinner, more avascular blebs5,6. On presentation, patients may complain of mild blurring of vision, tearing, and light sensitivity. Frequently, a small bleb leak with only moderately decreased IOP can be managed conservatively in the short term with antibiotics, aqueous suppressants, and/or patching7. Larger leaks put the eye at risk for hypotony-related complications and failure of the bleb. The presence of a significantly shallow or flat AC, corneal edema, or deep stromal/Descemet’s folds indicates aggressive management is required.
Management
The treatment of a bleb leak is determined by bleb appearance, IOP levels, and presence of associated complications. A slow, pinpoint leak (S1), can be managed conservatively if the IOP is not too low. In addition to prophylactic broad-spectrum antibiotic drops, non-invasive measures include placement of a large diameter bandage contact lens (22–24 mm), aqueous suppressants, and possibly pressure patching to reduce aqueous flow through the defect, thus allowing conjunctival healing. If these measures fail, cyanoacrylic glue, autologous fibrin, and other tissue adhesives can be attempted to patch the defect8–10. Argon laser and Nd : YAG laser can cause a localized contraction of the overlying conjunctiva and potentially seal the defect11,12.
More invasive treatments include the placement of an ‘X’ suture (9-0 or 10-0 Prolene, ‘Palmberg’ suture) and an autologous blood patch13,14. Bleb needling redirects aqueous flow posteriorly and stimulates an inflammatory response. If the bleb leak is unresponsive to conservative or minimally invasive treatment, surgical intervention is warranted. In chronic or rapid leaks, the deficient conjunctiva is excised and the bleb is reformed by advancing adjacent conjunctiva15,16. In eyes with conjunctival scarring or insufficient healthy adjacent conjunctiva, an autologous conjunctival graft (usually from the inferior fornix or the other eye) may be used16. Alternatively, the bleb conjunctiva can be mechanically or chemically de-epithelialized (64 Beaver blade or denatured alcohol) followed by posterior conjunctival advancement during bleb revision17. See Figure 37.2.
Choroidal effusion
Clinical features
Choroidal detachment or effusion usually occurs in the setting of significant postoperative hypotony. Serous fluid from the choriocapillaries accumulates in the suprachoroidal space secondary to the difference in hydrostatic pressure between the hypotonous eye and the choroidal vessels18,19. Patients typically present with blurred vision, reduced peripheral vision, and occasionally with a headache or nausea. On exam, the IOP is usually low and the AC is shallow due to an anterior shift of the lens–iris diaphragm. Small choriodal effusions appear as shallow elevations with the loss of choroidal markings. Large detachments are dome-shaped elevations that have increased transillumination (Hagen’s sign).
Despite the increased bleb survival rate, the incidence of post-trabeculectomy effusions has risen secondary to anti-metabolite use. Various studies found the incidence of choroidal effusion with 5-FU was 3–33% and 10–25% with MMC20–27. Overall, the incidence of choroidal effusion requiring surgical draining has been reported to be as high as 14%20. Other factors that are associated with choroidal effusion include significant postoperative hypotony, inflammation, increased episcleral venous pressure and increased scleral rigidity28–34.
The risk of choroidal effusions can be reduced by minimizing the use (dosage and application/contact time) of anti-fibrotic agents, proper surgical closure of the sclerostomy and conjunctival incision and timely treatment of wound/bleb leaks and hypotony. If a patient is a low risk for extensive bleb scarring (primary trabeculectomy, thin conjunctiva, elderly patient), a single application of 5-FU for 5 minutes may be sufficient35. In higher risk groups (eyes with a history of uveitis, neovascularization, prior scarring or of African, West Indian, or Latino descent), MMC with multiple postoperative subconjunctival injections of 5-FU may be required36.
Management
The management of choroidal effusion in the early postoperative period includes addressing causes of hypotony, topical cycloplegia, topical corticosteroids, and avoiding physical activities that elevate intrathoracic pressure. Cycloplegia will rotate the lens–iris diaphragm posteriorly to minimize angle shallowing. If the AC is extremely shallow or flat, viscoelastic can be injected through the paracentesis to reform the chamber37,38. Most effusions will resolve spontaneously as the preoperative effects of glaucoma medications decrease, early wound healing occurs, and bleb formation begins. Indications for surgical intervention and drainage of an effusion include: (i) flat AC with persistent lens–corneal contact, (ii) flat AC with significant intraocular inflammation, (iii) appositional choroidal detachment (‘kissing choroidals’), (iv) combined serous retinal–choroidal detachment, (v) persistent bleb leak with hypotony, and (vi) persistent choroidal detachment39. Effusions can be drained via inferiorly located (3.5–4.5 mm posterior to the limbus), full-thickness scleral incisions placed either parallel or radial to the limbus. The retrieval of straw-colored fluid confirms that the effusion cavity was successfully accessed. The anterior chamber can be filled with fluid or viscoelastic during drainage of the effusion to facilitate more complete drainage, to reform the anterior chamber, and to elevate the bleb.
Visual prognosis following choroidal effusion is largely based on size, location relative to the macula, severity, chronicity, and other ocular complications of hypotony or a flat AC. Most small to moderate sized effusions resolve spontaneously without surgical intervention, and the visual outcome is good. The most common complication is cataract formation (4–54% in phakic eyes)40,41. Large choroidal effusions with severe hypotony and a flat AC are at a higher risk for developing corneal scaring from iris–cornea or lens–corneal touch42.
Flat AC/low bleb/high IOP
Malignant glaucoma/aqueous misdirection/ciliary block
Aqueous misdirection, also know as ‘malignant’ or ciliary block glaucoma, is an uncommon and challenging complication of intraocular surgery. Although malignant glaucoma has a complex and not fully understood pathophysiology, it is believed to occur when aqueous flow is diverted posteriorly into the vitreous cavity. Chandler proposed choroidal swelling causes a forward movement of the lens and an accumulation of fluid in the vitreous cavity. A ‘vicious’ cycle then ensues with increasing pressure posteriorly holding the lens in a forward position43. More recently, Quigley has proposed that malignant glaucoma is caused by poor vitreal fluid conductivity and a substantial posterior–anterior pressure gradient44. Choroidal expansion, documented by UMB, can elevate IOP, increase aqueous outflow from the AC, and develop a significant posterior–anterior pressure gradient. In this setting, the vitreous condenses and, along with the lens and iris, moves forward due to fluid expansion from the compressed vitreous45,46.
Clinical features
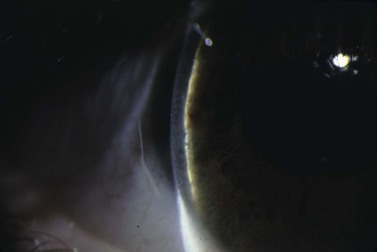
IOP will be elevated, the AC will shallow and flatten, and the bleb is poorly formed. Malignant glaucoma is difficult to distinguish from angle closure secondary to pupillary block. Typically in malignant glaucoma, the AC is uniformly shallow, whereas iris bombe is more typical with pupillary block. In addition, an iridotomy will relieve pupillary block, but will not break angle closure secondary to malignant glaucoma. Vision is typically decreased secondary to corneal edema, but may be normal. Although 20–54% of cases will have an IOP > 40 mmHg, up to 21% of patients will present with a normal or only slightly elevated IOP47–49. In addition, a B-scan ultrasound and a complete dilated fundus exam must be performed to rule out an annular choroidal detachment or suprachoroidal hemorrhage.
The incidence of malignant glaucoma after trabeculectomy is 0.2–4% in the general population and is higher in patients with narrow angles50–52. Malignant glaucoma typically occurs following intraocular surgery: 2.8–3.7% after a glaucoma drainage device (GDD) procedure, 0.03% after cataract surgery, 2–4.0% after iridectomy, and 10% after combined cataract extraction and penetrating keratoplasty43,50,53–56. However, single cases in non-operated eyes have been reported57,58. Smaller eyes (shorter axial length), eyes with narrow angles and eyes with a history of angle closure, pseudo-exfoliation, and chronic miotic use are at an increased risk for malignant glaucoma45,47,48,58. Malignant glaucoma in the fellow eye is a significant risk factor. This indicates an inherent predisposition for the development of malignant glaucoma43,44.
Management
The treatment of malignant glaucoma aims to lower IOP, to restore anterior chamber depth, and to re-establish the proper flow of aqueous. Cycloplegics widen the ciliary body diameter and pull the lens posteriorly by tightening the zonules59. Osmotic medications remove fluid from the eye and reduce the vitreous volume. Topical anti-inflammatory and anti-hypertensive medications are also used to control IOP and to reduce the formation of synechiae between intraocular structures. Anterior chamber reformation with fluid or viscoelastics may restore normal aqueous dynamics by re-establishing normal anatomic relationships.
Surgical management of malignant glaucoma is indicated when medical treatment fails. Argon laser causes a contraction of the ciliary processes to relieve ciliolenticular block60. Nd : Yag laser hyaloidotomy in aphakic and pseudophakic eyes produces communication between the anterior and posterior segments and allows the anterior flow of fluid60–66. Incisional interventions include transcorneal needling to disrupt the anterior hyaloids face, posterior sclerostomy with air injection (Chandler procedure), pars plana vitrectomy, lens extraction with posterior capsulotomy and anterior vitrectomy, cyclodestruction, and zonulo-hyaloido-vitrectomy48,50,51,62,67–72. The goal of all of these surgical approaches is to create a unicameral eye without the potential for competing anterior and posterior spaces.
The prognosis of malignant glaucoma depends on the duration of elevated IOP and angle closure. Prompt diagnosis and treatment optimize the visual outcome. However, despite good IOP control and early treatment, many patients with malignant glaucoma will experience a significant loss of vision. See Figure 37.3.
Flat AC/high bleb/high IOP
Suprachoroidal hemorrhage
Clinical features
Suprachoroidal hemorrhage (SCH) is a feared surgical complication of intraocular surgery (Fig. 37.4). A SCH occurs when the short posterior ciliary vessels rupture and bleed into the suprachoroidal space. SCH usually occurs after a sudden drop in IOP, which creates a change in the vascular gradient. When a SCH occurs intraoperatively along with loss of red reflex, iris and vitreous prolapse, and hardening of the globe, it’s known as an ‘expulsive hemorrhage’. Extrusion of ocular contents bodes for a poor prognosis. A delayed SCH occurs hours to days following surgery. In most delayed SCH there is preceding serous choroidal effusion with subsequent hemorrhage into the effusion. Patients will complain of sudden loss of vision and pain, which can develop after straining. On examination, the AC is shallow, the IOP is elevated, and the bleb is high secondary forced fluid expulsion in the anterior chamber through the sclerostomy and into the subconjunctival space73,74. A dilated fundus exam shows a dark red or brown choroidal elevation suggestive of blood, and a B-scan ultrasonography will show high internal reflectivity in the suprachoridal space.
The reported incidence of delayed SCH following glaucoma surgery ranges from 1.6% to 6.1% depending on the type of surgery performed49. Ocular risk factors for delayed SCH include aphakia, myopia, a high preoperative IOP, a sudden decrease in IOP in the immediate postoperative period (<24 hours), early postoperative hypotony (IOP ≤3 mmHg) and prior intraocular surgery. Prior history of SCH in the fellow eye is also a risk factor. The use of anti-metabolites may also be associated with a higher incidence of delayed SCH. Systemic risk factors for SCH include hypertension, preoperative anticoagulation, ischemic heart disease and respiratory disease. SCH has also been associated with a sudden increased in intrathoracic pressure, which can occur with vigorous coughing, vomiting, straining, and intraoperative ‘bucking’ while under general anesthesia75–81. These and all other types of Valsalva maneuvers should be avoided in the early postoperative period.
Management
The management of intraoperative SCH is directed at prompt closure of the eye and pressurization of the globe. Pain management and IOP control are vital to treat both intraoperative and delayed SCH. Indications for surgical intervention include intractable pain, flat AC, uncontrolled IOP, retinal detachment, central apposition (kissing choroidals), displacement of vitreous into the anterior chamber, and incarceration of vitreous or other intraocular contents into the wound. Surgical drainage of a SCH is performed through a full-thickness sclerostomy, 3–4 mm posterior to the limbus, and anterior segment infusion of balanced salt solution82. The timing of surgical intervention of SCH is debatable. Although many surgeons prefer nearly complete clot lysis prior to surgical drainage (confirmed by B-scan ultrasound), delaying intervention until complete liquefaction has not fully been elucidated. Some studies have shown improved visual outcome with early surgical intervention75,83,84. Surgical drainage often requires 3–5 days until greater than 50% of the blood has liquefied within the suprachoroidal space by B-scan, which often requires 3–5 days.
SCH has a guarded prognosis and can lead to vision-threatening complications, such as retinal detachment, hypotony-associated maculopathy, RPE disruption, keratopathy, and phthisis bulbi77. Small SCHs may resolve without compromising the vision; however, expulsive or large SCHs typically have poor outcomes83,84. Poor prognostic factors include an afferent pupillary defect, poor visual acuity at presentation, coexisting uveitis or macular degeneration, retinal detachment, and prior extracapsular cataract extraction75,83. Prognosis is also worse with breakthrough bleeding into the vitreous cavity.
Flat AC/high bleb/low IOP
Over-filtration
Over-filtration, with resultant ocular hypotony, can be seen with overly diffuse blebs, loose suturing of the scleral flap at the time of surgery, and thin, avascular blebs. The rise in use of intraoperative anti-metabolites has increased the incidence of ocular hypotony following trabeculectomy85. Clinically, IOP will be low and the AC depth normal or shallow. Bleb morphology is an important to diagnose the underlying cause of over-filtration. A diffuse bleb, a very high bleb, or a thin, cystic bleb along with a low IOP, normal or shallow AC, and a negative Seidel test can indicate over-filtration.
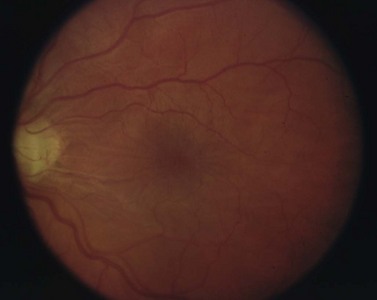
Long-standing hypotony may lead to a number of serious, sight-threatening complications. Loss of vision is typically secondary to choroidal effusion, choroidal hemorrhage, cataract development, and hypotony maculopathy. Hypotony maculopathy is one of the more serious and common complications associated with over-filtration. Chronic hypotony causes chorioretinal folds, choroidal thickening, loss of photoreceptors, and dilated retinal vessels. If left untreated, these can lead to permanent retinal changes and loss of vision. See Figure 37.5.
Given the potential long-term complications with persistent hypotony, several techniques have been developed to reduce the outflow of aqueous humor through an overfunctioning filtering bleb. Treatment options include the placement of an oversized bandage contact lenses or compressive Simmons shell, intra-bleb autologous blood injection (Fig. 37.6), trichloroacetic acid, cryotherapy, laser therapy (argon, Nd : YAG), compression mattress sutures, AC injection of viscoelastic, and surgical bleb revision. The placement of a large diameter contact lens is a safe and effective way of compressing the bleb and restricting flow. After 1–2 weeks, cellular remodeling occurs and aqueous outflow slows. Cryotherapy can shrink larger blebs, and tricholoracetic acid can induce inflammation with subsequent bleb fibrosis. However, a high incidence of corneal toxicity and conjunctival breakdown has been also reported following tricholoracetic acid. Shirato et al. and Letartre et al. describe transconjunctival suturing of the scleral flap as a safe and effective over-filtration treatment86,87. Transient leakage at the site of suturing points was occasionally seen; however, these spontaneously closed without intervention.
Complications associated with deep anterior chamber
Deep AC/low bleb/high IOP
Obstruction of outflow
Resistance at the internal sclerostomy
Blood, fibrin, viscoelastic, ocular structure (iris, vitreous, ciliary body), or implant material can block the internal sclerostomy or tip of a drainage device. Increased resistance to outflow deepens the AC and increases IOP. The bleb height will be low. Gonioscopy directly visualizes the internal ostomy and is essential for diagnosis and proper treatment. Blood occluding the sclerostomy will appear as a reddish discoloration around or in the sclerostomy track. Digital pressure to the globe may dislodge the blood88. If the IOP is not too high, conservative management with close monitoring is appropriate as most clots resolve within 24–72 hours. If the IOP is significantly elevated or the integrity of the bleb is in question, additional treatment modalities can be used. Intracameral tissue plasminogen activator (tPA) can lyse the clot successfully89,90. However, significant complications have been reported: hyphema, band keratopathy, corneal clouding, and vitreous hemorrhage90–94. Early transconjunctival suture lysis or loosening of releasable sutures can help to dislodge the clot. Once the obstruction has been cleared, hypotony is common. Therefore, in the absence of vision threatening pressure spikes, conservative management is advised.
Peripheral iris tissue can become incarcerated into the internal sclerostomy (Fig. 37.7). Pupillary constriction with topical mitotics may occasionally relieve the occlusion. Argon laser to adjacent iris stroma can contract the iris away from the internal ostium; Nd : YAG laser can remove iris blocking the opening. Injection of viscoelastic at the site of blockage can separate the two opposing structures. If surgical treatment is required, an iris spatula can sweep the incarcerated tissue away from the sclerostomy. If vitreous is occluding the internal sclerostomy, an anterior vitrectomy can be performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree