Ligneous Conjunctivitis
Peter C. Donshik
Melinda L. Ramsby
Gregory S. Makowski
BACKGROUND
Ligneous conjunctivitis is a rare form of chronic conjunctivitis first described in 1847 by Bouisson (1) as a case of pseudomembranous conjunctivitis. In 1933, Borel (2) described a young girl with bilateral membranous conjunctivitis and indurated eyelids. Borel was the first to use the term ligneous to describe the wood-like feeling of the indurated eyelids in this patient. In the last 70 years less than 150 cases have been reported. Ligneous conjunctivitis most commonly afflicts the upper eyelid, but can involve all palpebral surfaces. The course of ligneous conjunctivitis is typically one of recurrence and remission that persists for months, years, or throughout life.
EPIDEMIOLOGY
Ligneous conjunctivitis has a predilection for young children usually between the ages of 2 and 6 years but has been reported to occur as early as the first week of life (3) and as late as 85 years (4). In 119 reported cases, the average age of onset was 13.9 years whereas the median age of onset was 5 years (5). There is a female predilection (3:1), and familial cases suggest an autosomal-dominant transmission (6). In addition to the conjunctiva, ligneous lesions can involve other mucosal membranes including the mouth, nasopharynx, trachea, larynx, alveolar and tympanic membranes, vagina, cervix, and fallopian tubes (7, 8, 9). Cases also arise in association with antecedent infection, trauma, pinguecula, pterygium, cataract, and ptosis surgery (5,10, 11, 12), consistent with a role for injury in initiating the ligneous process.
CLINICAL
Ligneous conjunctivitis usually begins with an acute onset and then becomes chronic. It is unaffected by topical antibiotics or steroids. Lesions typically start with nonspecific indicators of mucosal irritation such as tearing and conjunctival hyperemia. Disease progression is characterized by the formation of friable pseudomembranes composed of loose fibrovascular tissue that is easily removed from the underlying conjunctiva but associated with profuse bleeding (Fig. 33-1). As the disease continues, a thick mass develops on top of the fibrovascular pseudomembrane and this new pseudomembrane is thick, firm, and “woody” (Fig. 33-2). These late stage lesions are tightly adherent to the underlying conjunctiva and are difficult to remove. Once removed, lesions tend to rapidly reoccur (Fig. 33-3). With continued inflammation the lid may become indurated.
The ligneous plaque can appear sessile or pedunculated, with a flat, smooth surface that is white or yellowish white in color (Fig. 33-4). The upper and lower (upper more common than lower) palpebral conjunctiva are the usual surfaces affected, but the bulbar conjunctiva can also be involved (Fig. 33-5). Although usually bilateral, the disease may present in an asymmetrical fashion with the first eye being more severely involved. The disease can progress for months or years, and approximately one third of cases undergo spontaneous regression.
Symptoms of discomfort, tearing, photophobia, and difficulty keeping the eye open can be mild or severe. Vision is usually unaffected. The chronic inflammation can cause ptosis of the lid (Fig. 33-6), and amblyopia can develop. Further, if the condition spreads to the limbus, the possibility of corneal complications such as opacification, neovascularization and perforation can arise (2). In the early stages, ligneous conjunctivitis can be confused with other pseudomembranous conjunctivitis. However, the chronic conjunctival inflammation, as well as recurrence of the pseudomembrane after removal, helps differentiate ligneous conjunctivitis from other conditions.
PATHOLOGY
Histologic examination of the ligneous pseudomembrane reveals acute and chronic fibrinous inflammation. Areas of
vascular and fibrinous organization are apparent, as are foci of granulation tissue exhibiting a variable cellular component of plasma cells, eosinophils, mast cells, lymphocytes, and neutrophils. Activated T cells and B lymphocytes have also been reported (13). Less consistent are the presence of focal epithelial degeneration, hypertrophy, submucosa invasion, and vascular degeneration with endothelial gaps (14).
vascular and fibrinous organization are apparent, as are foci of granulation tissue exhibiting a variable cellular component of plasma cells, eosinophils, mast cells, lymphocytes, and neutrophils. Activated T cells and B lymphocytes have also been reported (13). Less consistent are the presence of focal epithelial degeneration, hypertrophy, submucosa invasion, and vascular degeneration with endothelial gaps (14).
 FIGURE 33-1. A: Thick pseudomembrane involving the upper lid in a 25-year-old woman. B: Everted upper lid showing the thick pseudomembrane attached to the upper tarsal surface. C: Removal of the pseudomembrane with associated bleeding.(see color image) |
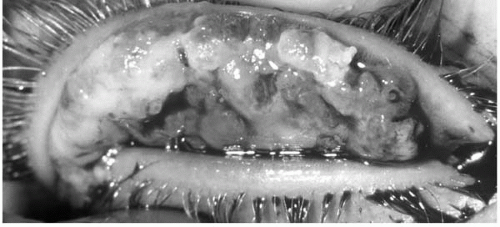 FIGURE 33-2. Thick firm woody appearance of the superior tarsal surface.(see color image) |
The hallmark of the ligneous lesion is the large, amorphous pools of relatively acellular, eosinophilic fibrils within the lamina propria and submucosa (Fig. 33-7). Electron microscopy of these amorphous deposits (Fig. 33-8) demonstrates tactoids of parallel filaments with cross striations and ultrastructural features characteristic of fibrin. Histochemical and immunochemical analyses reveal minor quantities of mucopolysaccharide, immunoglobulin G (IgG) and albumin (8), but unanimously confirm that fibrin is the major component of the ligneous plaque (7, 8, 9,14, 15, 16).
BIOCHEMISTRY
Biochemical analysis performed in our laboratory (17) demonstrate that the ligneous lesion is composed of mucoid and
ligneous compartments. The mucoid fraction represents an exaggerated mucus thread and is easily harvested from the conjunctival cul-de-sac in affected eyes. The ligneous plaque is proteinaceous and not surprisingly, enriched in fibrin (Fig. 33-9): both intact β-monomers and γ-γ dimers (degradation-resistant cross-linked products of transglutaminase). The protease profile of mucoid and ligneous compartments is also distinct. Specifically, the ligneous compartment is selectively enriched in tissue plasminogen activator (tPA) (Fig. 33-10), and all three isoforms of matrix metalloproteinase-9 (MMP-9) (Fig. 33-11). In contrast, the mucoid compartment is relatively devoid of protein, and contains mostly inactive forms of MMP-9 and no tPA (Figs. 33-10 and 33-11).
ligneous compartments. The mucoid fraction represents an exaggerated mucus thread and is easily harvested from the conjunctival cul-de-sac in affected eyes. The ligneous plaque is proteinaceous and not surprisingly, enriched in fibrin (Fig. 33-9): both intact β-monomers and γ-γ dimers (degradation-resistant cross-linked products of transglutaminase). The protease profile of mucoid and ligneous compartments is also distinct. Specifically, the ligneous compartment is selectively enriched in tissue plasminogen activator (tPA) (Fig. 33-10), and all three isoforms of matrix metalloproteinase-9 (MMP-9) (Fig. 33-11). In contrast, the mucoid compartment is relatively devoid of protein, and contains mostly inactive forms of MMP-9 and no tPA (Figs. 33-10 and 33-11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


