CHAPTER 66 Macular hole surgery
Introduction
Macular hole (MH) was an incurable condition until the late 1980s, when its first successful surgical treatment was reported1. Since then it has aroused ophthalmologists’ interest, which has led to improved understanding of its pathogenesis, surgical treatment, and postoperative results.
History
MH was first described by Knapp in 1869. In 1924, Lister considered the role of the vitreous in the occurrence of MHs by describing vitreous bands causing traction on the macula, but this hypothesis was ignored for a long time. Gass in 1988 postulated that focal shrinkage of the prefoveolar vitreous cortex and tangential retinal traction are responsible for MH formation2. Finally in 1999 Gaudric et al. and Haouchine et al., using optical coherence tomography (OCT), provided a precise description of the formation of MHs3,4.
Epidemiologic consideration and terminology
The onset of idiopathic MH usually occurs in the 6th decade of life, predominantly among women. Both eyes are affected in 10% of cases. Population studies has found an incidence of idiopathic MH of 7.8 per 100 000 persons per year, with a female to male ratio of 3.3 to 1 and a prevalence of 0.33% in elderly subjects over 55 years old5,6.
Clinical features, diagnosis, and differential diagnosis
Diagnosis of an idiopathic full-thickness MH
Most MHs occur in eyes with no previous pathology (‘idiopathic’). The patient generally complains of acute or subacute decrease in both far and near visual acuity (VA), ± metamorphopsia and/or micropsia, ± positive or negative scotoma. Five percent of patients are asymptomatic7. The visual loss caused by MH is variable. VA decreases gradually with time, and after several months of evolution it is usually around 0.1. In a series of unoperated MHs, more than 80% of eyes had a VA between 0.1 and 0.05 after 5 years of follow-up8. In practice, the VA of an eye with a full-thickness MH is usually less than 0.5 (typically 0.2). Patients rarely identify a central scotoma, but fairly frequently report what is indicative of a negative microscotoma (i.e. the disappearance of a letter from a word). The distortion or constriction of images and words is also reported.
At fundus biomicroscopy, the MH appears as a round full-thickness defect with sharp edges located at the center of the fovea. The size of the hole varies and tends to increase with time8–10. The surrounding retina is usually thickened by edema and microcysts, and is slightly detached from the retinal pigment epithelium (RPE). In half the cases, 1–15 yellow deposits are present on the exposed RPE. An operculum may also be found in front of the hole. It is generally smaller than the hole, usually round but sometimes irregular in shape, translucent, discreetly yellow, and slightly mobile with eye movements. An epiretinal membrane may also be present around the hole. It appears as a discreet reflection, usually with no wrinkling of the internal limiting membrane (ILM). The prevalence of epiretinal membranes is higher in long-standing MHs11–13. Posterior vitreous detachment may vary, from incomplete separation of the vitreous from the macula to a vitreous completely detached from the macula and even from the disc3,4.
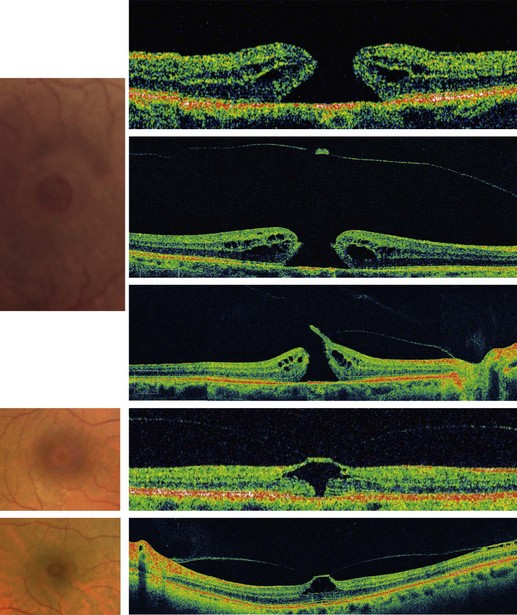
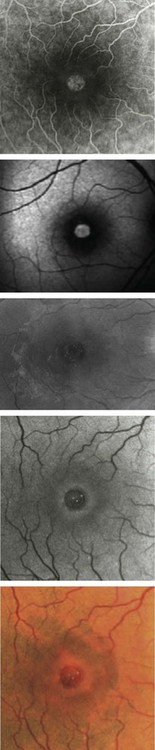
OCT allows a reliable diagnosis of MHs by confirming the existence of a full-thickness opening in the center of the fovea with no interposition of tissue between the vitreous cavity and the RPE. OCT also clearly differentiates full-thickness MHs from lamellar or pseudo-holes, shows the stage of MH, measures its diameter, and provides information regarding the risk of developing a MH in the fellow eye. No other ancillary testing is mandatory. Fundus photographs can be used as archive. Fundus autofluorescence images and fluorescein angiography are not of great interest for MHs. The defect is usually hyperautofluorescent and after fluorescein injection shows a discrete early hyperfluorescence. The surface area of fluorescence does not increase during angiography and its intensity decreases at later phases with no dye diffusion (Fig. 66.1)14,15.
Differential diagnosis
Without OCT, MHs might be misdiagnosed. With OCT, the differential diagnosis is very reliable. Unlike a full-thickness MH, in a macular lamellar or pseudohole there is an interposition of retinal tissue between the vitreous cavity and RPE on OCT scans. Lamellar holes, usually due to an aborted process of MH formation, are characterized by thinning of the base of the foveal center, and normal thickness of the foveal edge that presents a cleft between its inner and outer retina16. Pseudoholes are due to tangential retraction of an epiretinal membrane that thickens the foveal edge with a normal or thin foveal center16.
Impending MHs
In most cases, early stage MHs are foveal cysts3,4. VA in these cases is usually normal or above 0.5. The macula may look normal on fundus biomicroscopy, or else an outer central yellow spot may be present, combined with a flattened foveal pit and foveolar radial striae17. In more advanced cases, outer MHs, the foveola has a cystic appearance, with radial striae. An outer yellow ring is present17.
Secondary MHs
Post-traumatic MHs mostly occur in young males. Traumatic MH is due to a violent deformation of the eyeball, which results in rupture of the fovea18,19. The vitreous remains completely attached to the retinal surface. The profile of the traumatic hole is not different from that of the idiopathic hole, except in cases in which the retina is thinner than normal at the hole edge due to post-traumatic atrophy of the pigment epithelium. Indeed, in some cases, these MH may be associated with a break in Bruch’s membrane or an area of pigment epithelium atrophy at the posterior pole, which on OCT scans corresponds to retinal thinning and to a deep scotoma in the visual field. If the lesion involves the foveal center, there is a risk that vision will not improve, even if the MH is closed.
In about 10% of highly myopic eyes, OCT reveals the presence of a MH in the staphyloma, which causes moderate loss of vision and is not seen on biomicroscopy. In eyes with high myopia, an MH may also occur after a long evolution of a myopic foveoschisis, especially when it is complicated by foveal detachment20.
Anatomical considerations
Before OCT became available, Gass classified MHs into several stages on the basis of fundus biomicrospy. Later he revised his classification. This revised classification is still in use and is summarized in Box 66.1. Mainly on the basis of OCT examination of MHs and their relationship with posterior vitreous detachment, Gaudric et al. and Haouchine et al. gave the description of the different steps in MH formation and evolution (Fig. 66.2)3,4. Gaudric’s description of MHs is also used as a system of classification mainly based on OCT. In this classification the size of the MH is indicated separately. The information provided by Gaudric’s classification is more accurate.
Box 66.1
Gass’s revised classification of macular holes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree