(1)
Alo Eye Care, Kolkata, India
Keywords
Basal cell carcinomaClassic rodent ulcerSquamous cell carcinomaVascular tumorsMetastatic tumors6.1 Malignant Tumors of Epidermis
6.1.1 Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the commonest malignant tumor of the eyelids. It is a tumor of a low degree of malignancy and is locally aggressive. This tumor also is known as “rodent ulcer.” The lower lid and medial canthus are affected more commonly. If the tumor is untreated, it may infiltrate the tissue, penetrate deep into the bone, and cause ulceration.
6.1.1.1 Age of Presentation
BCC usually occurs in adults between the ages of 50 and 80 years. It may develop in a younger population in patients with nevoid basal cell carcinoma syndrome, nevus sebaceous of Jadassohn, or xeroderma pigmentosum.
6.1.1.2 Risk Factors
Suspected risk factors for developing BCC include the following:
Exposure to ultraviolet radiation
Skin type 1 (always burns, never tans), red or blonde hair, and blue or green eyes have been shown to be risk factors (Wong et al. 2003).
History of frequent or severe sunburn in childhood
A positive family history of skin cancer
Patients on immunosuppressive treatment
History of arsenic poisoning
6.1.1.3 Types
Nodular
Nodular BCC, the most common type, appears as a translucent, waxy papule with a rolled, pearly border. It often is associated with telangiectasia over the margin of the lesion, and a central ulceration usually develops over time.
Ulcerative
The classic rodent ulcer has an indurated edge and ulcerated center. The margin of the ulcer shows dark pigmented edges. It is slow growing but may spread deeply, causing considerable destruction.
Noduloulcerative
The noduloulcerative BCC lesion has a typical waxy papule with a central depression, and ulceration, bleeding, crusting, a rolled border, translucency, and telangiectases over it are quite common. In this form, as the margin of the tumor grows, the center’s blood supply diminishes, and the tumor begins to take on a crusted, umbilicated appearance, which may loosen and bleed. This bleeding is often what brings the patient to the physician.
Pigmented
Pigmented BCC may be nodular or flat with slightly increased brown or black pigment. This type is seen more often in individuals with dark skin.
Morpheaform/Sclerosing
Morpheaform/sclerosing tumors resemble scar tissue or morphea, occurring as a thick, firm plaque with atrophy, hypopigmentation, erythema, and prominent telangiectasia. Morpheaform BCCs have an irregular growth pattern, making the tumors’ margins difficult to delineate. This pattern is more aggressive and has poorly defined borders. This type presents late and may become very large, requiring extensive plastic surgical reconstruction.
6.1.1.4 Differential Diagnosis
Each type of BCC may mimic a different suspected lesion; therefore, the differential diagnoses have been grouped on the basis of subtypes:
Ulcerative BCC
Discoid eczema
Psoriasis
Actinic keratosis (solar keratosis)
Bowen’s disease
Squamous cell carcinoma
Seborrheic keratosis
Nodular BCC
Intradermal nevus
Sebaceous hyperplasia
Fibrous papule
Molluscum contagiosum
Keratoacanthoma
Pigmented BCC
Melanoma
Morpheaform BCC
Scar tissue
Localized scleroderma
6.1.1.5 Treatment
Treatment involves wide surgical excision with a frozen section of margin or Moh’s micrographic technique to assure a tumor-free margin. This is followed by lid reconstruction of the tissue defect, based on the principles of reconstruction.
BCC usually is a locally invasive form of malignancy. It may recur after excision. Metastasis occurs very rarely.
In cases in which the BCC has extended deep into the orbit, exenteration may be necessary.
In cases in which surgery cannot be performed, cryotherapy, radiotherapy, or photodynamic therapy to the tumor mass and base sometimes is tried. Chemotherapy may be another option.
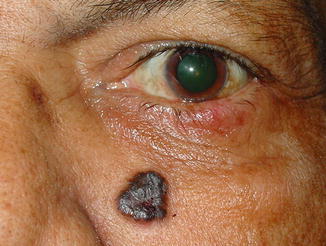

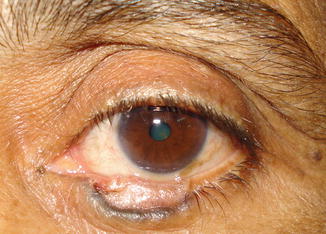





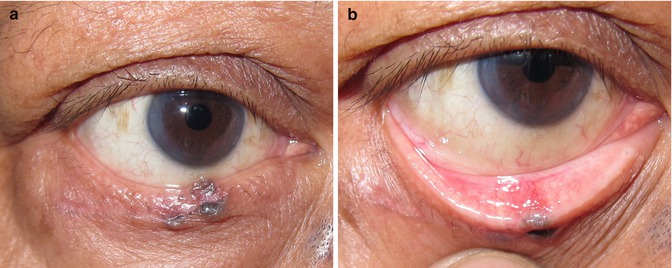


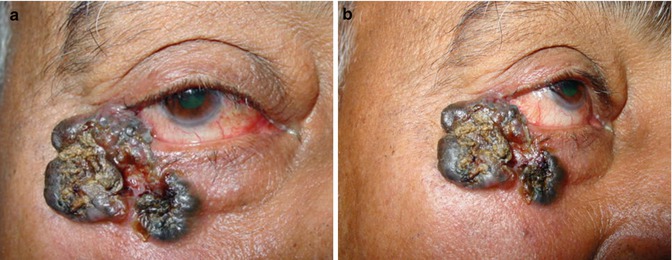










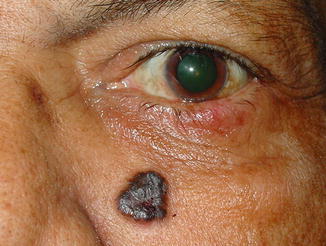
Fig. 6.1
Hyperpigmented, elevated shiny lesion over the nasolabial fold highly suspicious of BCC

Fig. 6.2
Note the fine telangiectatic vessels on its surface and central dense pigmentation very classical of BCC
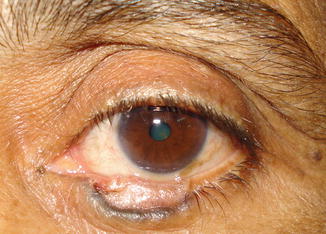
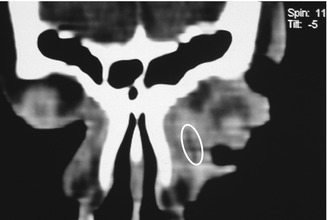
Fig. 6.3
An ulcerative BCC involving the lower lid margin

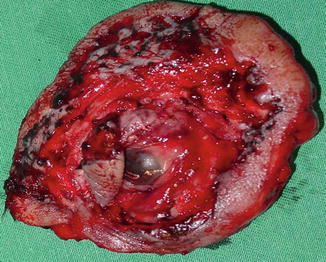
Fig. 6.4
The whole upper and lower lids are involved. The BCC has extended into the orbit, causing a fungating mass

Fig. 6.5
An ulcerative lesion involving the lateral canthus

Fig. 6.6
Noduloulcerative variety of BCC

Fig. 6.7
A small pigmented rodent ulcer over the medial canthus

Fig. 6.8
Rodent ulcer in which the base has necrosed
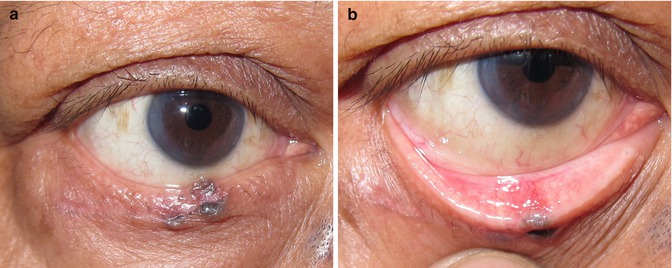
Fig. 6.9
(a) A small pigmented rodent ulcer over the lid margin. (b) Note its extension into the tarsal aspect

Fig. 6.10
Very large ulcerated lesion involving almost the whole upper lid

Fig. 6.11
A relatively large nodular pigmented variety of BCC
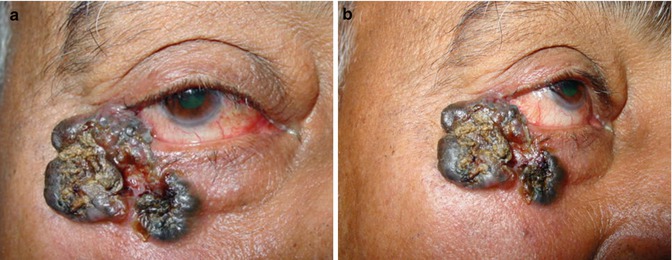
Fig. 6.12
(a, b) A large multilobulated elevated lesion with a central ulcerated area over the medial canthus and lower lid

Fig. 6.13
This lesion is similar to the one in Fig. 6.12 but involves the inferonasal part of the lid margin and beyond. A hyperpigmented, elevated, shiny lesion appears over the nasolabial fold. Highly pathognomic of BCC

Fig. 6.14
A pigmented BCC over the medial canthus

Fig. 6.15
A large elevated and pigmented variety of BCC

Fig. 6.16
BCC with central ulceration and surrounding pigmentation

Fig. 6.17
BCC of multicentric origin involving the medial canthus lower lid as well as the lateral canthus. It has become difficult to remove because of its multicentricity

Fig. 6.18
Morpheaform/sclerosing type of BCC

Fig. 6.19
In the common nodular form, as the margin of the tumor grows, the center’s blood supply diminishes and begins to take on a crusted, umbilicated appearance, which may loosen and bleed. This bleeding often is what brings the patient to the physician

Fig. 6.20
The whole orbit has been involved by BCC. A fly has deposited eggs on the central ulcer, and larval stage maggots have formed within the orbit. Note the innumerable black spots, which are the ends of the maggots

Fig. 6.21
Another BCC infested by maggots

Fig. 6.22
Very large forehead BCC infested with maggots
6.1.2 Squamous Cell Carcinoma
Squamous cell carcinoma (SCC) may resemble BCC, but it is relatively avascular and tends to grow much faster. Whereas BCC is locally invasive, SCC is more likely to metastasize. Perineural spread to the orbit and periocular region, as well as intracranial spread, is much greater. Local lymph node extension is common in recurrent cases. SCC usually accounts for 2–9 % of eyelid malignancies.
6.1.2.1 Clinical Presentation
SCC may arise de novo or from a premalignant lesion, such as actinic keratosis. It may occur in situ (Bowen’s disease) or be invasive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree