23
Macular Edema Associated with Aphakia and Pseudophakia
Hiroko Terasaki
INTRODUCTION
Cystoid macular edema (CME) is characterized by cystoid spaces in the macular area with perifoveal fluorescein leakage, increased thickness of the retina, and visual impairment. This form of CME is referred to as clinically significant CME. CME can also be present without the increased macular thickness and is referred to as angiographic CME (1–5). CME is not a frequent complication of recent, modern, and successful cataract extraction and posterior intraocular lens (IOL) implantation (1). There are some factors that predispose eyes to CME after uneventful cataract surgery, including uveitis, retinal vein occlusion, and diabetes mellitus, and also after complicated cataract surgery (2, 3). CME tends to resolve spontaneously or with pharmacological treatment (6–11); however, if it remains chronic, a permanent loss of central vision can occur. Clinical improvement can occur in eyes with no apparent vitreous traction.
Vitrectomy has been reported to be effective in treating CME, and some pseudophakic eyes with chronic CME that is unresponsive to medical treatment will recover good vision after vitrectomy (12–18). In this chapter, we discuss the rationales for vitrectomy to treat aphakic/pseudophakic CME and report the indications and effectiveness of recent surgical techniques in treating CME.
PATHOGENESIS OF APHAKIC/PSEUDOPHAKIC CYSTOID MACULAR EDEMA
Inflammatory responses are activated to different degrees in eyes that have undergone intraocular surgery. Prostaglandins (PGs) are released postoperatively by a disruption of the blood–retinal barrier caused by inflammation, hypotony, vitreous traction, and other complications. The PGs are metabolic breakdown products of arachidonic acid, and they have been postulated to be causative of CME (19). The products of the arachidonic acid cascade are not only chemical transmitters but also consist of complement, platelet-activation factor, lysosomal enzymes, and interleukin 6. In addition to these chemical mediators, vascular endothelial growth factor (VEGF) also acts with PGs as key mediators in the breakdown of the blood-aqueous-barrier (BAB) or blood-retinal-barrier (BRB). In fact, the efficacy of intravitreal injection of anti-VEGF has been reported to treat eyes with CME (11), which would indicate that there was an upregulation of VEGF in eyes with CME. This upregulation is not limited to the macular area but is present diffusely in the eye, which suggests that soluble chemical mediators are released by the primary lesion (20). In addition to the inflammation, vitreous traction on the retina in the macular area has been postulated to be the cause of CME in a small number of patients.
ROLE OF VITRECTOMY
Releasing the vitreous traction on the iris or the ciliary body is expected to inactivate the inflammatory response and enhance the passive transport of chemical mediators through the nonpigmented epithelium of the ciliary body. Removing the entire vitreous as a reservoir for cytokines may contribute to a faster clearance of chemical mediators.
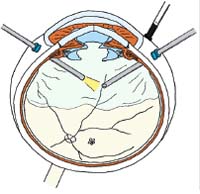
Eyes in which the posterior hyaloid remains attached to the retina may benefit from separation of the vitreous from the retina and release of traction. Peeling the internal limiting membrane (ILM) has not been proven to alleviate the CME in a cohort study, although there are some case reports that found an improvement of CME after ILM peeling (21).
EVALUATION OF CYSTOID MACULAR EDEMA
The basic ophthalmological examinations required to examine eyes with suspected CME are visual acuity, ophthalmoscopy, biomicroscopy, and fluorescein angiography. The recent development of high-resolution optical coherence tomography (OCT) instruments has allowed clinicians to detect different degrees of increased macular thickness, cystoid spaces in the middle layers of the retina, and the presence or absence of the IS/OS line, a high-reflective line in OCT images present at the border of photoreceptor inner and outer segments. Vitreous traction on the macular area can also be documented by high-resolution OCT techniques (Figs. 23-1 to 23-4).
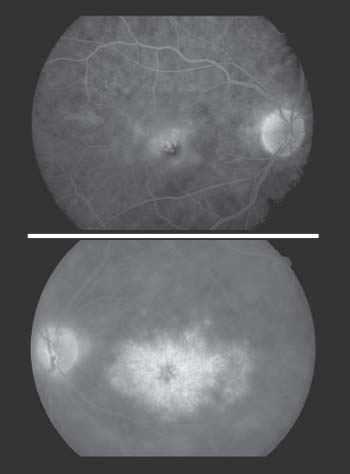
Figure 23-1.Fluorescein angiogram of pseudophakic eye with cystoid macular edema. Grade II? with circumferential leakage of fluorescein (top). Grade III? with typical honeycomb appearance of fluorescein pooling in the cystic spaces (bottom) (From Miyake K, Ota I, Maekubo K, et al. Latanoprost accelerates disruption of the blood-aqueous barrier and the incidence of angiographic cystoid macular edema in early postoperative pseudophakias. Arch Ophthalmol 1999;117:34).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


