Fig. 10.1
(a) The femtosecond laser is focused to the target area within the corneal stroma. Microplasma is created, vaporizing approximately 1 μm of corneal tissue. (b) A bubble of gas and water forms around each pulse. (c–e) Repeated applications allow gas bubbles to coalescence along a single plane, creating a “cut”
10.2 Femtosecond Lasers in Ophthalmology
In the early 1990s, Ronald Kurtz, MD, in collaboration with Tibor Juhasz, PhD, and their associates designed and constructed the prototype of the ophthalmic femtosecond laser system that later became the IntraLase system (Abbott Medical Optics (AMO), Santa Ana, CA). In 2005 the US Food and Drug Administration cleared the use of the femtosecond laser (AMO, Santa Ana, California) for laser-enabled full- and partial-thickness corneal incisions, which was rapidly followed by patient treatments at UC Irvine and elsewhere (Ignacio et al. 2006; Steinert et al. 2007). Currently, the new 6th-generation IntraLase iFS system is in use and allows for significantly faster laser cutting time with lower pulse energies. Several other FS laser platforms have also been modified for laser-enabled keratoplasty including the VisuMax (Carl Zeiss Meditec AG, Jena, Germany) and FEMTO LDV (Ziemer Ophthalmic Systems AG, Port, Switzerland) and the FEMTEC (Bausch & Lomb and 20/10 Perfect Vision, Heidelberg, Germany). The author’s experience has been with the IntraLase platform; therefore, this platform will serve as the basis for this manuscript. The fundamental aspects, however, are similar among the available platforms.
10.3 The Femtosecond Laser-Enabled Keratoplasty (FLEK)
The femtosecond laser allows for exact, reproducible and customized trephination patterns on both the donor and host tissues. The “top-hat” button configuration was the first customized trephination pattern using the FS laser (Fig. 10.2a). We have previously demonstrated that the “top-hat” shape leads to increased wound stability, increase in resistance to leakage, and possibly less astigmatism than traditional trephination PKP wounds (Steinert et al. 2007; Farid et al. 2007). Since then, a variety of other complex patterns of laser trephination cuts have been described, including “mushroom,” “zigzag,” and “Christmas tree” patterns (Fig. 10.2a–d). The “top-hat”–shaped cut replaces greater endothelial cells and may be beneficial in endothelial diseases such as Fuchs’ dystrophy as well as creating an internal flange to help seal the wound. In diseases involving primarily the anterior and stromal cornea such as keratoconus or stromal pathologies, the “mushroom” cut may be more advantageous by providing a greater anterior stromal replacement. The “zigzag” cut pattern, however, works well in virtually all settings with an angled anterior side cut that facilitates donor-host interface alignment, potentially decreasing tissue misalignment, and results in less optical distortion. Furthermore, the “zigzag” configuration has the simplest learning curve for suturing. Where precise care has to be taken to place the suture through the posterior wing of the top-hat cut to prevent posterior tissue separation postoperatively (Fig. 10.3), in the “zigzag” incision pattern, the needle needs to be passed at the easily visualized lamellar tissue apex and then inserted into the corresponding host lamellar space in order to achieve excellent wound apposition (Fig. 10.4). Improved sealing of the incision site permits the surgeon to use less suture tension than traditional keratoplasty, reducing distortion from tight or multiple sutures. In addition, the increased surface area of these incisions leads to improved tensile strength of the wound, allowing for earlier suture removal when indicated (Farid et al. 2009; Buratto and Böhm 2007; Price and Price 2008; Cheng et al. 2008b; Bahar et al. 2009). Lastly, FLEK has been shown to have rapid visual recovery and astigmatism comparable to or often better than traditional blade trephination (Farid et al. 2009; Buratto and Böhm 2007; Price and Price 2008; Cheng et al. 2008b; Bahar et al. 2009).
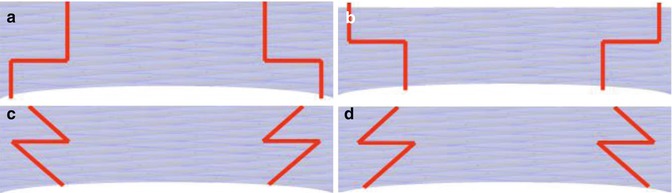
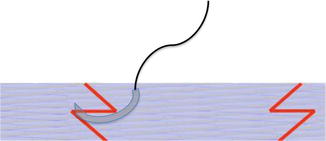
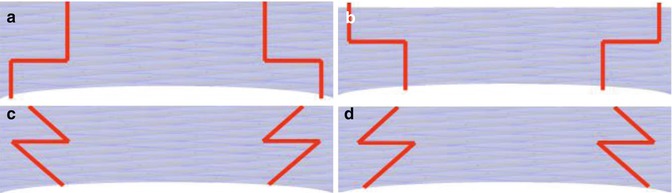
Fig. 10.2
(a) “Top-hat” configuration. (b) “Mushroom” configuration. (c) “Zigzag” configuration. (d) “Christmas tree” configuration
Fig. 10.3
Incorrect placement of suture in “top-hat” incision can lead to posterior wound gape
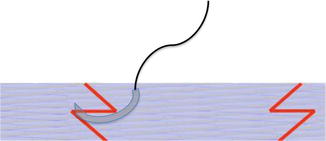
Fig. 10.4
Correct placement of needle at apex of “zigzag” incision
10.4 Patient Selection and Evaluation
Successful postsurgical FLEK outcome is crucially dependent on proper patient selection. Initially, contraindications to the procedure should carefully be excluded: any condition preventing proper laser docking such as severe ocular surface irregularity, elevated glaucoma filtering bleb or glaucoma shunt implant, small orbits, extremely narrow palpebral fissures, and recent corneal perforations. Extreme caution should be utilized if the decision is made to perform FLEK on patients with prior penetrating keratoplasty or globe trauma because of the risk of corneal/globe rupture. Interestingly, a small retrospective case series by Rush et al. did not show any rupture of old corneal wounds with the significant rise in intraocular pressure associated with laser applanation in patients with previous corneal grafts or globe trauma using the IntraLase platform (Rush et al. 2011). Although the FS laser is known to have excellent cut penetration through even dense scars, severe peripheral corneal neovascularization and/or opacity may be a relative contraindication.
10.5 Tissue Preparation and Surgical Procedure
Several donor configurations are available for the zigzag button arrangement, each with a specific diameter [8.0 mm (“zigzag” A), 8.5 mm (“zigzag” B), and 9.0 mm (“zigzag” C)]. It is our customary practice to have the donor tissue supplied pre-cut from the eye bank. The eye bank uses the surgeon-specified laser parameters to compliment the planned surgery (i.e., “zigzag” C donor into a “zigzag” C host). Alternatively, laser cutting of donor tissue can be accomplished using an artificial anterior chamber with the same laser where the host tissue is cut. For the majority of patients, we use a same-size donor and host trephination; however, if the preoperative keratometry readings are very steep, the surgeon can consider undersizing the graft by one (i.e., “zigzag” B donor into “zigzag” C). Host cutting can be done under topical or retrobulbar anesthesia. Centration of the suction ring on the patient’s eye is crucial to achieving centration of the graft. Complex cutting patterns and alignment marks can increase the amount of time the suction ring remains on the eye, thereby favoring preoperative retrobulbar block for patient comfort; however, this has become less significant with the newer, faster generation of femtosecond lasers. Conditions that may complicate host laser cutting such as nystagmus, dementia, excessive anxiety, and children should be offered general anesthesia to ensure safety and success of the procedure; however, this requires coordinated care with anesthesia to provide portable monitoring and anesthesia. Additionally, having the femtosecond laser either in the operating suite or in close proximity to the operating suite allows for FLEK in these unique situations.
The “zigzag” cut results in three distinct cuts that can be readily visualized on postoperative slit lamp biomicroscopy and anterior segment OCT imaging (Figs. 10.5a, b). The femtosecond laser also allows for the placement of radial alignment marks on the host and donor, which facilitate precise suture placement and improved tissue distribution.
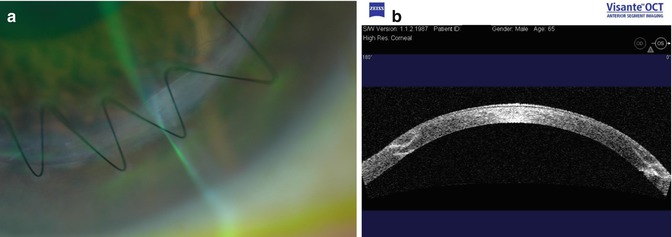
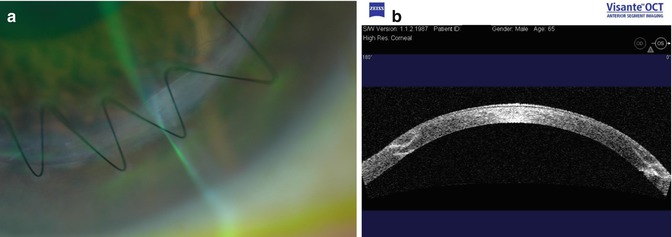
Fig. 10.5
(a) Slit lamp photo of “zigzag” incision. (b) Anterior segment OCT of “zigzag” incision
It is our customary procedure to leave a 70 μm posterior layer of uncut tissue to maintain a closed eye and formed anterior chamber between laser cut and cap removal. Preoperative pachymetry mapping, obtained either by anterior segment optical coherence tomography (Visante OCT, Carl Zeiss Meditec, Inc., Dublin, California), Scheimpflug photography (Pentacam, Oculus USA, Lynwood, Washington), or ultrasound is necessary to determine the posterior incision depth limit. Studies have demonstrated that side-cut bridges are stronger than lamellar bridges; however, both types of tissue bridges are stronger than full-thickness cuts (Price et al. 2008; Heur et al. 2011). For easier detection and potential graft-host alignment issues, a posterior side-cut bridge is preferred over an anterior side-cut bridge.
After the femtosecond laser incision is complete, antibiotic drops are placed in the eye, and the eye is shielded; if the laser is located another surgical room, the patient transported to the operating suite. The host corneal button can be bluntly dissected (i.e., with a Sinskey hook) to reveal the lamellar and side-cut laser incisions. These incisions usually separate cleanly, although limited sharp dissection with a surgical blade or scissors may be needed. Next, the anterior chamber is then entered with a blade and the posterior corneal bridging tissue is cut with corneal scissors. Care should be taken to create a posterior lip of host tissue to aid in a hermetic seal. The donor cornea is sutured into place using the surgeon’s suturing pattern of choice. The depth of the suture in the donor and host tissue should be carefully aligned in order to minimize misalignment and tissue distortion (Heur et al. 2011) (Fig. 10.4).
10.6 Literature Review of Femtosecond Keratoplasty
10.6.1 FLEK
FLEK has been shown to have equal or better best spectacle corrected visual acuity (BSCVA) and postoperative astigmatism, when compared to conventional PK. Farid et al., in their preliminary study of 13 patients with femtosecond laser-generated “zigzag” incision configuration, showed over a 9-month period the mean astigmatism to be less than 3.0 diopters at all intervals beginning as early as the first postoperative month (Farid et al. 2007). A larger follow-up study showed that the femtosecond laser generated “zigzag”–shaped incision results in a more rapid recovery of BSCVA and induces less astigmatism as compared to conventional blade trephination PKP with 81 % of the “zigzag” group versus 45 % of the conventional Barron suction trephination group achieved BSCVA of ≥20/40 by postoperative month 3 in patients with good visual potential (Farid et al. 2009). In addition, Chamberlain et al. compared 50 patients with “zigzag” FLEK to 50 patients with conventional PKP and reported statistically significant improvement in astigmatism in the FLEK group in the first 6 postoperative months and earlier suture removal in the FLEK group, however, without significantly improved BCSVA (Chamberlain et al. 2011). The low levels of astigmatism is proving to be stable even after all sutures are removed up to 5 years after the procedure (Wade et al. unpublished data, ASCRS annual meeting abstract 2013). In patients with keratoconus, Gaster et al. found that patients treated with “zigzag” FLEK achieved better BCSVA, lower topographic astigmatism, and earlier suture removal at all time points than patients treated with conventional PKP, but this was only statistically significant at 3 and not at the 6 month end point of the study (Gaster et al. 2012).
In a non-randomized study comparing “top-hat” configuration FLEK with manual trephinated top-hat PKP, Bahar et al. showed that femtosecond “top-hat” PKPs had higher endothelial cell counts and underwent faster suture removal times compared to manual “top-hat” trephination PKPs. Further, the “top-hat” FLEK group had less astigmatism and better BSCVA in comparison to the manual “top-hat” PKPs after 12 months of follow-up (Bahar et al. 2009).
Of note, Chamberlain et al. reported statistically greater posterior surface HOAs in DSAEK than FLEK or PKP, although the differences in anterior surface higher-order aberrations among the full-thickness grafts were not statistically significant but showed a trend of lower HOAs in the FLEK group (Chamberlain et al. 2012).
Traditional penetrating keratoplasty has certainly shown its great efficacy over the last decades. Nonetheless, FLEK continues to prove to be as effective or perhaps advantageous procedure. Studies continue to show that FLEK results in excellent visual acuity and reduced astigmatism which are comparable or improve on conventional trephination PK (Steinert et al. 2007; Farid et al. 2007, 2009; Buratto and Böhm 2007; Price and Price 2008; Cheng et al. 2008b; Bahar et al. 2009; Tan and Heng 2013; Birnbaum et al. 2013; Mootha et al. 2011).
10.6.2 Femtosecond Laser-Enabled Lamellar Keratoplasty
Just as the FS laser has revolutionized penetrating keratoplasty, the FS laser is being used to facilitate lamellar keratoplasty including deep anterior lamellar keratoplasty (DALK), anterior lamellar keratoplasty (ALK), and Descemet’s stripping automated endothelial keratoplasty (DSAEK). As the laser platforms improve, the complexity and reliability of stromal cuts continue to improve. Interestingly, when donor tissue is processed for DSAEK, manual trephination may currently be superior to using the femtosecond laser alone or when utilizing a combination of both manual and laser technique (Rosa et al. 2013; Vetter et al. 2013; Murta et al. 2013; Mootha et al. 2011; Farid and Steinert 2009). Nonetheless, as femtosecond technology adapts to endothelial keratoplasties, the femtosecond platform continues to hold great promise with these types of transplants.
10.6.3 Deep Anterior Lamellar Keratoplasty
DALK is the ideal procedure for ectatic diseases of the cornea in which the endothelium is normal, such as keratoconus. Farid and Price independently first described the “zigzag” DALK (Farid and Steinert 2009; Price et al. 2009). The “zigzag” FS laser incision is combined with the big-bubble technique to aid in baring of Descemet’s membrane from the rest of the corneal stroma and perform a deep anterior lamellar transplant, combined with the FS laser incision benefits. The posterior cut begins at a depth of 50–100 μm anterior to the endothelium and defines a starting point for needle insertion and big-bubble dissection. In the event of Descemet’s rupture during dissection, conversion to a full-thickness transplant can be done while maintaining the benefits of the femtosecond laser incision (Price et al. 2009; Buzzonetti et al. 2010a). An alternate application using the femtosecond laser was described by Buzzonetti et al. (2012). In this technique, a channel to the posterior stroma, 50 μm above the endothelium, can be created using the FS laser. A blunt cannula can then be passed through the channel, minimizing risk of Descemet’s perforation, to facilitate big-bubble dissection at the proper corneal plane (Buzzonetti et al. 2012). FS DALK, although a novel technique, is beginning to prove to be an efficacious for treating stromal pathologies providing promising visual acuity and astigmatic postoperative outcomes (Price et al. 2009; Buzzonetti et al. 2010a, 2012; Cheng et al. 2008b; Shehadeh-Mashor et al. 2013; Yoo et al. 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


