LASIK Complications and Management
Christopher J. Rapuano
▪ Introduction
The significant advantages of LASIK over photorefractive keratectomy (PRK) are somewhat tempered by the increased complexity of the surgery, which increases the type and severity of complications. While the risk of complications is low, when a complication occurs, it needs to be managed appropriately to achieve the best chance of a satisfactory result. Additionally, surgeons should continue to strive to minimize complications. This chapter will focus on intraoperative and postoperative complications and their causes, prevention, and management. It may be helpful for the reader to refer to Chapter 10 on retreatment as needed for a more detailed discussion of the indications and techniques related to re-lifting a LASIK flap. Use the intraoperative and postoperative planning index to find representative cases that demonstrate each of the complications discussed.
▪ Intraoperative Complications
SHREDDED FLAP
A shredded flap is one of the most feared complications of LASIK. It is typically only recognized after the microkeratome has made its pass and is removed from the eye. The surgeon may notice the flap to be somewhat irregular. Otherwise, it becomes obvious when the surgeon attempts to lift the flap and does not find a standard flap attached at a hinge.
Causes
Poor suction or pseudosuction. Most, if not all, modern microkeratome systems alert the surgeon when the machine senses adequate suction on the eye and will allow the microkeratome to pass only after suction is achieved. However, if the suction port or ports are occluded by conjunctiva, the machine can measure full suction without the intraocular pressure (IOP) being adequately elevated. This situation is termed pseudosuction. Patients with redundant or boggy conjunctiva, such as might occur in association with thyroid orbitopathy, after retinal surgery or after multiple attempts at achieving suction, are at greater risk for pseudosuction.
Poor blade quality. If a pass is made with an imperfect blade, the result may be a poor-quality flap. The exact condition of the blade will impact both the nature and the degree of flap damage.
Recutting a flap. Recutting a LASIK flap is a retreatment option, but a second flap may intersect with the first flap, resulting in an irregular flap and an irregular stromal bed. Because of this risk, recutting a flap is considered a less desirable approach to retreatment.
Attempting to create a thin flap. LASIK on the second eye using a microkeratome with the same blade will generally result in a thinner flap. Microkeratomes may cut thinner flaps in thin corneas. The femtosecond laser can also be set to a thickness <100 µm. In any of the above situations, flaps thinner than expected may result and the flap may be of poor quality. A shredded flap is less likely with the femtosecond laser.
Prevention
Obtain sufficient exposure. Poor suction can occur due to difficulty positioning the microkeratome onto the eye. This is more likely to occur when exposure is inadequate. The surgeon may notice a hissing sound, if suction is insufficient.
Press the ring firmly against the globe. Firm posterior pressure on the suction ring presses the redundant conjunctiva against the sclera. This may help reduce the risk of pseudosuction.
Triple check the IOP:
First: As the pressure in the eye is increasing, the surgeon should monitor the pupil, which often dilates slightly and then remains enlarged.
Second: Once the machine registers full suction, the IOP should be high enough to obstruct blood flow to the eye and the patient will usually notice the vision dimming or even blacking out.
Third: Check the IOP. This can be done with a Barraquer tonometer, pneumotonometer, TonoPen, or even with digital palpation. The pressure should be >65 mmHg to obtain a quality flap with a blade microkeratome.
Check the blade. The surgeon or an experienced technician should always check the quality of the blade prior to seating it in the microkeratome.
Avoid recutting a LASIK flap for retreatment. Other retreatment options are reliable and safer.
Be cognizant of the risk of creating a very thin flap. Consider PRK if the cornea is thin. Consider using a new microkeratome blade or a thicker plate on the second eye to avoid the risk of a shredded flap.
Management
ABORT THE EXCIMER LASER ABLATION.
Replace flap pieces as best as you can. The goal is to put all of the pieces of the shredded flap back into their original location. This is often quite difficult because there may be multiple small fragments of essentially clear cornea.
Place a bandage soft contact lens (BSCL). The BSCL is usually removed 1 to 7 days later. Topical antibiotic and topical corticosteroid eyedrops are applied in routine fashion with the lens in place and after the lens is removed.
Long-Term Management
Later options include no refractive surgery, transepithelial PRK with or without mitomycin-C, and LASIK with a femtosecond laser setting a significantly deeper flap depth.
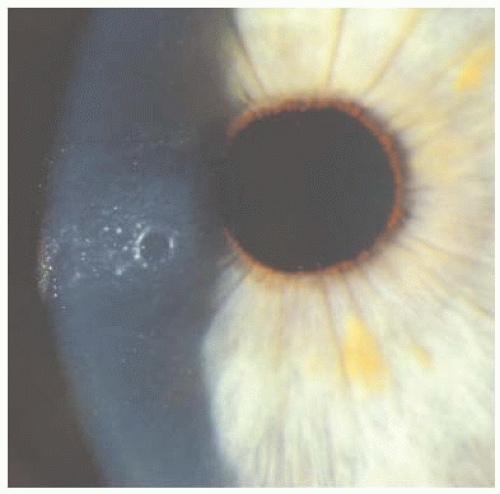
BUTTONHOLE FLAP
Buttonhole flaps (Fig. 11.1) have been described in eyes with normal corneal curvature, but steep corneas appear to be at increased risk, when using a blade microkeratome. The surgeon must always closely examine the quality of the flap as it is being lifted and reflected. Special attention should be paid to the central and paracentral cornea, looking for a fullthickness (easy to detect) or partial-thickness (harder to detect) buttonhole. Buttonholes are easier to detect on the stromal bed appearing as an area of elevation or a smooth island of tissue, but can also be seen as an irregularity or hole in the underside of the flap as it is lifted (Fig. 11.2). Although rare, buttonholes can occur with the femtosecond laser.
Causes
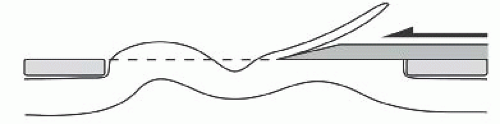
Steep cornea (≥48.00 diopters [D]). The proposed mechanism for steep corneas
predisposing to buttonholes is that when suction is applied, the steepness allows a large amount of tissue to be “pushed up,” above the plane of the suction ring. As this large area of corneal tissue is deformed by the mechanical microkeratome pass, it buckles posteriorly to the plane of the blade and is left uncut, creating a buttonhole (Fig. 11.3).
Localized corneal thinning or scarring. A localized area of stromal loss or scarring may be covered by thickened epithelium. As the flap is made, there may be a full-thickness stromal defect that is covered only by tenuous epithelium.
Partial- or full-thickness buttonholes can occur during the femtosecond laser pass as gas passes through a focal area of corneal thinning or scar. Alternatively, it can result from a traumatic flap lift or from debris on the applanation lens that causes focal posterior displacement of the cornea with resultant focal superficial femtosecond laser ablation.
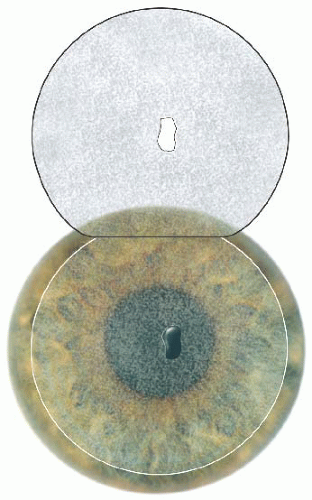 FIGURE 11.2 Smooth, elevated contour of a full-thickness buttonhole noted in the stromal bed, with a corresponding hole noted in the flap. |
Prevention
Use an appropriate suction ring (e.g., use an 8.5-mm suction ring when K > 45.00 D). Most microkeratome systems are designed with a variety of suction rings. Smaller rings do not allow as much corneal tissue to protrude anteriorly. Follow the manufacturer’s recommendations regarding which suction ring size to use, based on the keratometry readings.
Femtosecond laser. The risk of a buttonhole is less because the applanating lens flattens the cornea within the suction ring and there is no mechanical pass across the cornea to induce a buckling of tissue. Consider using a thicker flap if possible when a scar or corneal facet is present within the margins of the flap. Gentle flap dissection can prevent a traumatic flap dissection. If a gas bubble is seen during the laser pass in an area of scar, extra care should be taken during flap dissection. These are very rare situations. In general, the femtosecond laser is safer than a blade microkeratome for the patient with a steep cornea.
Surface ablation. If steep keratometry readings or areas of corneal scarring/thinning are noted preoperatively, the surgeon may want to avoid the possibility of a LASIK flap complication and perform a surface ablation.
Management
DO NOT LASER.
Replace the flap as best as you can.
Place a BSCL, in the event of a full-thickness buttonhole. The BSCL is usually removed 1 to 7 days later.
Long-Term Management
Later options include no refractive surgery, transepithelial PRK (with or without mitomycin-C), and LASIK (using a microkeratome with a thicker plate or a deeper femtosecond laser ablation) (See Video 20).
SHORT OR DECENTERED FLAP WITH AN EDGE IN LASER TREATMENT ZONE
The LASIK flap needs to be properly centered and large enough to accommodate the entire centered excimer laser ablation. A 6-mm-diameter ablation does not require as large a flap as an 8-mm-diameter wavefront-guided custom ablation or a 9-mm hyperopic correction.
Causes
Poor centration of the microkeratome or femtosecond laser. The suction ring should be centered on the pupil or slightly decentered toward the planned hinge location. It may slip slightly or the globe might rotate under the ring as suction is applied to the eye.
Small flap. The flap may be too small to allow the full laser ablation size. This may be due to inadequate suction prior to the pass or due to a flat corneal contour with keratometry readings ≤40.00 D.
Incomplete flap. Loss of suction during the mechanical microkeratome pass might result in a foreshortened flap. An incomplete flap can occur with the femtosecond laser if suction is lost, if the applanation pressure is light, if fluid is present under the applanation lens, or if the meniscus is too close to the flap edge (See Video 13). Refer to Chapter 5 for a more complete discussion of the femtosecond laser.
Prevention
Re-center the suction ring. If the suction ring is decentered, suction should be released and the ring repositioned properly before the microkeratome or femtosecond laser pass. Some femtosecond lasers (e.g., IntraLase) have a toggling function that allows for minor readjustments of centration; however, the diameter of the flap decreases when this is done. Many femtosecond lasers do not have this capability.
Management
Use the reticle. If the flap has been created, use the excimer laser reticle to determine whether the treatment zone will fit entirely beneath the flap. If the hinge is slightly encroaching within a large (e.g., 8- or 9-mm diameter) ablation zone, then the laser treatment can most likely proceed safely. The hinge should be covered with a hinge protector when the treatment zone is large. Ablation of the hinge should be prevented to avoid a doubly treated area. Laser system software that can design a hingesparing ablation may exist on the particular excimer laser being used. Check with the medical director of the laser center.
DO NOT LASER if flap size is inadequate. If the flap does not cover the vast majority of the treatment zone, it is best to abort the excimer laser procedure.
Do not attempt another blade microkeratome pass during the same surgery session. The femtosecond laser is more versatile in this situation. At the first sign of a significant incomplete laser ablation, stop the femtosecond laser. Using the same applanation cone, the laser can be reset, the surface dried, and, if good applanation can be achieved, another laser pass attempted. The pocket should not be cut on the second pass of the femtosecond laser. Usually, an adequate flap can be created with this second pass; however, if the stromal bed appears very irregular, it may be best to abort the excimer laser procedure.
Do not try a lamellar dissection to increase flap diameter. Attempting to increase the flap diameter with a blade is very likely to cause irregular astigmatism and a poor visual outcome. In some cases after a femtosecond laser flap has been created, a small area of incomplete ablation can successfully be bluntly dissected.
Replace the flap. If the flap is inadequate, replace it as one would replace a routine LASIK flap.
Late Management
Later options include no refractive surgery. After waiting for 3 to 6 months, one could attempt to repeat microkeratome or femtosecond LASIK with a larger and thicker flap. Finally, surface ablation with or without mitomycin-C could be considered. Surface ablation over a previous flap increases the risk of haze.
FREE CAP
Automated lamellar keratoplasty, the predecessor to LASIK, and original LASIK techniques were performed by creating a free cap. The current hinged-flap technique improved wound alignment and the safety of the LASIK procedure. While there are reports of free caps occurring in eyes with normal corneal curvature, the risk is increased in patients with flat corneas when using a blade microkeratome.
The presence of a free cap (see Case 66, Fig. 1, Chapter 16) is not always a disaster, particularly if it is discovered right away and prompt, appropriate action is taken. The surgeon must immediately recognize that a free cap was created before the technician removes and disassembles the blade microkeratome, potentially losing the cap. Noting that part of the corneal ink mark is missing following the microkeratome pass and observing an irregular light reflex as the microkeratome is removed from the eye are key findings. The free cap must be gently removed from the microkeratome unit and placed epithelial side down on a thin layer of saline. If the ink marks are disappearing, they may need to be augmented to ensure correct cap placement. If the cap looks like a jigsaw puzzle piece, it should fit perfectly on the stromal bed when it is replaced. If the cap does not fit perfectly, it may be upside down.
Causes
Flat cornea (K ≤ 40 D). It is suspected that when suction is applied, the flat contour does not allow enough tissue to protrude above the plane of the suction ring. As the blade cuts across, a small free cap is created.
Poor microkeratome ring suction. Poor suction also results in inadequate tissue protruding through the ring.
Inadequate docking of the femtosecond laser with the suction ring.
Improper settings for the microkeratome. If the settings (e.g., ring size on the console does not match the size used, incorrect hinge width) of the microkeratome are incorrect, there is an increased risk of flap complications.
Torn hinge
Prevention
Use a large suction ring on a flat cornea (e.g., 9.5-mm Hansatome ring). Using a larger suction ring allows a greater amount of tissue to protrude anteriorly, ideally creating a normal-sized, hinged flap.
Femtosecond laser. Successful flap creation with the femtosecond laser system is less dependent on corneal curvature and is, therefore, less likely to create a free cap. Careful attention to the docking procedure and recognition of suction loss is necessary.
Surface ablation. If flat keratometry readings are noted preoperatively, the surgeon may prefer to perform a surface ablation. This is particularly true if a femtosecond laser is not an option.
Management
The size and centration of the free cap will determine the ability to perform the laser ablation. If the free cap is as large as the laser treatment zone, the laser treatment may be safely performed, provided the area of exposed stroma is well centered. If the laser ablation zone is larger than the stromal bed, do not perform the excimer laser treatment.
Position the free cap dull side (stroma) posteriorly and shiny side (epithelial) anteriorly. The ink marks should line up, ensuring correct orientation and that the epithelial side is anterior. Place both a BSCL and a shield. Some surgeons place one or more sutures to secure the flap in position. However, sutures in a small free cap may cause distortion within the visual axis.
INTERFACE DEBRIS
Small amounts of interface debris are common and usually inconsequential. They may create tiny interface scars.
Cause
Interface opacities can come from numerous sources, including makeup, meibomian gland secretions, epithelium, metallic blade fragments, and poor cleaning of the microkeratome.
Prevention
Instruct the patient to avoid face or eye makeup on the day of surgery.
Careful removal of makeup the night before surgery.
Cleansing the eyelids of residual makeup.
Treating meibomian gland dysfunction (MGD) and blepharitis preoperatively.
Meticulous cleaning of equipment and use of disposable equipment may help decrease interface debris.
Aggressive irrigation of the flap interface with balanced salt solution, using irrigating cannulas, such as the Viduarri (BD Visitec No. 585216) or the Manche cannula (Asico AE-7281).
Use of an aspirating eyelid speculum such as the Lieberman speculum (Asico AE-1040A).
Management
Irrigate significant interface debris before leaving the laser room. Check the interface under high magnification under the laser. A light pipe, with the laser microscope light off, can help highlight debris. Significant debris, especially if located in the visual axis, should be removed. Minor amounts are often difficult to remove and may be left in place.
Check the patient at the slit lamp. Bring the patient back under the laser microscope to remove significant interface debris as needed.
Debris near the edge of the flap that is seen at the slit lamp can be removed with a fine spatula.
EPITHELIAL LOOSENING OR DEFECT
The microkeratome pass can cause the epithelium to loosen, dislodge, or even slough. The management of this problem begins with the preoperative recognition of predisposing factors, the choice of equipment designed to minimize these problems, proper intraoperative management of the corneal surface, and postoperative care. One key to intraoperative management is identifying the abnormality to be at the level of the corneal epithelium and not the flap interface.
Predisposing Factors
Epithelial basement membrane (EBM) dystrophy. One of the most common risk factors for epithelial problems during and after LASIK is EBM dystrophy.
Recurrent erosion history. A history of recurrent erosions should alert the surgeon that the patient probably has corneal epithelial adhesion problems and may be at risk for such difficulties during and after LASIK.
Older patient (≥45 years). Several studies have demonstrated older age to be a risk factor for epithelial problems with LASIK.
Poor-quality blade.
Large flap diameter.
Excessive topical anesthetic. Topical anesthetic is toxic to the epithelium. The anesthetic drop should be instilled just prior to placement of the eyelid speculum.
Pivoting microkeratome.
Prevention
Avoid LASIK in patients with excessive risk of epithelial problems.
Minimize the use of topical anesthetic.
Lubricate the eye before the microkeratome pass. The Zero Compression Head on the Hansatome has greatly reduced epithelial disruption compared to the standard head.
During femtosecond laser flap dissection, be certain the dissector is actually in the interface and not just subepithelial.
Management
If the flap stroma is normal, you can proceed with the excimer laser ablation.
Realign all loose epithelium and replace all the epithelial tags in their original position as much as possible.
Check the stromal bed carefully for epithelial fragments, which must be removed.
Consider placing a BSCL, although this may increase the risk of diffuse lamellar keratitis (DLK).
Use preservative-free lubricants frequently.
Follow closely as there is an increased risk of DLK with epithelial defects, even when they occur months or years after LASIK surgery.
If there is a large area of severe epithelial loosening or sloughing, consider debriding the abnormal epithelium and consider postponing surgery on the fellow eye. Surface ablation, if possible, would be a better choice.
LIMBAL BLEEDING
Bleeding at the edge of the flap is not uncommon. If it is anticipated and managed appropriately, the excimer laser ablation can be performed without problem.
Causes
Limbal neovascularization. It is most common in previous long-term contact lens wearers. Patients with atopic keratoconjunctivitis, acne rosacea, blepharitis, and/or meibomianitis may be left with corneal neovascularization even after the external disease has been medically controlled. The more extensive the neovascularization, the more likely bleeding is to occur. Patients with blood vessels in the ablation zone are poor candidates for LASIK surgery. Superficial vessels within the hinge will generally not bleed.
Large, peripheral flaps are associated with an increased risk of transecting peripheral blood vessels.
Decentered flaps are closer to the limbus on one side and therefore at greater risk of bleeding.
Prevention
Avoid superior flap decentration so that the flap edge will be less likely to transect the more common superior vessels.
Make a smaller flap either with a smaller diameter microkeratome ring or with smaller diameter settings using the femtosecond laser.
AVOID TOPICAL BRIMONIDINE (e.g., ALPHAGAN) as a means to constrict blood vessels. Brimonidine use can make postoperative flap dislocation more likely.
Consider using a femtosecond laser. Significant bleeding from perilimbal corneal neovascularization is much less likely when the flap is created with a femtosecond laser than when a mechanical microkeratome is used.
Management
Wait 30 to 60 seconds after the flap is made before lifting.
Place a sponge (e.g., Chayet sponge) at the edge of the flap to collect the blood before it migrates onto the stromal bed.
Direct, gentle pressure at the site of hemorrhage with a Merocel sponge can help achieve adequate hemostasis more quickly.
A drop of phenylephrine can slow the bleeding but will also dilate the pupil, which may impact excimer laser ablation centration.
It is critical to prevent the blood from reaching the ablation zone during the excimer laser treatment because it will mask the laser ablation and predispose to irregular astigmatism. Interrupt the ablation to remove accumulating blood that is entering the treatment zone. This must be done quickly to avoid excessive drying of the flap bed, which can lead to overcorrection.
Irrigate any blood from the interface at end of surgery. Blood in the interface increases the risk of DLK.
POORLY ADHERENT FLAP
A poorly adherent flap noted immediately after surgery is more likely to become displaced postoperatively. It is wise to make sure the flap is well aligned and in stable position prior to the patient leaving the laser center.
Causes
Overhydration of the flap. Excessive irrigation of the flap interface and lifting and replacing the flap multiple times increases flap hydration and can lead to poor adherence.
Trauma to the flap from the eyelid speculum. During speculum removal the flap can be displaced, requiring careful repositioning. Care should be taken to lift the eyelid speculum away from the cornea during removal to prevent hitting the flap.
Endothelial dysfunction (e.g., Fuchs’ corneal dystrophy). Reduced endothelial pump function may decrease flap adherence. A thick cornea, central pachymetry ≥650 µm, noted preoperatively should prompt a further evaluation with specular microscopy to rule out a low endothelial cell count. A thick cornea due to endothelial dysfunction may result in postoperative flap instability after LASIK surgery.
Prevention
Keep the flap irrigation and manipulation to a minimum.
Remove the eyelash drapes and eyelid speculum very carefully, avoiding contact with the flap edge.
Avoid topical Brimonidine, which can increase the risk of flap displacement.
Avoid LASIK in patients with endothelial dysfunction.
Some feel that the femtosecond laser with its ability to create a more perpendicular side cut or even a reverse bevel cut (see Fig. 5.1) makes flaps that are more resistant to flap displacement.
Management
Let the flap “dry” in good position for a few minutes prior to carefully removing the eyelid speculum.
Consider placing a BSCL on the eye if the flap does not appear secure.
Insist that the patient wear protective glasses and nighttime goggles postoperatively and avoid touching or rubbing the eyes.
Instruct patient on safe eyedrop instillation.
▪ Postoperative Complications
Complications that usually occur soon after surgery include a displaced flap, infection, DLK, central toxic keratopathy, and flap striae. Other complications that occur later include dry eye syndrome/neurotrophic keratopathy, epithelial ingrowth, pressure-induced stromal keratitis (PISK), pressure-induced interface fluid, and ectasia. Postoperative vision complaints that may be considered complications by patients include poor unaided visual acuity due to inadequate correction of refractive error or regression of refractive effect; poor night vision due to glare, haloes, or decreased contrast sensitivity; photophobia; and ghosting. Refer to Chapter 10 for a more detailed discussion of the management of patients with these complaints.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree