Purpose
To evaluate the long-term outcomes of vitrectomy for progressive X-linked retinoschisis.
Design
Prospective, nonrandomized, consecutive, interventional case series.
Methods
Twenty-eight eyes of 22 patients who were diagnosed with progressive X-linked retinoschisis were divided into 2 groups: a nonsurgical group (n = 11) and a vitrectomy group (n = 17). The main outcome measures included best-corrected visual acuity, the area of the macular schisis cavity measured by optical coherence tomography, the retinal anatomic status, and complications.
Results
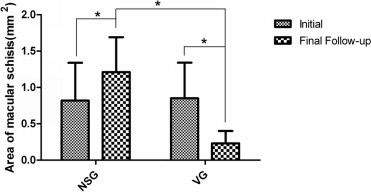
The mean follow-up period was 34.7 months (range, 10 to 68 months). The mean best-corrected visual acuity increased from 20/125 at baseline to 20/55 at the final follow-up in the vitrectomy group ( P = .001), but decreased from 20/100 at baseline to 20/400 at the final follow-up in the nonsurgical group ( P = .000). In the vitrectomy group, the macular schisis cavity resolved in all 17 eyes; the mean area of the macular schisis cavity decreased from 0.85 mm 2 at baseline to 0.23 mm 2 at the final follow-up ( P = .000), and the retinas of 16 eyes (94%) were attached after surgery. In the nonsurgical group, retinal schisis progressively extended in 9 eyes (82%); the mean area of the macular schisis cavity increased from 0.82 mm 2 at baseline to 1.21 mm 2 at the final follow-up ( P = .000); in 8 eyes (72%), retinal detachment developed, and 2 eyes (18%) experienced vitreous hemorrhage, which terminated the observations.
Conclusions
Vitrectomy may be an effective and essential treatment for patients with progressive X-linked retinoschisis to prevent a deterioration of vision before severe complications developed in their eyes.
X-linked retinoschisis caused by mutations of the RS1 gene in Xp22.1 is a human-inherited retinal degenerative disease that leads to schisis of the neural retina. This disease was described first in 1898 by Haas and today is known as X-linked retinoschisis. X-linked retinoschisis is the most common form of juvenile-onset retinal degeneration in males, with a prevalence of 1 in 25 000 to 1 in 5000, and causes vision loss. Females who are heterozygous for the RS1 mutation, however, usually have no clinical symptoms of X-linked retinoschisis. The common sight-threatening complications of X-linked retinoschisis include traction or rhegmatogenous retinal detachment, dense vitreous hemorrhage, intraretinal splitting involving the macula, hemorrhage within a large schisis cavity, and so forth. Other less common complications include neovascular glaucoma, vitreoretinal traction with secondary macular dragging, and optic atrophy. Roughly 20% of all patients with X-linked retinoschisis may progress to retinal detachment, and in up to one third of such patients, vitreous hemorrhage develops, which causes severe vision loss.
Until now, no satisfying treatment has been available to halt the formation and development of schisis in patients with X-linked retinoschisis. Surgical interventions are required for X-linked retinoschisis patients with severe complications such as retinal detachment and vitreous hemorrhage. Currently, the main surgical interventions for X-linked retinoschisis include scleral buckle and vitrectomy with gas or silicon oil tamponade. A stable stage of X-linked retinoschisis generally is considered as having stable retinal function and structure during follow-up, clinical observation rather than surgical intervention thus is needed to monitor the progression of this disorder. However, there were many patients with progressive X-linked retinoschisis from our 15-year clinical observation. A patient with progressive X-linked retinoschisis is defined as a X-linked retinoschisis patient who has no complications like vitreous hemorrhage and retinal detachment but demonstrates progressively decreasing vision together with progressive expanding of macular schisis or progressive peripheral schisis cavity threatening the 5-mm diameter macula area around fovea during more than 6 months of follow-up. It is not yet known if surgical intervention or clinical observation should be performed on patients with progressive X-linked retinoschisis.
Although some positive outcomes of surgical intervention for X-linked retinoschisis patients with complications have been reported, no defined indications, appropriate time periods, or methods for surgical intervention to treat progressive X-linked retinoschisis have been realized fully. From our previous observation, we found that after complications happen, patients with X-linked retinoschisis would have a poor prognosis, including poor visual acuity, even after surgical intervention. Furthermore, we also found that patients with progressive X-linked retinoschisis who do not receive surgical intervention easily can experience severe complications, such as retinal detachment and vitreous hemorrhage. To clarify the effectiveness of vitrectomy for progressive X-linked retinoschisis, we first evaluated the long-term outcomes of vitrectomy for progressive X-linked retinoschisis.
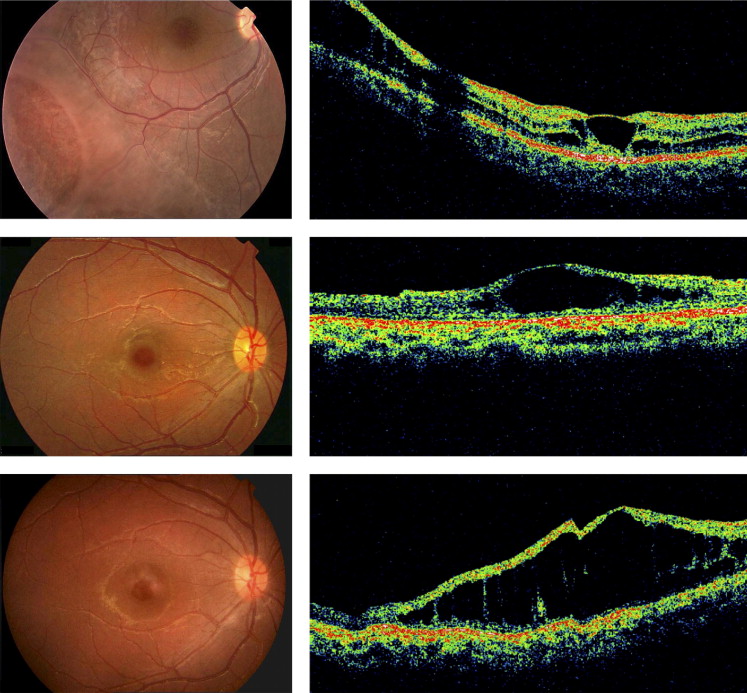
Methods
To evaluate the long-term outcomes of vitrectomy for patients with progressive X-linked retinoschisis, we enrolled 28 eyes of 22 patients with progressive X-linked retinoschisis who were diagnosed at the Zhongshan Ophthalmic Center of Sun Yat-sen University in Guangzhou, China, from February 2004 through June 2010. We confirmed progressive X-linked retinoschisis status based on clinical evidence, including patient symptoms, fundus changes, optical coherence tomography (OCT), fluorescein fundus angiography, and electroretinography. X-linked retinoschisis patients without any complications but with progressively decreasing vision together with progressive expanding of macular schisis or progressive peripheral schisis cavity threatening the 5-mm diameter macula area around fovea during more than 6 months of follow-up were considered to be at the progressive stage in this study ( Figure 1 ) . All patients were male with a mean age of 11.9 years (range, 6 to 34 years). The eyes of 22 patients with progressive X-linked retinoschisis were divided into 2 groups: a nonsurgical group (n = 11) and a vitrectomy group (n = 17). Two eyes of 2 patients in the vitrectomy group underwent laser photocoagulation before the patients were enrolled in this study. All surgeries were performed at the Zhongshan Ophthalmic Center by the same experienced retina specialist (S.T.).
The eyes in the nonsurgical group were under close observation and were examined for their BCVA, fundus features, and OCT results. Laser photocoagulation was performed if the eye had a peripheral schisis cavity threatening the macula. Observation was terminated and surgical intervention was performed if an eye began to exhibit severe complications, such as vitreous hemorrhage or tractional or rhegmatogenous retinal detachment.
All 17 eyes in the vitrectomy group underwent a 23-gauge or 25-gauge sutureless vitrectomy. The surgical procedures were as follows. First, a core vitrectomy and surgery-induced PVD were performed, and then the premacular vitreous cortex was removed completely. After that, internal limiting membrane (ILM) of 2 to 3 disc diameters around fovea was peeled by intraocular forceps, whereas we avoided peeling the ILM over the very weakened retinoschisis area, and only the ILM around this area was peeled. Next, the peripheral vitreous was removed completely, including the dissection of the cortical vitreous from the inner retinoschisis wall. Laser photocoagulation was applied when it was necessary. Finally, 16% C 3 F 8 gas tamponade was performed after a fluid–air exchange. Patients were instructed to maintain a prone position for at least 2 weeks after surgery. The main outcome observations during the follow-up period included BCVA, the status of retinal anatomic features demonstrated on Stratus OCT (Carl Zeiss Meditec Inc, Dublin, California, USA), and postoperative complications such as cataracts, glaucoma, or proliferative vitreoretinopathy (PVR).
The OCT scan length was 5 mm and passed horizontally and vertically through the fovea. In addition, the areas of macular schisis cavities in the horizontal scans of OCT images were calculated by Image-Pro Plus version 5.1 software (Media Cybernetics Co, Bethesda, Maryland, USA). The red line-tagged area represented the schisis cavity, and the area of the macular schisis cavity was calculated by the sum of the red line-tagged area ( Figure 2 , Second row right).
All data were analyzed using the SPSS statistical software version 16.0 (SPSS, Inc, Chicago, Illinois, USA). The paired and independent-samples t tests were used to compare the intragroup and between-group differences, respectively. A P value of less than .05 was considered statistically significant.
Results
The mean follow-up period in this study was 34.7 months (range, 10 to 68 months): 35.3 months (range, 10 to 63 months) for the nonsurgical group and 34.3 months (range, 11 to 68 months) for the vitrectomy group. There was no significant difference in the follow-up period between the 2 groups ( P = .881). The patients’ profiles are shown in the Table .
| Case No. | Eye | Group | Age (y) | Initial BCVA | Final BCVA | Surgical Indication (Laser for NSG) | Operations Procedure | Complications during Follow-up | Final Retinal Status | Follow-up (mos) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | L | NSG | 11 | 20/200 | 1/400 | — | — | VH | VH | 29 |
| 2 | R | NSG | 10 | 20/100 | 20/400 | — | — | TRD | Detached | 49 |
| 3 | R | NSG | 9 | 20/100 | 20/1000 | — | — | TRD | Detached | 27 |
| L | NSG | 9 | 20/67 | 20/250 | PSTM, PDV | P | RRD | Detached | 10 | |
| 4 | R | NSG | 15 | 20/200 | 1/400 | — | — | RRD | Detached | 35 |
| 5 | R | NSG | 16 | 20/100 | 20/200 | — | — | TRD | Detached | 39 |
| 6 | R | NSG | 18 | 20/67 | 20/200 | — | — | RRD | Detached | 15 |
| L | NSG | 18 | 20/100 | 20/333 | — | — | TRD | Detached | 51 | |
| 7 | L | NSG | 7 | 20/50 | 20/500 | PSTM | P | TRD | Detached | 17 |
| 8 | R | NSG | 12 | 20/200 | 20/200 | — | — | — | Attached | 63 |
| 9 | L | NSG | 15 | 20/250 | 1/200 | PSTM, PDV | P | VH | VH | 53 |
| 10 | L | VG | 11 | 20/50 | 20/20 | PSTM | PPV, ILMP, P, G | — | Attached | 36 |
| 11 | R | VG | 6 | 1/200 | 20/100 | EMS, PDV | PPV,ILMP, G | — | Attached | 27 |
| 12 | R | VG | 7 | 20/667 | 20/100 | PSTM, PDV | PPV, P, G | — | Attached | 44 |
| L | VG | 7 | 20/200 | 20/100 | EMS, PDV | PPV, ILMP, G | — | Attached | 48 | |
| 13 | L | VG | 6 | 20/250 | 20/100 | EMS, PDV | PPV, ILMP, G | — | Attached | 23 |
| 14 | L | VG | 8 | 1/400 | 20/200 | PSTM, EMS, PDV | PPV, ILMP, P, G | — | Attached | 13 |
| 15 | R | VG | 34 | 20/67 | 20/67 | EMS, PDV | PPV, ILMP, G | — | Attached | 40 |
| 16 | R | VG | 13 | 20/500 | 20/100 | EMS, PDV | PPV, ILMP, G | HIOP | Attached | 53 |
| L | VG | 13 | 20/200 | 20/25 | EMS, PDV | PPV, ILMP, G | — | Attached | 53 | |
| 17 | R | VG | 11 | 20/200 | 20/33 | PSTM, PDV | PPV, P, G | — | Attached | 15 |
| L | VG | 11 | 20/100 | 20/100 | PSTM | PPV, ILMP, G | — | Attached | 19 | |
| 18 | L | VG | 9 | 20/50 | 20/33 | EMS, PDV | PPV, ILMP, P, G | — | Attached | 43 |
| 19 | L | VG | 13 | 20/40 | 20/40 | PSTM | PPV, ILMP, P, G | — | Attached | 68 |
| 20 | R | VG | 12 | 20/100 | 20/50 | EMS, PDV | PPV, ILMP, G | — | Attached | 19 |
| 21 | L | VG | 8 | 20/200 | 20/400 | PSTM, PDV | PPV, P, G | ERM, PVR, TRD | Detached | 11 |
| 22 | R | VG | 10 | 20/200 | 20/67 | EMS, PDV | PPV, ILMP, P, G | — | Attached | 35 |
| L | VG | 10 | 20/400 | 20/100 | EMS, PDV | PPV, ILMP, G | — | Attached | 36 |
Anatomic Status of the Retinas
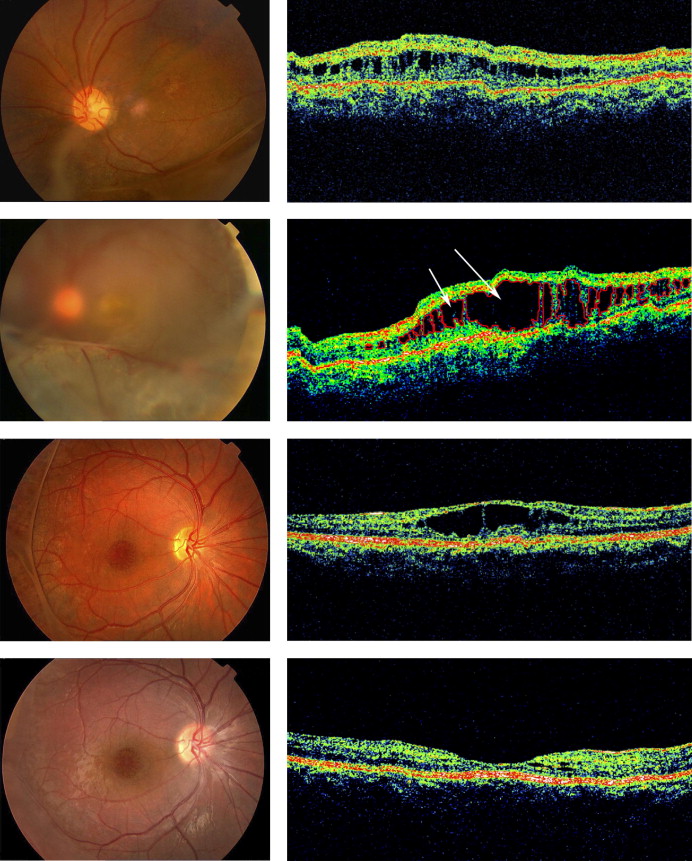
In the nonsurgical group, the retina remained attached in only 3 eyes (27%) at the final follow-up, tractional retinal detachment developed in 5 (45%) eyes, and rhegmatogenous retinal detachment occurred in 3 (27%) eyes during the 10 to 51 months of follow-up. In the vitrectomy group, the retina remained attached in 16 eyes (94%) after the primary surgery, and only 1 eye (6%) had retinal detachment 11 months after the first vitrectomy, but achieved retinal attachment with a second vitrectomy.
The OCT images showed that in the nonsurgical group, the macular schisis cavity expanded in 6 eyes (55%) ( Figure 2 , Top and Second rows) and the peripheral retina schisis extended in 3 eyes (27%); the mean area of the macular schisis cavity increased from 0.82 to 1.21 mm 2 ( P = .000; Figure 3 ) . In the vitrectomy group, the macular schisis cavity resolved greatly in all 17 eyes after surgery ( Figure 2 , Third and Bottom rows), and the mean area of the macular schisis cavity decreased from 0.85 to 0.23 mm 2 ( P = .000; Figure 3 ). There was no significant difference in the initial mean area of macular schisis between the nonsurgical and vitrectomy groups ( P = .865), whereas the final mean area of macular schisis in the nonsurgical group was significantly larger than that of the vitrectomy group ( P = .000; Figure 3 ).