Purpose
To compare the long-term outcomes of accelerated and standard corneal cross-linking protocols in the treatment of progressive keratoconus.
Design
Prospective randomized clinical trial.
Methods
Thirty-one eyes with keratoconus were treated with an accelerated protocol (18 mW/cm 2 , 5 min) and all contralateral eyes were treated with the standard method (3 mW/cm 2 , 30 min) using the same overall fluence of 5.4 J/cm 2 .
Results
At 18 months after the procedure, the standard group showed significant improvement in spherical equivalent ( P < .05), K-readings ( P < .05), Q value ( P < .05), index of surface variance ( P < .05), and keratoconus index ( P = .008) and decline in central corneal thickness ( P < .05), but no significant change in visual acuity, corneal hysteresis, corneal resistance factor, P2 area, or endothelial cell density. In the accelerated group, central corneal thickness was the only parameter with statistically significant change. However, neither of these parameters showed significant differences between the standard and the 18 mW/cm 2 accelerated protocol, except K-reading ( P = .059) and index surface variance ( P = .034).
Conclusion
An accelerated cross-linking protocol, using 18 mW/cm 2 for 5 minutes, shows a comparable outcome and safety profile when compared to the standard protocol, but better corneal flattening is achieved with the standard method than the accelerated method. Overall, both methods stop the disease progression similarly. This study will continue to examine more long-term results.
The standard method of corneal cross-linking (CXL) with riboflavin and ultraviolet (UV) A (3 mW/cm 2 , 30 minutes), now widely known as the “Dresden protocol,” was originally developed by Wollensak and associates for the treatment of progressive keratoconus. The long-term safety and efficacy of this method has been demonstrated through many investigations. In 2010, several accelerated CXL protocols were introduced with the purpose of reducing illumination time by increasing intensity while maintaining the fluence at 5.4 J/cm 2 . Both clinical and experimental studies in this area have reported ambiguous results. In the first report of this randomized clinical trial, we demonstrated a similar trend for these 2 methods in terms of 6-month changes in vision, refraction, keratometry, corneal shape, endothelial cell density (ECD), and corneal biomechanics, which are in agreement with previously published data. The only intermethod difference was the decrease in the central corneal thickness (CCT), which was greater in the standard group than in the accelerated group. Clinically, it is important to compare long-term results of the 2 methods; thus, here we present 18-month results with these methods and their comparison.
Methods
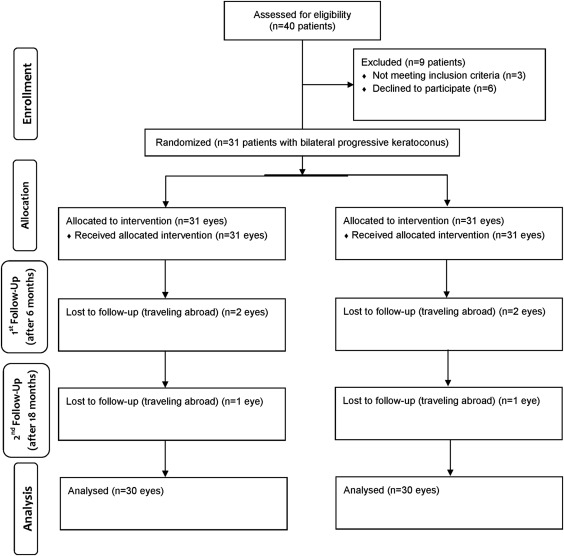
This study was performed at Noor Eye Hospital, Tehran, Iran between March 6, 2013 and February 14, 2015. The methodology of this study has been described previously. In brief, this prospective single-masked randomized clinical trial enrolled patients with bilateral progressive keratoconus. To ensure concealment, randomization was done by a person other than the ophthalmic surgeon. In each patient, the contralateral eye served as the control (standard CXL) for the other eye. Inclusion criteria were a diagnosis of progressive keratoconus (at least 1 diopter [D] increase in maximum keratometry [K max ], manifest cylinder, or manifest refraction spherical equivalent [MRSE] or the loss of at least 2 lines of corrected distance visual acuity [CDVA] within the past 12 months), age between 15 and 35 years, keratometry reading less than 55.0 D, and a minimum CCT of 400 μm. Patients with any history of eye surgery or eye disease were excluded from the study. Hard and soft contact lens users were instructed not to wear their lenses for 3 weeks and 3 days, respectively, before the procedure ( Figure 1 ).
The study was reviewed and approved by the Institutional Review Board of Noor Ophthalmology Research Center and the Iranian Registry of Clinical Trials, a member of the WHO Registry Network (registration number: IRCT201207244333N1; registry date: August 30, 2012). Written signed informed consents were obtained from participants.
Surgical Technique
In the control group, proparacaine hydrochloride 0.5% was used for local anesthesia, and the central 9.0 mm of the corneal epithelium was removed manually using a hokey knife. After removal of the lid speculum, riboflavin drops 0.1% in 20% dextran (Streuli Pharmeceuticals, Uznach, Switzerland) were instilled onto the corneal surface every 3 minutes for 30 minutes. Intraoperative pachymetry was done in all cases before irradiation. At this stage, none of the eyes had corneal thickness under 400 μm to require a swelling solution. After anterior chamber saturation with riboflavin, irradiation was commenced at a wavelength of 370 nm and power of 3 mW/cm 2 from a distance of 5 cm. Irradiation was done using the UVX system (IROC, Zürich, Switzerland). Riboflavin instillation continued every 3 minutes during the 30 minutes of irradiation. At the end of this stage, the corneal surface was rinsed with sterile balanced saline solution, a soft bandage contact lens (Night & Day; Ciba Vision, Duluth, Gorgia, USA) was applied, and a drop of levofloxacin was instilled. Postoperative medications included levofloxacin eye drops 4 times daily, betamethasone 0.1%, and preservative-free artificial tears (Hypromelose, Chauvin, Aubenas, France) as required. Patients were examined on days 1 and 3 after the procedure, and the lens was removed after epithelial healing. After removal of the lens, levofloxacin was discontinued and betamethasone was continued 4 times daily for another week. When the epithelium was not healed, daily visits were continued until complete healing. No case of intraoperative or postoperative complication was observed.
In the treatment group, all steps were similar to the control group, except that irradiation was at 18 mW/cm 2 for 5 minutes using the UV system (PESCHKE Meditrade GmbH, Waldshut-Tiengen, Germany).
Examinations
Examinations included testing for uncorrected distance visual acuity (UDVA) and best corrected distance visual acuity (CDVA) using the Snellen chart, and spherical equivalent (SE) using a retinoscope (ParaStop HEINE BETA 200; HEINE Optotechnik, Herrsching, Germany). We also measured topographic indices with the Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany), corneal biomechanical properties using the Ocular Response Analyzer (ORA; Reichert Ophthalmic Instruments, Buffalo, New York, USA; software version: 3.01), and the ECD with noncontact specular microscopy (Konan Medical, Hyogo, Japan). Treatment results such as demarcation line and potential complications were assessed through slit-lamp (Haag-Streit, Cleveland, Ohio, USA) examinations.
Statistical Analysis
Analysis was done using the intention-to-treat approach. In this report, the main analysis was focused on 18-month changes compared with preoperative values using repeated-measures analysis of variance. Additionally, 18-month changes were compared to 6-month-postoperative results in each group using the same method. Since study power impacts the significance of associations, the powers of the tests used in the analyses were calculated by the Biologically Significant Effect Size approach using the G Power 3.1.9.2 software (Universitate Kiel, Kiel, Germany). The level of significance considered for results was 0.05.
Results
Considering the inclusion criteria, 31 patients (31 eyes in each group) were enrolled in the study. The mean age of the participants was 25.13 ± 4.21 years, and 59.4% of them were male.
Visual and Refractive Results
Table 1 summarizes the vision and refraction data in the 2 study groups. At 18 months, the improvement in UDVA was statistically similar in the 2 groups ( P = .745, power = 67%). CDVA was similarly unchanged in both groups ( P = .551, power = 94%). Eighteen-month changes in spherical error ( P = .415, power = 83%), refractive astigmatism ( P = .370, power = 79%), and spherical equivalent ( P = .178, power = 78%) were not significantly different between the 2 groups.
| Treatment Group | Baseline n = 31 | 6 Months n = 29 | 18 Months n = 30 | P Value a | P Value b |
|---|---|---|---|---|---|
| UDVA (logMAR) | |||||
| Accelerated | 0.72 ± 0.53 | 0.61 ± 0.49 | 0.63 ± 0.49 | .176 | .745 |
| Standard | 0.74 ± 0.50 | 0.72 ± 0.51 | 0.68 ± 0.49 | .107 | |
| CDVA (logMAR) | |||||
| Accelerated | 0.20 ± 0.18 | 0.19 ± 0.17 | 0.20 ± 0.19 | .451 | .551 |
| Standard | 0.22 ± 0.18 | 0.20 ± 0.21 | 0.23 ± 0.22 | .943 | |
| Spherical error (D) | |||||
| Accelerated | −1.44 ± 2.32 | −1.43 ± 2.50 | −1.37 ± 2.48 | .312 | .415 |
| Standard | −1.62 ± 1.80 | −1.67 ± 2.29 | −1.32 ± 2.13 | .124 | |
| Cylinder error (D) | |||||
| Accelerated | −2.45 ± 1.69 | −2.51 ± 1.73 | −2.47 ± 1.70 | .569 | .370 |
| Standard | −2.72 ± 1.92 | −2.78 ± 1.90 | −2.51 ± 1.85 | .487 | |
| SE (D) | |||||
| Accelerated | −2.67 ± 2.70 | −2.56 ± 2.85 | −2.61 ± 2.83 | .479 | .178 |
| Standard | −3.02 ± 2.26 | −3.06 ± 2.65 | −2.58 ± 2.35 | .041 |
a Eighteen months compared to baseline.
Topographic Results
K max showed no significant change in the accelerated group ( P = .407) but significantly decreased in the standard group ( P = .005). The intergroup difference was borderline statistically significant with low power in this regard ( P = .093, power = 68%). The trend of changes in mean keratometry (K mean ) was similar to K max in both groups, and the intergroup difference in K mean changes was borderline statistically significant ( P = .059, power = 72%). CCT decreased similarly in both groups ( P = .324, power = 79%). The Q-value was unchanged in the accelerated group ( P = .366), but shifted to oblate in the standard group ( P = .019); the intergroup difference in this regard was not significant ( P = .426, power = 67%). In terms of changes in keratoconus indices, the intergroup difference was statistically significant for the index of surface variance (ISV) ( P = .034, power = 62%) but not for the index of vertical asymmetry (IVA) ( P = .720, power = 54%), the keratoconus index (KI) ( P = .622, power = 56%), the center keratoconus index (CKI) ( P = .341, power = 77%), the index of height asymmetry (IHA) ( P = .397, power = 70%), or the index of height decentration (IHD) ( P = .409, power = 70%) ( Table 2 ).
| Treatment Group | Preoperative (31 Patients) | Postoperative 6 Months (29 Patients) | Postoperative 18 Months (30 Patients) | P Value a | P Value b |
|---|---|---|---|---|---|
| Maximum keratometry (D) | |||||
| Accelerated | 47.89 ± 3.22 | 48.24 ± 3.48 | 47.83 ± 3.77 | .407 | .093 |
| Standard | 48.77 ± 3.65 | 48.65 ± 3.75 | 48.13 ± 3.18 | .005 | |
| Mean keratometry (D) | |||||
| Accelerated | 46.39 ± 3.28 | 46.44 ± 3.38 | 46.18 ± 3.43 | .309 | .059 |
| Standard | 47.10 ± 2.84 | 46.87 ± 3.14 | 46.39 ± 2.94 | .004 | |
| Central corneal thickness (μm) | |||||
| Accelerated | 489.60 ± 32.32 | 482.89 ± 33.22 | 480.32 ± 36.35 | <.001 | .324 |
| Standard | 489.63 ± 34.94 | 471.70 ± 36.91 | 469.50 ± 38.75 | <.001 | |
| Q-value | |||||
| Accelerated | −0.62 ± 0.25 | −0.66 ± 0.30 | −0.56 ± 0.29 | .366 | .426 |
| Standard | −0.72 ± 0.32 | −0.74 ± 0.44 | −0.64 ± 0.38 | .019 | |
| Index of surface variance | |||||
| Accelerated | 66.23 ± 29.68 | 70.09 ± 30.29 | 65.41 ± 28.73 | .601 | .034 |
| Standard | 77.27 ± 38.92 | 78.27 ± 40.20 | 72.32 ± 35.38 | .001 | |
| Index of vertical asymmetry | |||||
| Accelerated | 0.72 ± 0.35 | 0.77 ± 0.38 | 0.70 ± 0.35 | .095 | .720 |
| Standard | 0.86 ± 0.49 | 0.80 ± 0.42 | 0.81 ± 0.44 | .018 | |
| Keratoconus index | |||||
| Accelerated | 1.17 ± 0.10 | 1.17 ± 0.09 | 1.15 ± 0.09 | .244 | .622 |
| Standard | 1.21 ± 0.13 | 1.19 ± 0.13 | 1.19 ± 0.13 | .008 | |
| Center keratoconus index | |||||
| Accelerated | 1.04 ± 0.03 | 1.04 ± 0.03 | 1.04 ± 0.04 | .900 | .341 |
| Standard | 1.05 ± 0.04 | 1.05 ± 0.05 | 1.04 ± 0.04 | .162 | |
| Index of height asymmetry | |||||
| Accelerated | 24.30 ± 20.12 | 21.64 ± 19.17 | 29.60 ± 25.32 | .097 | .397 |
| Standard | 24.84 ± 20.63 | 29.60 ± 25.32 | 28.19 ± 22.08 | .500 | |
| Index of height decentration | |||||
| Accelerated | 0.08 ± 0.07 | 0.06 ± 0.04 | 0.09 ± 0.05 | .547 | .409 |
| Standard | 0.07 ± 0.05 | 0.08 ± 0.05 | 0.10 ± 0.05 | .061 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


