Purpose
To evaluate the long-term clinical outcomes of 0.1% tacrolimus dermatologic ointment (Protopic) in cases of refractory atopic keratoconjunctivitis (AKC).
Design
Prospective, nonrandomized, noncontrolled case series.
Methods
Twenty-two eyes from 11 patients with severe AKC who were treated with 0.1% tacrolimus ointment were followed prospectively. The mean age of the patients was 32.27 ± 12.7 years (range, 19-61 years). Each patient completed a follow-up period of at least 48 months, during which the signs and symptoms of AKC were assessed. Changes in the total scores of signs and symptoms from baseline were recorded at each visit, and the main outcome measure was the clinical response to topical tacrolimus treatment.
Results
Dramatic improvements in clinical signs and symptoms were achieved 1 week after starting topical tacrolimus treatment, and complete clinical resolution was observed in almost all patients 6 weeks after starting treatment. Treatment was gradually reduced, with increasing intervals between applications. Eight patients remained asymptomatic for up to 3 years, although recurrence occurred in 3 patients who attempted to discontinue treatment. All patients complained of a mild burning sensation upon application of the ointment. No additional medications were required to provide relief, and no patient discontinued treatment because of adverse drug effects. No drug-related ocular complications were encountered, and no significant changes in visual acuity or refraction were documented.
Conclusions
Tacrolimus dermatologic ointment is a potentially safe and effective treatment for AKC cases refractory to standard treatment and may substitute for steroid treatments aimed at controlling disease activity.
Atopic keratoconjunctivitis (AKC) is a chronic atopic disease of the conjunctiva. It is the most serious type of allergic conjunctival disease because of the associated corneal and lenticular complications. In severe cases, subepithelial fibrosis of the conjunctiva, fornix shortening, symblepharon, corneal ulceration and neovascularization, and cataracts may occur. Atopic dermatitis is considered the most common systemic association. Symptoms of AKC include itching, burning, photophobia, and foreign body sensation, and the clinical signs include eczematous lid changes, conjunctival injection, edema, papillae on the upper tarsal conjunctiva, and corneal punctate erosions. Antihistamines or mast cell stabilizers are often insufficient to control AKC; therefore, the addition of steroids may be required to give patients symptomatic relief. However, the side effects of these steroids include cataracts, glaucoma, herpetic keratitis, eyelid skin atrophy, and depigmentation. In addition, immunosuppressive medications, such as steroid-sparing agents, have been introduced to relieve patient symptoms, reduce disease morbidity, and avoid the serious side effects of steroids. Topical cyclosporine is effective but can result in an intense stinging sensation with topical application, leading to poor compliance. Therefore, although 0.05% cyclosporine emulsion has been shown to be effective for use in AKC patients, its clinical efficacy was not sufficient in some steroid-dependent cases.
Tacrolimus (formerly FK-506) is a nonsteroidal, strong immunosuppressant isolated from Streptomyces tsukubaensi and demonstrates a much higher potency than cyclosporine (up to 100 times). Tacrolimus suppresses T-cell activation, T helper cell–mediated responses, B-cell proliferation, and cytokine release, especially that of interleukin 2. This drug acts by forming a complex with its cytosol partner FK506-binding protein 12, which also binds calcineurin. As a result, both calcineurin inhibitors (CIs) inhibit the phosphatase-controlled translocation of nuclear factor of activated T cells (NFAT) into the nucleus and prevent the induction of cytokines and expression of their receptors, which helps to prevent the activation and proliferation of lymphocytes and other immune cells. Eosinophil cationic protein (ECP), which is released from the secretory granules of eosinophils upon activation, has been shown to play an important role in the pathogenesis of allergic conjunctivitis; for example, tear ECP levels in allergic patients were found to be linked to the severity of clinical disease. Although systemic tacrolimus has been used to treat allergic eye disease, there is no commercially available ophthalmic preparation for tacrolimus. Therefore, dermatologic tacrolimus ointment has been used instead. Previous studies have reported improvements in the symptoms of conjunctivitis, without significant side effects, following treatment with tacrolimus ointment in atopic blepharoconjunctivitis. Topical tacrolimus ointment (0.02%-0.1%) has also been used to treat giant papillary conjunctivitis, AKC, and vernal keratoconjunctivitis (VKC), with good results. Furthermore, a 0.1% tacrolimus ophthalmic suspension has been used for the treatment of AKC and VKC with only 4 weeks of follow-up. The purpose of this study was to evaluate the long-term clinical outcomes with the use of tacrolimus ointment for refractory AKC.
Methods
This prospective, nonrandomized, noncontrolled case series included 22 eyes from 11 patients with active AKC who were refractory to conventional treatments. The Institutional Review Board of King Khalid University in Abha, Saudi Arabia, approved the study protocol. Patients were recruited from Abha Private Hospital and Aseer Central Hospital after written informed consent was obtained to participate in this study.
Atopic keratoconjunctivitis was diagnosed with a typical history including chronic, bilateral itching, redness, and signs of thickened scaly lid conjunctival hyperemia; papillae on the upper tarsal conjunctiva; and corneal erosions. All of the included patients were steroid dependent, and their diseases were active despite treatment with cyclosporine as well as conventional treatments, such as antihistamines, mast cell stabilizers, and topical nonsteroidal anti-inflammatory medications. The patients were asked to discontinue all other medications, including topical or systemic immunosuppressive medications, 1 week before beginning treatment with tacrolimus ointment. The exclusion criteria consisted of coexisting conjunctival disorders, chemical injury, Stevens-Johnson syndrome, corneal diseases, uveitis, ocular infections, contact lens use, a history of using systemic nonsteroidal anti-inflammatory medications or immunosuppressive drugs, and ocular surgery within the previous 3 months.
Complete ophthalmic examinations, including the assessment of best spectacle-corrected visual acuity (BSCVA), slit-lamp biomicroscopy, fluorescein staining, funduscopy, and applanation tonometry, were conducted. Prior to the initiation of the study, the advantages and disadvantages of the treatment were explained to the patients. All patients with severe AKC were instructed to apply tacrolimus 0.1% dermatologic ointment (Protopic; Astellas Pharma Inc., Northbrook, Illinois, USA) into the inferior conjunctival fornix of each eye once daily for 1 week followed by weekly tapering (ie, every other day for 1 week, twice a week for 1 week, and once a week afterwards). The patients with moderate AKC were advised to use the tacrolimus ointment once every other day for 1 week, tapering to twice a week in the following week and once a week thereafter. The dosing for patients with mild AKC was twice a week for the first week and then once a week thereafter. During treatment, patients returned for evaluation after 1 week, 4 weeks, and 6 weeks, and every 6 months thereafter. The main outcome measures were graded according to the clinical severity of disease at each visit and included symptoms of itching or redness, foreign body sensation, signs of lid thickening, conjunctival hyperemia, the presence of papillary hypertrophy of the superior tarsal conjunctiva, and superficial punctate keratopathy. The patients’ signs and symptoms were graded on a 4-point scale, and the severity of each sign or symptom was graded using the following scale: 0 (no symptoms); 1 or mild (occasional symptoms); 2 or moderate (frequent symptoms); and 3 or severe (constant symptoms) ( Table 1 ). The change in the total scores of signs and symptoms from baseline at each visit was recorded.
| Sign | Score | Definition |
|---|---|---|
| Conjunctival hyperemia | 3 | Diffuse dilated blood vessels over the entire bulbar conjunctiva |
| 2 | Dilation of many vessels | |
| 1 | Dilation of few vessels | |
| 0 | None | |
| Lid thickening and/or scales | 3 | Severe |
| 2 | Moderate | |
| 1 | Mild | |
| 0 | None | |
| Papillae | 3 | Papillae size: more than 0.3 mm |
| 2 | Papillae size: 0.2-0.3 mm | |
| 1 | Papillae size: less than 0.2 mm | |
| 0 | None | |
| Superficial punctate keratopathy | 3 | Total corneal surface |
| 2 | More than half corneal surface | |
| 1 | Less than half corneal surface | |
| 0 | None |
All data were analyzed using a statistical software package (SPSS Inc, Chicago, Illinois, USA). An analysis of variance (ANOVA) and the paired t test were used to statistically analyze changes in the mean scores of signs and symptoms following treatment with topical 0.1% tacrolimus ointment; P values of .05 or less were considered statistically significant.
Results
Twenty-two eyes from 11 patients (10 male and 1 female) with refractory AKC were included in this study. These patients had a mean age of 32.27 ± 12.7 years (range, 19-61 years), and all had experienced bilateral involvement of AKC for a mean duration of 7.63 ± 4.90 years (range, 3-20 years) ( Table 2 ).
| Patient No. | Sex/Age (y) | AKC Duration (y) | Treatment Duration (mo) | Follow-up (mo) |
|---|---|---|---|---|
| 1 | M/20 | 10 | 9 | 60 |
| 2 | M/36 | 7 | 63 | 63 |
| 3 | M/27 | 6 | 10 | 58 |
| 4 | M/61 | 20 | 11 | 56 |
| 5 | M/23 | 11 | 63 | 63 |
| 6 | F/19 | 3 | 11 | 49 |
| 7 | M/29 | 9 | 8 | 52 |
| 8 | M/30 | 4 | 12 | 55 |
| 9 | M/51 | 6 | 6 | 54 |
| 10 | M/34 | 5 | 12 | 51 |
| 11 | M/25 | 3 | 63 | 63 |
All patients had active perennial symptomatic disease despite previous use of various medications, including antihistamines, mast cell stabilizers, topical cyclosporine, and steroids. Itching was the most prominent symptom, with other complaints including redness and foreign body sensation. All patients had a history of atopic dermatitis, and all eyes examined had lid thickening, conjunctival hyperemia, and papillary conjunctivitis.
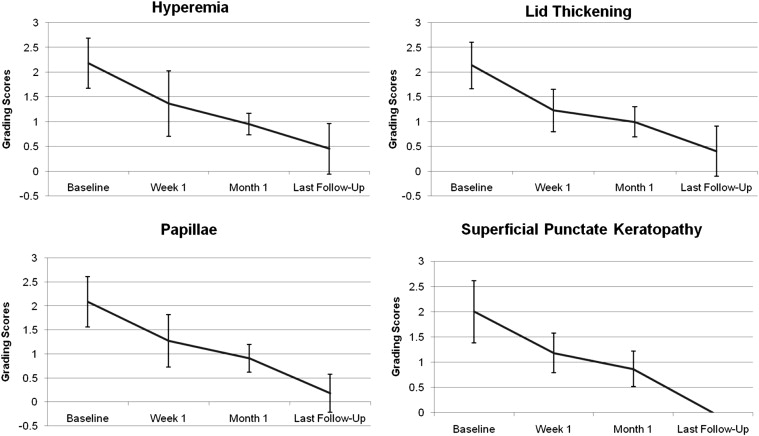
After starting treatment with 0.1% tacrolimus dermatologic ointment (Protopic), the patients were followed for a mean duration of 54.18 ± 4.75 months (range, 49-63 months). The changes in their mean scores of symptoms following tacrolimus treatment are shown in Figure 1 .
All symptoms significantly improved after treatment, and itching was the first symptom to show improvement. Previously, 3 of the patients had suffered from severe itching and the other 8 patients had suffered from moderate itching; but 1 week after starting treatment with tacrolimus ointment, all of the patients showed a dramatic improvement in itching. After 1 month, all patients achieved complete resolution of their symptoms ( Figure 1 ).
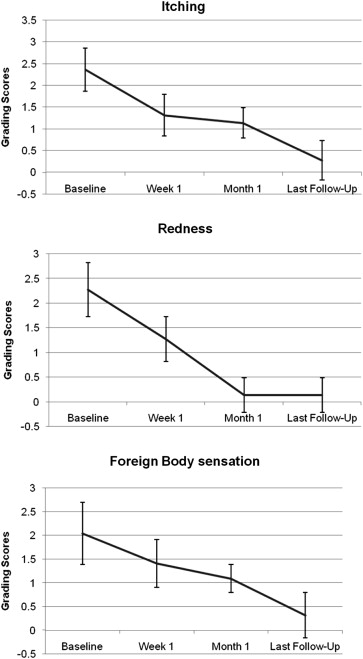
At the end of the follow-up period, the patients remained asymptomatic but continued to apply topical tacrolimus ointment. No additional medications, such as mast cell stabilizers, topical cyclosporine, or steroids, were required to provide additional relief to patients. We observed a dramatic improvement in the patients’ clinical signs of disease after starting tacrolimus treatment ( Figure 2 ).